Chapter: Clinical Dermatology: Bullous diseases
Toxic epidermal necrolysis (LyellŌĆÖs disease)
Toxic
epidermal necrolysis (LyellŌĆÖs disease)
Cause
Toxic
epidermal necrolysis is usually a drug reaction, most commonly to sulphonamides,
barbiturates, carbamazepine or allopurinol , but can also be a manifestation of
graft-vs.-host disease. Some-times it is unexplained.
Presentation
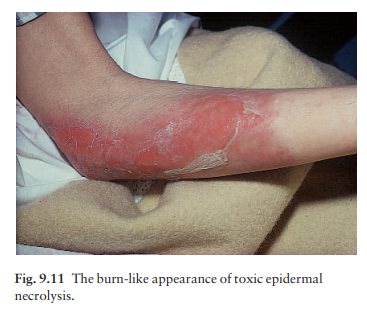
The skin becomes red and intensely painful, and then begins to come off in sheets like a scald. This leaves an eroded painful glistening surface (Fig. 9.11). NikolskyŌĆÖs sign is positive. The mucous membranes may be affected, including the mouth, eyes, and even the bronchial tree.
Course
The
condition usually clears if the offending drug is stopped. New epidermis grows
out from hair follicles so that skin grafts are not usually needed. The
dis-order may come back if the drug is taken again.
Complications
Toxic
epidermal necrolysis is a skin emergency and can be fatal. Infection, and the
loss of fluids and elec-trolytes, are life-threatening, and the painful denuded
skin surfaces make life a misery. Corneal scarring may remain when the acute
episode has settled.
Differential diagnosis
The
epidermolysis of the staphylococcal scalded skin syndrome looks like toxic epidermal necrolysis
clinically, but only the stratum corneum is lost. Whereas toxic epidermal
necrolysis affects adults, the staphy-lococcal scalded skin syndrome is seen in
infancy or early childhood. Histology differentiates the two. Pemphigus may
also look similar, but starts more slowly and is more localized. Severe
graft-vs.-host reac-tions can also cause this syndrome. Some believe that toxic
epidermal necrolysis can evolve from StevensŌĆō Johnson syndrome because some
patients have the clinical features of both.
Investigations
Biopsy
helps to confirm the diagnosis. The split is subepidermal in toxic epidermal
necrolysis, and the entire epidermis may be necrotic. A frozen section provides
a quick answer if there is genuine difficulty in separating toxic epidermal
necrolysis from the scalded skin syndrome. There are no tests to tell which
drug, if any, caused the disease.
Treatment
If
toxic epidermal necrolysis is caused by a drug, this must be stopped ;
otherwise, treatment relies mainly on symptomatic management. Intensive nursing
care and medical support are needed, includ-ing the use of central venous
lines, intravenous fluids and electrolytes. Many patients are treated in units
designed to deal with extensive thermal burns. Air suspension beds increase
comfort. The weight of opinion has turned against the use of systemic
corti-costeroids but, if they are given, it should be for short periods only,
right at the start. Intravenous IgG seems more promising.
Related Topics