Chapter: Basic & Clinical Pharmacology : Sedative-Hypnotic Drugs
Treatment of Sleep Problems
TREATMENT OF SLEEP PROBLEMS
Sleep
disorders are common and often result from inadequate treat-ment of underlying
medical conditions or psychiatric illness. True primary insomnia is rare.
Nonpharmacologic therapies that are useful for sleep problems include proper
diet and exercise, avoiding stimu-lants before retiring, ensuring a comfortable
sleeping environment, and retiring at a regular time each night. In some cases,
however, the patient will need and should be given a sedative-hypnotic for a
limited period. It should be noted that the abrupt discontinuance of many drugs
in this class can lead to rebound insomnia.
Benzodiazepines
can cause a dose-dependent decrease in both REM and slow-wave sleep, though to
a lesser extent than the barbiturates. The newer hypnotics zolpidem, zaleplon,
and eszopiclone are less likely than the benzodiazepines to change sleep
patterns. However, so little is known about the clinical impact of these
effects that statements about the desirability of a particular drug based on
its effects on sleep architecture have more theoretical than practical significance.
Clinical criteria of efficacy in alleviating a particular sleeping problem are
more useful. The drug selected should be one that provides sleep of fairly
rapid onset (decreased sleep latency) and sufficient duration, with minimal
“hangover” effects such as drowsiness, dysphoria, and mental or motor
depression the following day. Older drugs such as chloral hydrate,
secobarbital, and pentobar-bital continue to be used occasionally, but
zolpidem, zaleplon, eszopiclone, or benzodiazepines are generally preferred.
Daytime sedation is more common with benzodiazepines that have slow elimination
rates (eg, lorazepam) and those that are biotrans-formed to active metabolites
(eg, flurazepam, quazepam). If benzodiazepines are used nightly, tolerance can
occur, which may lead to dose increases by the patient to produce the desired
effect. Anterograde amnesia occurs to some degree with all ben-zodiazepines
used for hypnosis.
Eszopiclone,
zaleplon, and zolpidem have efficacies similar to those of the hypnotic benzodiazepines
in the management of sleep disorders. Favorable clinical features of zolpidem
and the other newer hypnotics include rapid onset of activity and mod-est
day-after psychomotor depression with few amnestic effects. Zolpidem, one of
the most frequently prescribed hypnotic drugs in the United States, is
available in a biphasic release formulation that provides sustained drug levels
for sleep main-tenance. Zaleplon acts rapidly, and because of its short
half-life, the drug has value in the management of patients who awaken early in
the sleep cycle. At recommended doses, zaleplon andeszopiclone (despite its
relatively long half-life) appear to cause less amnesia or day-after somnolence
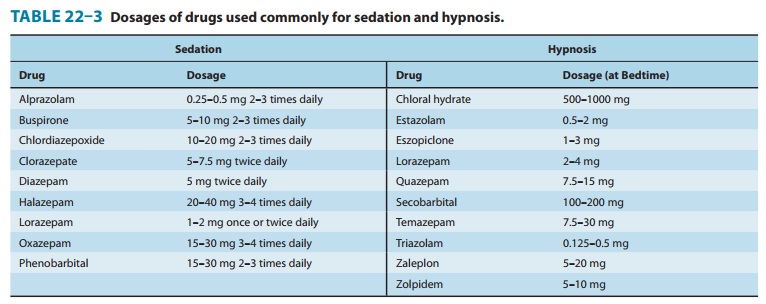
than zolpidem or benzo-diazepines. The drugs in this class commonly used for
sedation and hypnosis are listed in Table 22–3 together with recom-mended
doses.
Note: The failure of insomnia to remit after 7–10
days of treat-ment may indicate the presence of a primary psychiatric or
medi-cal illness that should be evaluated. Long-term use of hypnotics is an
irrational and dangerous medical practice.
Related Topics