Chapter: Psychiatric Mental Health Nursing : Personality Disorders
Treatment - Personality Disorders
TREATMENT
Several treatment strategies are used with clients with
per-sonality disorders; these strategies are based on the disorder’s type and
severity or the amount of distress or functional impairment the client
experiences. Combinations of medica-tion and group and individual therapies are
more likely to be effective than is any single treatment (Svrakic &
Cloninger, 2005). Not all people with personality disorders seek treat-ment,
however, even when significant others urge them to do so. Typically, people
with paranoid, schizoid, schizotypal, narcissistic, and passive-aggressive
personality disorders are least likely to engage or remain in any treatment.
They see other people, rather than their own behavior, as the cause of their
problems.
Psychopharmacology
Pharmacologic treatment of clients with personality disor-ders
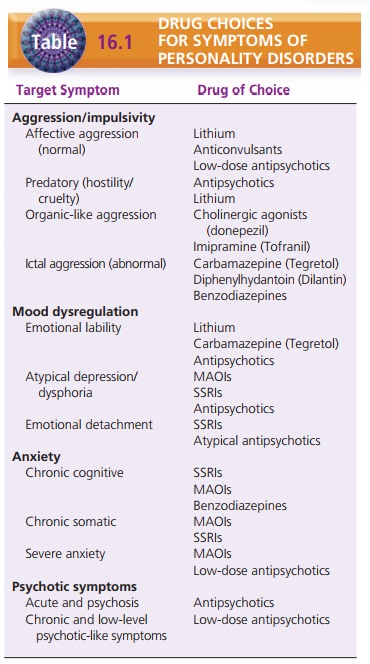
focuses on the client’s symptoms rather than the par-ticular subtype. The four
symptom categories that underlie personality disorders are cognitive–perceptual
distortions, including psychotic symptoms; affective symptoms and mood
dysregulation; aggression and behavioral dysfunc-tion; and anxiety. These four
symptom categories relate to the underlying temperaments that distinguish the DSM-IV-TR clusters of personality
disorders:
·
Low reward dependence and cluster A disorders corre-spond to the
categories of affective dysregulation, de-tachment, and cognitive disturbances.
·
High novelty seeking and cluster B disorders corre-spond to the
target symptoms of impulsiveness and aggression.
·
High harm avoidance and cluster C disorders corre-spond to the
categories of anxiety and depression symptoms.
Cognitive–perceptual disturbances include magical think-ing, odd
beliefs, illusions, suspiciousness, ideas of refer-ence, and low-grade
psychotic symptoms. These chronic symptoms usually respond to low-dose
antipsychotic medications (Simeon & Hollander, 2006).
Several types of aggression have been described in peo-ple with
personality disorders. Aggression may occur in impulsive people (some with a
normal electroencephalo-gram and some with an abnormal one); people who exhibit
predatory or cruel behavior; or people with organic-like impulsivity, poor
social judgment, and emotional lability. Lithium, anticonvulsant mood
stabilizers, and benzodiaz-epines are used most often to treat aggression.
Low-dose ![]()
![]() neuroleptics may be useful in modifying
predatory aggres-sion (Simeon & Hollander, 2006).
neuroleptics may be useful in modifying
predatory aggres-sion (Simeon & Hollander, 2006).
Mood dysregulation symptoms include emotional instability,
emotional detachment, depression, and dys-phoria. Emotional instability and
mood swings respond favorably to lithium, carbamazepine (Tegretol), val-proate
(Depakote), or low-dose neuroleptics such as haloperidol (Haldol). Emotional
detachment, cold and aloof emotions, and disinterest in social relations often
respond to selective serotonin reuptake inhibitors or atypical antipsychotics
such as risperidone (Risperdal), olanzapine (Zyprexa), and quetiapine
(Seroquel). Atypi-cal depression is often treated with selective serotonin
reuptake inhibitors, monoamine oxidase inhibitor anti-depressants, or low-dose
antipsychotic medications (Simeon & Hollander, 2006).
Anxiety seen with personality disorders may be chronic cognitive
anxiety, chronic somatic anxiety, or severe acute anxiety. Chronic cognitive
anxiety responds to selective serotonin reuptake inhibitors and monoamine
oxidase inhibitors, as does chronic somatic anxiety or anxiety manifested as
multiple physical complaints. Episodes of severe acute anxiety are best treated
with monoamine oxi-dase inhibitors or low-dose antipsychotic medications.
Table 16.1 summarizes drug choices for various target symptoms of
personality disorders. These drugs, includ-ing side effects and nursing
considerations.
Individual and Group Psychotherapy
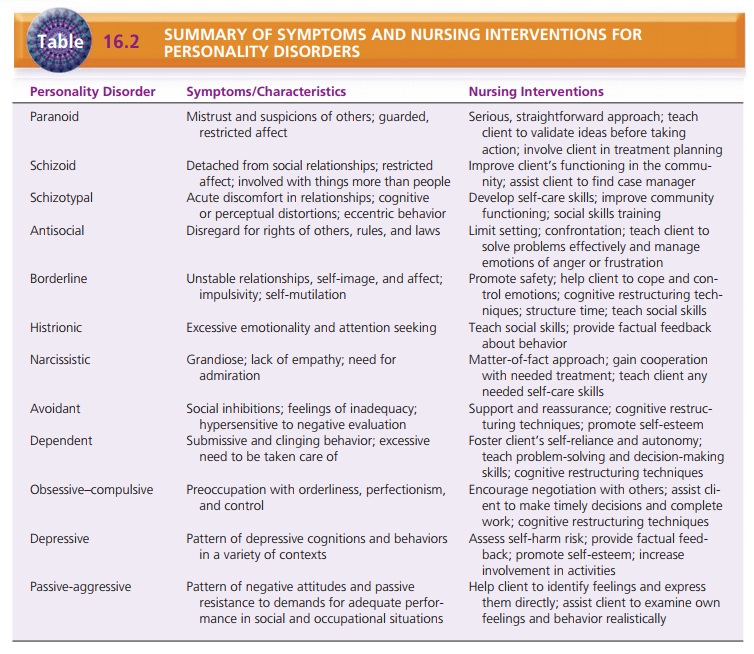
Therapy helpful to clients with personality disorders varies
according to the type and severity of symptoms and the par-ticular disorder.
Inpatient hospitalization usually is indicated when safety is a concern, for
example, when a person with borderline personality disorder has suicidal ideas
or engages in self-injury. Otherwise, hospitalization is not useful and may
even result in dependence on the hospital and staff.
Individual and group psychotherapy goals for clients with
personality disorders focus on building trust, teaching basic living skills,
providing support, decreasing distressing symptoms such as anxiety, and
improving interpersonal relationships. Relaxation or meditation techniques can
help manage anxiety for clients with cluster C personality disor-ders.
Improvement in basic living skills through the rela-tionship with a case
manager or therapist can improve the functional skills of people with schizotypal
and schizoid personality disorders. Assertiveness training groups can assist
people with dependent and passive-aggressive per-sonality disorders to have
more satisfying relationships with others and to build self-esteem.
Cognitive–behavioral therapy has been particularly helpful for
clients with personality disorders (Lynch, Trost, Salsman, & Linehan,
2007). Several cognitive restructur-ing techniques are used to change the way
the client thinks about self and others: thought stopping, in which the client
stops negative thought patterns; positive self-talk, designed to change
negative self-messages; and decatastro-phizing, which teaches the client to
view life events more realistically and not as catastrophes.
Dialectical behavior therapy was designed for clients with
borderline personality disorder (Linehan, 1993). It focuses on distorted
thinking and behavior based on the assumption that poorly regulated emotions
are the under-lying problem. Table 16.2 summarizes the symptoms of and nursing
interventions for personality disorders.
Related Topics