Chapter: Clinical Dermatology: Bullous diseases
Pemphigoid
Subepidermal immunobullous disorders
These
can be hard to separate on clinical grounds and only the two most important,
pemphigoid and dermatitis herpetiformis, are described in detail here. Several
others are mentioned briefly.
Pemphigoid
Pemphigoid is an autoimmune disease. Serum from about 70% of patients contains antibodies that bind in vitro to normal skin at the basement membrane zone.
However,
their titre does not correlate with clinical disease activity. The IgG
antibodies bind to two main antigens: most commonly to BP230 (within the
cel-lular part of the hemidesmosome), and less often to BP180 (a transmembrane
molecule with one end within the hemidesmosome and the other bound to the
lamina lucida). Complement is then activated, an inflammatory cascade starts
and mast cells degranulate, liberating a variety of inflammatory mediators.
Presentation
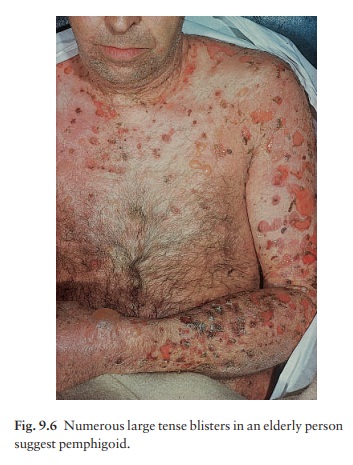
Pemphigoid
is a chronic, usually itchy, blistering dis-ease, mainly affecting the elderly.
The tense bullae can arise from normal skin but usually do so from urticarial
plaques (Fig. 9.6). The flexures are often affected; the mucous membranes
usually are not. The Nikolsky test is negative
Course
Pemphigoid is usually self-limiting and treatment can often be stopped after 1–2 years.
Complications
Untreated,
the disease causes much discomfort and loss of fluid from ruptured bullae.
Systemic steroids and immunosuppressive agents carry their usual com-plications
if used long-term. The validity of a possible association with internal
malignancy is still debated.
Differential diagnosis
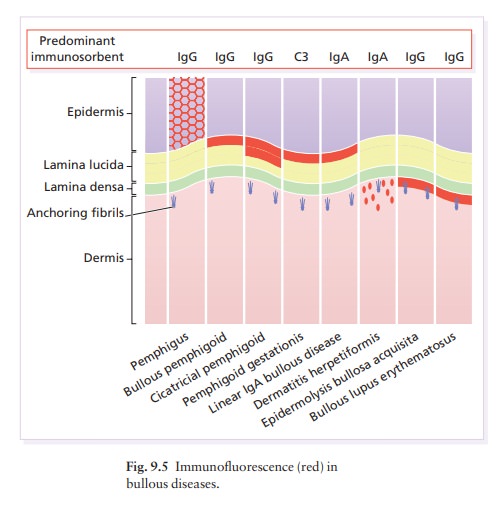
Pemphigoid
may look like other bullous diseases, espe-cially epidermolysis bullosa
acquisita, bullous lupus erythematosus, dermatitis herpetiformis, pemphigoid
gestationis, bullous erythema multiforme and linear IgA bullous disease.
Immunofluorescence helps to separate it from these (Fig. 9.5).
Investigations
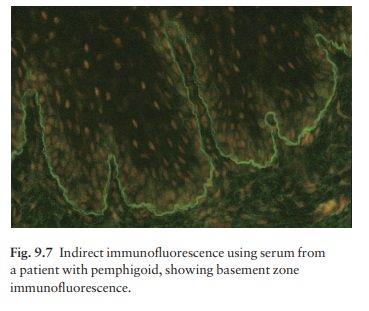
The
histology is that of a subepidermal blister, often filled with eosinophils.
Direct immunofluorescence shows a linear band of IgG and C3 along the base-ment
membrane zone. Indirect immunofluorescence, using serum from the patient,
identifies IgG antibodies that react with the basement membrane zone in some
70% of patients (Fig. 9.7).
Treatment
In the acute phase, prednisolone or prednisone at a dosage of 40 – 60 mg/day is usually needed to control the eruption. Immuno-suppressive agents may also be required. The dosage is reduced as soon as possible, and patients end up on a low maintenance regimen of systemic steroids, taken on alternate days until treatment is stopped. For unknown reasons, tetracyclines and niacinamide help some patients.
Related Topics