Chapter: Ophthalmology: Eye Lens
Acquired Cataract : Senile Cataract
Acquired Cataract
Senile Cataract
Epidemiology:
Senile cataract is by far the most frequent form of
cataract,accounting for 90% of all cataracts. About 5% of all 70-year-olds and
10% of all 80-year-olds suffer from a cataract requiring surgery.
Ninety percent of all cataracts are senile
cataracts.
Etiology:
The precise causes of senile cataract have not been identified.
Asoccurrence is often familial, it is important to obtain a detailed family
history.
Classification and forms of senile cataracts:
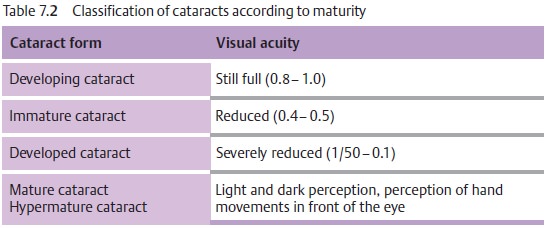
The classification according tomaturity (Table 7.2) follows the degree of visual impairment and the matur-ity, which
earlier was important to determine the time of surgery. We follow a morphologic classification as
morphologic aspects such as the hardness andthickness of the nucleus now
influence the surgical procedure (Table 7.3):
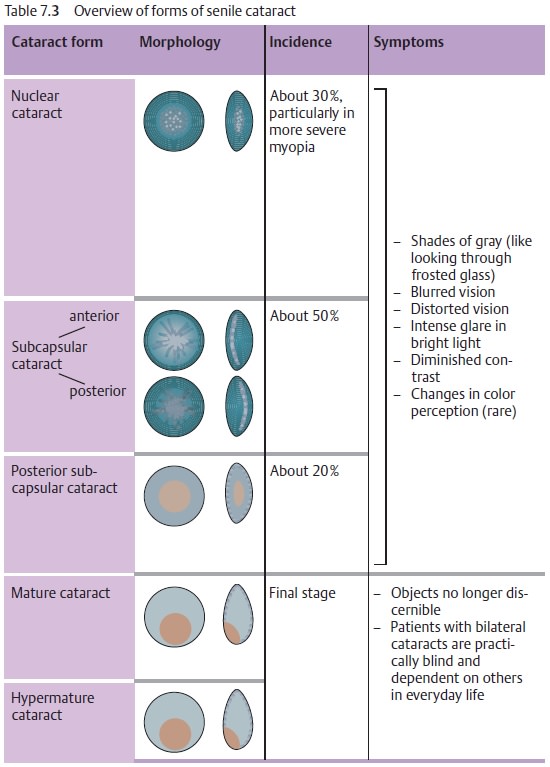
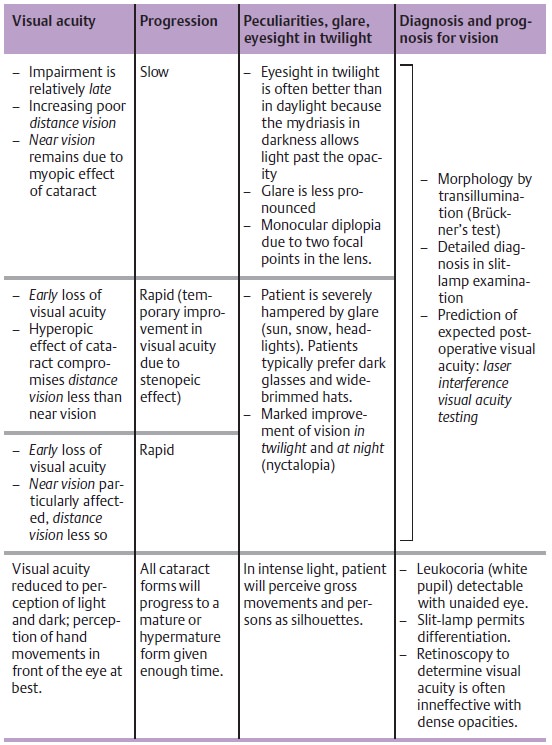
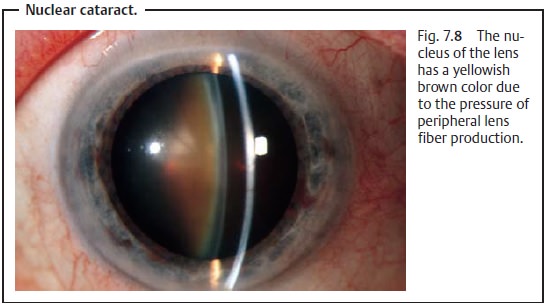
Nuclear cataract.In the fourth decade of life, the pressure of peripheral
lensfiber production causes hardening of the entire lens, especially the
nucleus. The nucleus takes on a yellowish
brown color (brunescent nuclear cataract). This may range from reddish
brown to nearly black discoloration of the entire lens (black cataract).
Because they increase the refractive power of the lens, nuclear cataracts lead
to lenticular myopia and occasionally produce a second focal point in the lens
with resulting monocular diplopia (Fig. 7.8).
Nuclear cataracts develop very slowly. Due to
the lenticular myopia, near vision (even without eyeglasses) remains good for a
long time.
Cortical cataract.Nuclear cataracts are often associated with changes in thelens cortex. It is interesting to note that patients with cortical cataracts tend to have acquired hyperopia in contrast to patients with nuclear cataracts, who tend to be myopic (see above).
Whereas changes in nuclear cataracts are due to hardening, cortical changes are characterized by increased water content. Several morphologic changes will be
apparent upon slit-lamp examination with maximum mydri-asis:
❖ Vacuoles: Fluid accumulations will be present in the form of small
narrowcortical vesicles. The vacuoles remain small and increase in number.
❖ Water Fissures: Radial patterns of fluid-filled fissures will be seen
betweenthe fibers.
❖ Separation of the lamellae: Not as frequent as water fissures, these consistof a zone of
fluid between the lamellae (often between the clear lamellae and the cortical
fibers).
❖ Cuneiform cataract: This is a frequent finding in which the opacitiesradiate from
the periphery of the lens like spokes of a wheel.
Cortical cataracts progress more rapidly than
nuclear cataracts. Visual acuity may temporarily improve during the course of
the disease. This is due to a stenopeic effect as light passes through a clear
area between two radial opacities.
Posterior subcapsular cataract.This is aspecial form of
cortical cataractthatbegins in the visual axis. Beginning as a small
cluster of granular opacities, this form of cataract expands peripherally in a
disk-like pattern. As opacity increases, the rest of the cortex and the nucleus
become involved (the usual spectrum of senile cataract).
Posterior subcapsular cataract leads to early,
rapid, and severe loss of visual acuity. Near vision is usually significantly
worse than distance vision (near-field miosis). Dilating eyedrops can improve
visual acuity in this form of cataract.
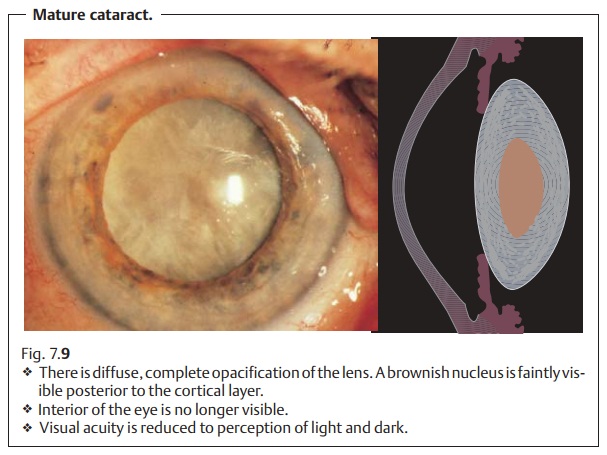
Mature cataract. The lens is diffusely white due tocomplete opacification ofthe cortex. A yellow lens nucleus is often
faintly discernible (Fig. 7.9).
Wherewater content is increased, a lens with a mature cataract can swell and
acquire a silky luster (intumescent cataract in which the capsule is under
pressure). The increasing thickness of the lens increases the resistance of the
pupil and with it the risk of angle closure glaucoma.
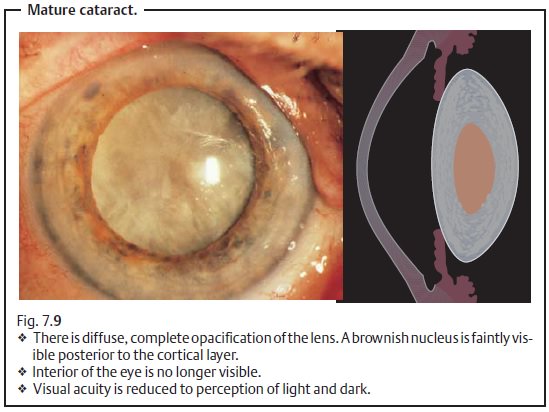
Vision is reduced to perception of light and
dark, and the interior of the eye is no longer visible. Cataract surgery is
indicated to restore visual acuity.
Hypermature cataract.If a mature cataract progresses to the point ofcomplete liquification of the cortex, the dense brown nucleus will subside within the capsule. Its superior margin will then be visible in the pupil as a dark brown silhouette against the surrounding grayish white cortex. The pressure in the lens capsule decreases. The contents of the limp and wrinkled capsular bag gravitate within the capsule. This condition, referred to as Morgagni’s cataract, is the final stage in a cataract that has usually developedover the course of two decades. The approximate onset of the cataract can usually be inferred from such findings (Figs. 7.10a and b).
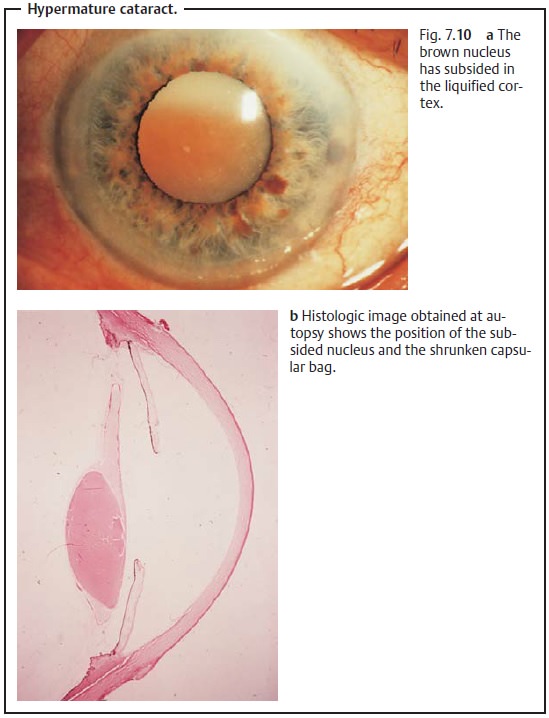
Prompt cataract extraction not only restores visual acuity but also prevents development of phacolytic glaucoma.
When the lens capsule becomes permeable for
liquified lens substances, it will lose volume due to leakage. The capsule will
become wrinkled. The escaping lens proteins will cause intraocular irritation
and attract macro-phages that then cause congestion of the trabecular network (phacolytic glau-coma: see Secondary open
angle glaucoma).
Emergency extraction of the hypermature
cataract is indicated in pha-colytic glaucoma to save the eye.
Related Topics