Chapter: Clinical Dermatology: Bullous diseases
Dermatitis herpetiformis
Dermatitis
herpetiformis
Dermatitis
herpetiformis is a very itchy chronic subepidermal vesicular disease, in which
the vesicles erupt in groups as in herpes simplexahence the name
ŌĆśherpetiformisŌĆÖ.
Cause
Gluten-sensitive
enteropathy, demonstrable by small bowel biopsy, is always present, but most
patients do not suffer from diarrhoea, constipation or mal-nutrition as the
enteropathy is mild, patchy and involves only the proximal small intestine.
Absorption of gluten, or another dietary antigen, may form cir-culating immune
complexes that lodge in the skin. A range of antibodies can be detected,
notably directed against reticulin, gliadin and endomysiumaa com-ponent of
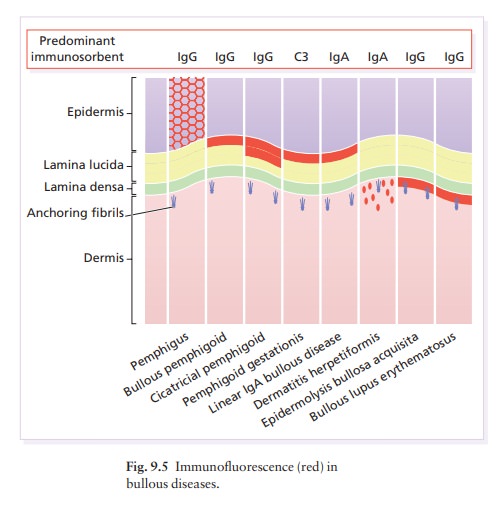
smooth muscle. Granular deposits of IgA and C3 in the superficial dermis under
the basement membrane zone (Fig. 9.5) induce inflammation, which then separates
the epidermis from the dermis. These deposits clear slowly after the
introduction of a gluten-free diet.
Presentation
The
extremely itchy, grouped vesicles (Fig. 9.9) and urticated papules develop
particularly over the elbows (Fig. 9.10) and knees, buttocks and shoulders.
They are often broken by scratching before they reach any size. A typical
patient therefore shows only grouped excoriations, sometimes with eczema-like
changes added by scratching.


Course
The
condition typically lasts for decades.
Complications
The complications of gluten-sensitive enteropathy include diarrhoea, abdominal pain, anaemia and, rarely, malabsorption. Small bowel lymphomas have been reported, and the use of a gluten-free diet may reduce this risk. There is a proven association with other autoimmune diseases, most commonly of the thyroid. Treatment, notably with dapsone, can cause side-effects.
Differential diagnosis
The
disorder masquerades as scabies, an excoriated eczema, insect bites or
neurodermatitis.
Investigations
If
a vesicle can be biopsied before it is scratched away, the histology will be
that of a subepidermal blister, with neutrophils packing the adjacent dermal
papil-lae. Direct immunofluorescence of uninvolved skin shows granular deposits
of IgA, and usually C3, in the dermal papillae and superficial dermis (Fig.
9.5). Small bowel biopsy is no longer recommended as routine because the
changes are often patchy. Tests for malabsorption are seldom needed.
Treatment
The disorder responds to a gluten-free diet, which should be supervised by a dietitian. Adherence to this can be monitored using the titre of antiendomysial antibody, which should fall if gluten is strictly avoided.
The bowel changes revert quickly to normal but IgA
deposits remain in the skin, and the skin disease can drag on for many months.
Because of this, and because a gluten-free diet is hard to follow and enjoy,
some patients prefer to combine the diet with dapsone or sulphapyridine
(sulfapyridine) at the start, although both can cause severe rashes, haemolytic
anaemia (especially in those with glucose-6-phosphate dehydrogenase
deficiency), leucopenia, thrombocytopenia, methaemoglobinaemia and peri-pheral
neuropathy. Regular blood checks are therefore necessary.
Related Topics