Chapter: Clinical Dermatology: Bullous diseases
Pemphigus
Bullous
disorders of immunological origin
In
pemphigus and pemphigoid, the damage is done by autoantibodies directed at
molecules that norm ally bind the skin.
This type of mechanism has not yet been proven for dermatitis herpetiformis; but the characteristic deposition of immunoglobulin (Ig) A in the papillary dermis, and an association with a variety of autoimmune dis-orders, both suggest an immunological basis for the disease.
Pemphigus
Pemphigus
is severe and potentially life-threatening. There are two main types. The most
common is pemphigus vulgaris, which accounts for at least three-quarters of all
cases, and for most of the deaths. Pemphigus vegetans is a rare variant of
pemphigus vulgaris. The other important type of pemphigus, superficial
pemphigus, also has two variants: the generalized foliaceus type and localized
erythema-tosus type. A few drugs, led by penicillamine, can trigger a
pemphigus-like reaction, but autoanti-bodies are then seldom found. Finally, a
rare type of pemphigus (paraneoplastic pemphigus) has been described in
association with a thymoma or an under-lying carcinoma; it is characterized by
unusually severe mucosal lesions.
Cause
All
types of pemphigus are autoimmune diseases in which pathogenic IgG antibodies
bind to antigens within the epidermis. The main antigens are des-moglein 3 (in
pemphigus vulgaris) and desmoglein 1 (in superficial pemphigus). Both are
cell-adhesion molecules of the cadherin family (see Table 2.5), found in desmosomes.
The antigen–antibody reaction interferes with adhesion, causing the
keratinocytes to fall apart.
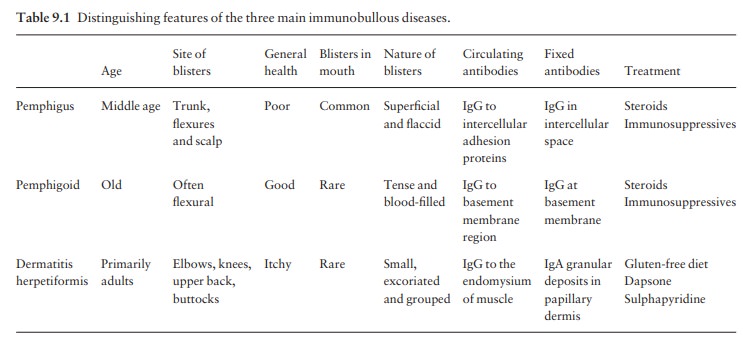
Presentation
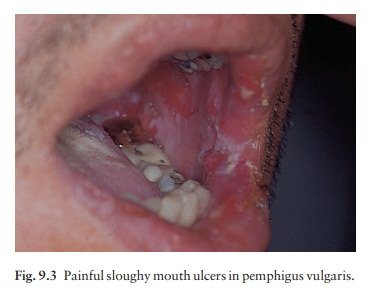
Pemphigus
vulgaris is characterized by flaccid blisters of the skin (Fig. 9.2) and mouth
(Fig. 9.3) and, after the blisters rupture, by widespread painful erosions.
Most patients develop the mouth lesions first.

Shearing stresses
on normal skin can cause new erosions to form (a positive Nikolsky sign). In
the vegetans variant (Fig. 9.4), heaped up cauliflower-like weeping areas are
present in the groin and body folds. The blisters in pemphigus foliaceus are so
superficial, and rupture so easily, that the clinical picture is dominated more
by weeping and crusting erosions than by blisters. In the rarer pemphigus
erythematosus, the facial lesions are often pink, dry and scaly.

Course
The
course of all forms of pemphigus is prolonged, even with treatment, and the
mortality rate of pemphigus vulgaris is still at least 15%. Superficial
pemphigus is less severe. With modern treatments, most patients with pemphigus
can live relatively normal lives, with occasional exacerbations.
Complications
Complications
are inevitable with the high doses of steroids and immunosuppressive drugs that
are needed to control the condition. Indeed, side-effects of treat-ment are now
the leading cause of death. Infections of all types are common. The large areas
of denuda-tion may become infected and smelly, and severe oral ulcers make
eating painful.
Differential diagnosis
Widespread
erosions may suggest a pyoderma, impetigo, epidermolysis bullosa or ecthyma.
Mouth ulcers can be mistaken for aphthae, Behçet’s disease or a herpes simplex
infection.
Investigations
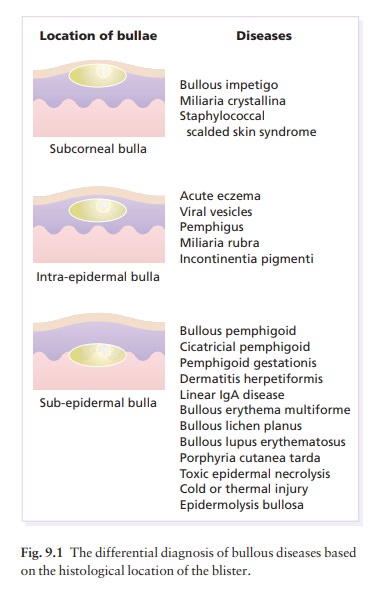
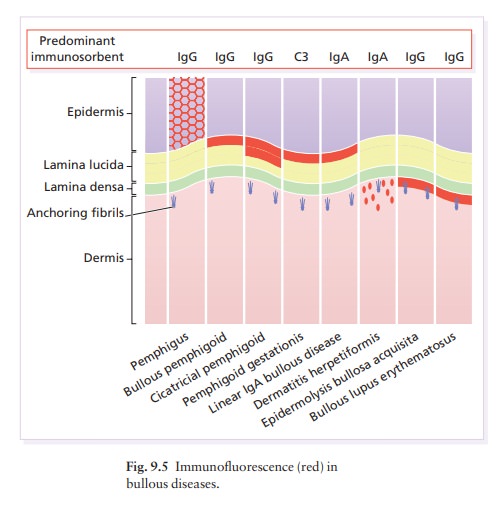
Biopsy
shows that the vesicles are intraepidermal, with rounded keratinocytes floating
freely within the blister cavity (acantholysis). Direct immunofluorescence of adjacent normal skin shows intercellular
epidermal deposits of IgG and C3 (Fig. 9.5). The serum from a patient with
pemphigus contains antibodies that bind to the desmogleins in the desmosomes of
normal epidermis, so that indirect immunofluorescence can also be used to confirm the diagnosis.
The titre of these antibodies correlates loosely with clinical activ-ity and
may guide changes in the dosage of systemic steroids.
Treatment
Because
of the dangers of pemphigus vulgaris, and the difficulty in controlling it,
patients should be treated in a specialized unit. Resistant and severe cases
need very high doses of systemic steroids, such as prednis-olone 80–320 mg/day, and the dose is dropped only
when new blisters stop appear-ing. Immunosuppressive agents, such as
azathioprine or cyclophosphamide and, recently, mycophenylate mofetil, are
often used as steroid-sparing agents. New and promising approaches include
plasmapheresis and intravenous immunoglobulin as used in other auto-immune
diseases. Treatment needs regular follow-up and is usually prolonged. In
superficial pemphigus, smaller doses are usually needed, and the use of
top-ical corticosteroids may help too
Related Topics