Chapter: Ophthalmology: Eye Lens
Treatment of Cataracts
Treatment of Cataracts
Medical Treatment
In spite of theoretical approaches in animal
research, the effectiveness of con-servative cataract treatment in humans has
not been demonstrated.
At present there are no available conservative
methods to prevent, delay, or reverse the development of a cataract.
Galactosemic cataracts are the only exception to this rule.
Surgical Treatment
Cataract surgery is the most frequently
performed procedure in ophthal-mology.
When is surgery indicated?
Earlier surgical techniques were dependent
upon the maturity of the cataract.
This is no longer the case in modern cataract
surgery.
❖ In the presence of bilateral cataracts, the eye with the worse visual acuity should undergo surgery
when the patient feels visually handicapped.However, this threshold will vary
depending on the patient’s occupational requirements.
❖ In the presence of a unilateral cataract, the patient is often inclined to postpone surgery as long as
vision in the healthy eye is sufficient.
❖ In the presence of a mature cataract, it is important to advise the patient to undergo surgery as
soon as possible.
Will the operation be successful?
The prospect of a successful outcome is
important for the patient. Most patients define a successful outcome in terms
of a significant improvement in vision. Therefore, it is important that the
patient undergoes a thorough pre-operative eye examination to exclude any
ocular disorders, aside from the cataract, that may worsen visual acuity and compromise
the success of the cataract operation. Such disorders include uncontrolled
glaucoma, uveitis, macular degeneration, retinal detachment, atrophy of the
optic nerve, and amblyopia.
A detailed history of the patient’s other
ocular disorders and vision prior to development of the cataract should be
obtained before surgery.
Several methods aid in making a prognosis with respect to expected visualacuity (retinal resolution) following cataract
surgery. These include:
❖ Retinoscopy to determine visual acuity.
❖ Evaluation of the choroid figure (in severe opacifications such as a maturecataract).
Reliability of cataract surgery
Cataract surgery is now performed as a
microsurgical technique under an operating microscope. Modern techniques,
microsurgical instruments, atrau-matic suture material (30 µm thin nylon suture thread), and specially trained surgeons have
made it possible to successfully perform cataract surgery without serious complications in 98% of all patients. The procedure
lasts about30 minutes and, like the postoperative phase, is painless.
Duration of hospitalization
The patient may be hospitalized for 3 days, depending on the adequacy of postoperative
care at home. Older patients who live alone may be unable to care adequately
for themselves and maintain the regime of prescribed medi-cations for the
operated eye in the immediate postoperative phase. The operation may be performed as an outpatient procedure
if the ophthalmolo-gist’s practice is able to ensure adequate care.
Possible types of anesthesia
Cataract extraction may be performed under local anesthesia or generalanesthesia. Today, most operations are performed under local
anesthesia.Aside from the patient’s wishes, there are medical reasons for
preferring one form of anesthesia over another:
General anesthesia: This is recommended for patients who are extremelyapprehensive
and nervous, deaf, or mentally retarded; it is also indicated for patients with
Parkinson’s disease or rheumatism, who are unable to lie still without pain.
Local anesthesia (retrobulbar, peribulbar, or topical anesthesia): This is
rec-ommended for patients with increased anesthesia risks.
Preoperative consultation regarding options for achieving
refractive correction (Table 7.4)
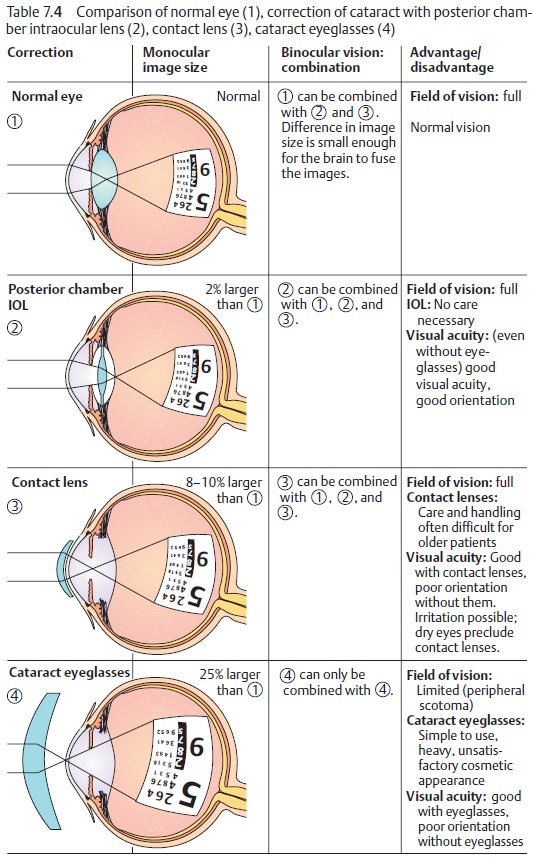
Intraocular lens: In 95 – 98% of all cataract extractions, an intraocular
lens(IOL) is implanted in place of the natural lens (posterior chamber lens). An eye with an artificial lens is referred
to as a pseudophakia. The power of
the lens required is determined preoperatively by biometry. The IOL refractive
power is determined by ultrasonic measurement of axis length, IOL refraction
con-stants, and the refractive power of the cornea. There are two types of
intraocular lenses:
❖ Monofocal IOLs.The patient can select whether the strength of the artifi-cial
lens is suitable for distance vision or near vision.
❖ Bifocal or multifocal IOLs.These allow close and remote objects to appearin focus. However,
it should be noted that bifocal and multifocal lenses do not achieve the
optical imaging quality of monofocal lenses.
Cataract eyeglasses: The development of the intraocular lens has largelysupplanted
correction of postoperative aphakia with cataract lenses. Long the standard,
this method is now only necessary in
exceptional cases. Cataract eye-glasses cannot be used for correcting unilateral aphakia because the
differ-ence in the size of the retinal images is too great (aniseikonia).
Therefore, cat-aract eyeglasses are only suitable for correcting bilateral aphakia. Cataract eyeglasses
have the disadvantage of limiting the field of vision (peripheral and ring scotoma).
Contact lenses (soft, rigid, and oxygen-permeable): These lenses permit anear normal field of vision and are suitable for postoperative correction of uni-lateral cataracts as the difference in image size is negligible. However, manyolder patients have difficulty learning how to cope with contact lenses.
Surgical Techniques
The operation is performed on only one eye at
a time. The procedure on the fellow eye is performed after about a week if once
the first eye has stabilized.
Historical milestones:
❖Couching(reclination): For 2000 years until the 19 th century, a
pointedinstrument was used to displace the lens into the vitreous body out of
the visual axis.
❖ 1746: J. Daviel performed the first extracapsular
cataract extraction byremoving the contents of the lens through an inferior
approach.
❖ 1866: A. von Graefe performed the first removal of a cataract through
a superior limbal incision with capsulotomy.
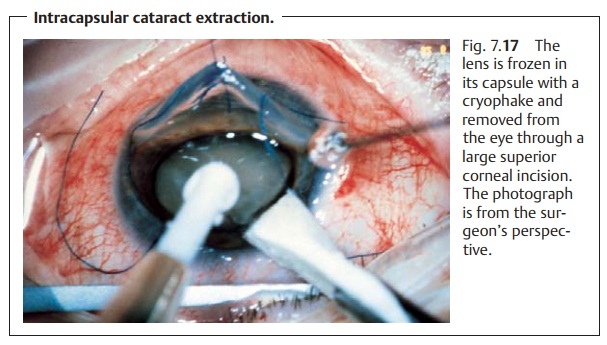
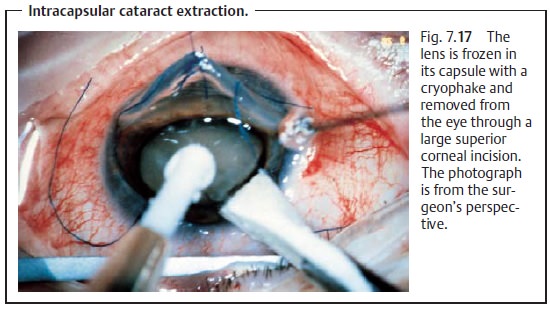
Intracapsular cataract extraction: Until the mid 1980s, this was the method ofchoice. Today intracapsular cataract extraction is
used only with subluxationor dislocation of the lens. The entire lens is frozen
in its capsule with a cryo-phake and removed from the eye through a large
superior corneal incision (Fig. 7.17).
Extracapsular cataract extraction: Procedure(Figs. 7.18a – c): The anteriorcapsule is opened (capsulorrhexis). Then only the
cortex and nucleus of the lens are removed (extracapsular extraction); the
posterior capsule and zonule suspension remain intact. This provides a stable
base for implanta-tion of the posterior chamber intraocular lens.
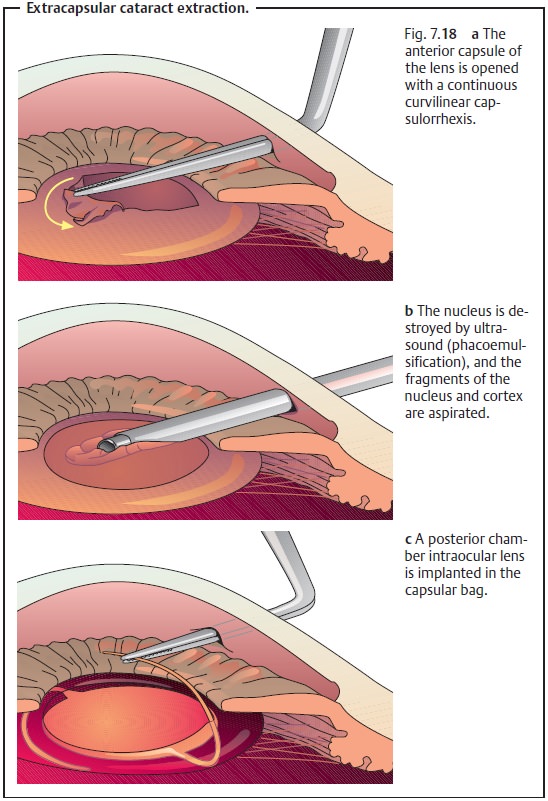
Extracapsular cataract extraction with implantation of a posterior chamber intraocular lens is now the method of choice.
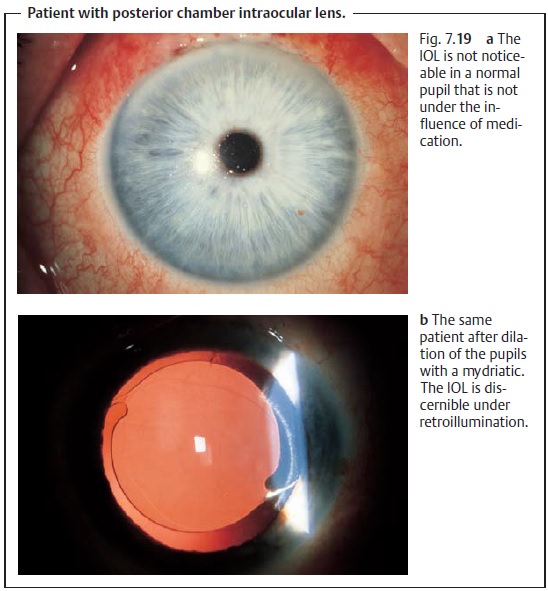
Today phacoemulsification (emulsifying and aspirating the nucleus of the lens with a high-frequency ultrasonic needle) is the preferred technique for removing the nucleus. Where the nucleus is very hard, the entire nucleus is expressed or aspirated. Then the softer portions of the cortex are removed by suction with an aspirator/irrigator attachment in an aspiration/irrigation maneuver. The posterior capsule is then polished, and an intraocular lens (IOL) is implanted in the empty capsular bag (Fig. 7.19a and b). Phacoemulsi-fication and IOL implantation require an incision only 3 – 6 mm in length. Where a tunnel technique is used to make this incision, no suture will be nec-essary as the wound will close itself.
Advantages over intracapsular cataract extraction.Extracapsular cataractextraction usually does
not achieve the same broad exposure of the retina that intracapsular cataract
extraction does, particularly where a secondary cataract is present. However,
the extracapsular cataract extraction maintains the integrity of the anterior
and posterior chambers of the eye, and the vit-reous body cannot prolapse
anteriorly as after intracapsular cataract extrac-tion. At 0.1 – 0.2%, the
incidence of retinal detachment after extracapsular cat-aract extraction is
about ten times less than after intracapsular cataract extraction, which has an
incidence of 2 – 3%.
Secondary Cataract
Epidemiology: Approximately 30% of all cataract patients develop a second-ary
cataract after extracapsular cataract extraction.
Etiology: Extracapsular cataract extraction removes only the anterior
centralportion of the capsule and leaves epithelial cells of the lens intact
along with remnants of the capsule. These epithelial cells are capable of
reproducing and can produce a secondary cataract of fibrous or regenerative
tissue in the pos-terior capsule that diminishes visual acuity (Fig. 7.20a).
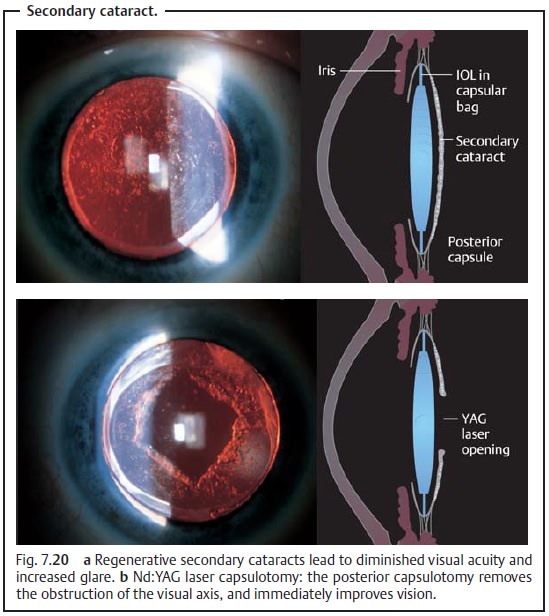
Treatment: A neodymium:yttrium-aluminum-garnet (Nd:YAG) laser canincise the
posterior capsule in the visual axis without requiring invasive eye surgery.
This immediately improves vision (Fig. 7.20b).
Special Considerations in Cataract Surgery in Children
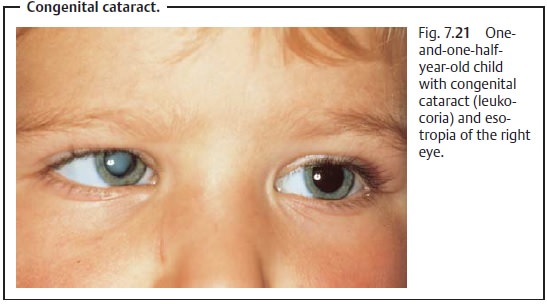
Observe changes in the child’s behavior: Children with congenital, trau-matic, or
metabolic cataract will not necessarily communicate their visual impairment
verbally. However, it can be diagnosed from these symptoms:
❖ Leukocoria.
❖ Oculodigital phenomenon: The child presses
his or her finger against the eye or eyes because this can produce light
patterns the child finds interest-ing.
❖ Strabismus: the first sign of visual
impairment (Fig. 7.21). ❖The child cries when the normal eye is covered.
❖The child has difficulty walking or grasping. ❖Erratic eye movement is present.
❖ Nystagmus.
Operate as early as possible: Retinal fixation and cortical visual responsesdevelop within the first six months of life. This means that children who undergo surgery after the age of one year have significantly poorer chances of developing normal vision.
Children with congenital cataract should
undergo surgery as early as possible to avoid amblyopia. The prognosis for
successful surgery is less favorable for unilateral
cataracts than for bilateral cataracts. This is because the amblyopia of
the cataract eye puts it at an irreversible disadvantage in comparison with the
fellow eye as the child learns how to see.
Plan for the future when performing surgery: After opening the extremelyelastic anterior lens capsule, one can aspirate the soft infantile cortex and nucleus. Secondary cataracts are frequent complications in infants.
Therefore, the procedure
should include a posterior capsulotomy
with anterior vit-rectomy to ensure an unobstructed visual axis. The
operation preserves the equatorial
portions of the capsule to permit subsequent implantation of a pos-terior
chamber intraocular lens in later years.
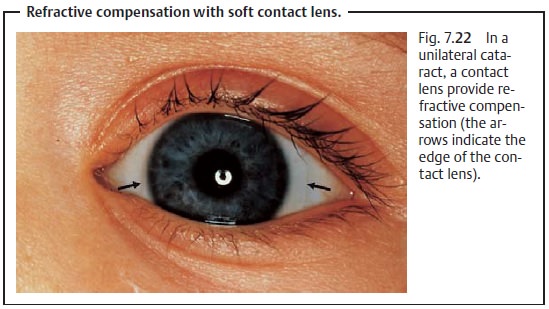
Refraction changes constantly: The refractive power of the eye changesdramatically within a
short period of time as the eye grows. The refraction in the eye of a newborn
is 30 – 35 diopters and drops to 15 – 25 diopters within the first year of
life. Refractive compensation for a unilateral
cataract is achieved with a soft
contact lens (Fig. 7.22). The
use of soft contact lenses in infants is difficult and requires the parents’
intensive cooperation. Refractive correction of bilateral cataracts is achieved with cataract eyeglasses.
Refraction should be evaluated by
retinoscopy every two months during the
first year of life and every three to four months during the second year, and
contact lenses and eyeglasses should be changed accordingly.
Implantation of posterior chamber intraocular lenses for congenital cata-ract is not yet
recommended in children under three years of age. This is because experience
with the posterior chamber intraocular lens and present follow-up periods are
significantly less than the life expectancy of the children. In addition, there
is no way to adapt the refractive power of the lens to changing refraction of
the eye as the child grows.
Orthoptic postoperative therapy is required: Unilateral cataractsin partic-ular require orthoptic postoperative therapy in the operated eye to close the gap with respect to the normal fellow eye. Regular evaluation of retinal fixation is indicated, as is amblyopia treatment (see patching).
Related Topics