Chapter: Medical Physiology: Heart Muscle; The Heart as a Pump and Function of the Heart Valves
The Cardiac Cycle
The Cardiac Cycle
The cardiac events that occur from the beginning of one heartbeat to the beginning of the next are called the cardiac cycle. Each cycle is initiated by sponta-neous generation of an action potential in the sinusnode. This node is locatedin the superior lateral wall of the right atrium near the opening of the superior vena cava, and the action potential travels from here rapidly through both atria and then through the A-V bundle into the ventricles. Because of this special arrangement of the conducting system from the atria into the ventricles, there is a delay of more than 0.1 second during passage of the cardiac impulse from the atria into the ventricles. This allows the atria to contract ahead of ventricular con-traction, thereby pumping blood into the ventricles before the strong ventricular contraction begins. Thus, the atria act as primer pumps for the ventricles, and the ventricles in turn provide the major source of power for moving blood through the body’s vascular system.
Diastole and Systole
The cardiac cycle consists of a period of relaxation called diastole, during which the heart fills with blood, followed by a period of contraction calledsystole.
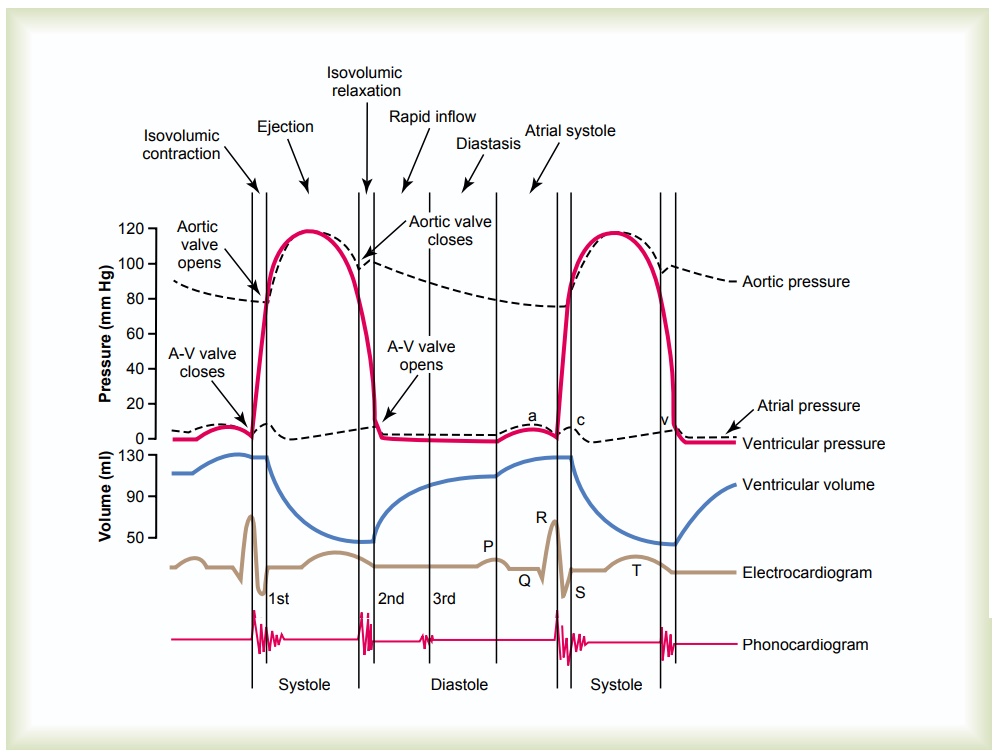
Figure 9–5 shows the different events during the cardiac cycle for the left side of the heart.The top three curves show the pressure changes in the aorta, left ven-tricle, and left atrium, respectively. The fourth curve depicts the changes in left ventricular volume, the fifth
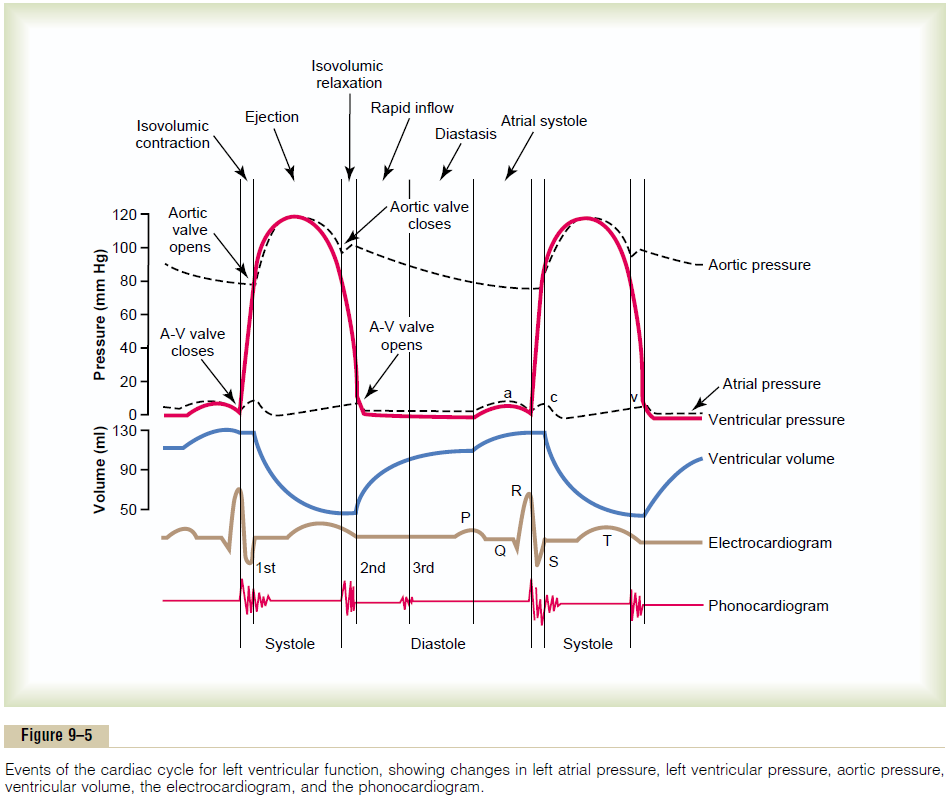
the electrocardiogram, and the sixth a phonocardio-gram, which is a recording of the sounds produced by the heart—mainly by the heart valves—as it pumps. It is especially important that the reader study in detail this figure and understand the causes of all the events shown.
Relationship of the Electrocardiogram to the Cardiac Cycle
The electrocardiogram in Figure 9–5 shows the P, Q,R, S, and T waves. They are electrical voltages generated by the heart and recorded by the electrocardiograph from the surface of the body.
The P wave is caused by spread of depolarization through the atria, and this is followed by atrial con-traction, which causes a slight rise in the atrial pres-sure curve immediately after the electrocardiographic P wave.
About 0.16 second after the onset of the P wave, the QRS waves appear as a result of electrical depolariza-tion of the ventricles, which initiates contraction of the ventricles and causes the ventricular pressure to begin rising, as also shown in the figure. Therefore, the QRS complex begins slightly before the onset of ventricu-lar systole.
Finally, one observes the ventricular T wave in the electrocardiogram. This represents the stage of repo-larization of the ventricles when the ventricular muscle fibers begin to relax. Therefore, the T wave occurs slightly before the end of ventricular contraction.
Function of the Atria as Primer Pumps
Blood normally flows continually from the great veins into the atria; about 80 per cent of the blood flows directly through the atria into the ventricles even before the atria contract. Then, atrial contraction usually causes an additional 20 per cent filling of the ventricles. Therefore, the atria simply function as primer pumps that increase the ventricular pumping effectiveness as much as 20 per cent. However, the heart can continue to operate under most conditions even without this extra 20 per cent effectiveness because it normally has the capability of pumping 300 to 400 per cent more blood than is required by the resting body. Therefore, when the atria fail to function, the difference is unlikely to be noticed unless a person exercises; then acute signs of heart failure occasionally develop, especially shortness of breath.
Pressure Changes in the Atria—The a, c, and v Waves. In the atrial pressure curve of Figure 9–5, three minor pressure elevations, called the a, c, and v atrial pressure waves, are noted.
The a wave is caused by atrial contraction. Ordinarily, the right atrial pressure increases 4 to 6 mm Hg during atrial contraction, and the left atrial pressure increases about 7 to 8 mm Hg.
The c wave occurs when the ventricles begin to contract; it is caused partly by slight backflow of blood into the atria at the onset of ventricular contraction but mainly by bulging of the A-V valves backward toward the atria because of increasing pressure in the ventricles.
The v wave occurs toward the end of ventricular contraction; it results from slow flow of blood into the atria from the veins while the A-V valves are closed during ventricular contraction. Then, when ventricular contraction is over, the A-V valves open, allowing this stored atrial blood to flow rapidly into the ventricles and causing the v wave to disappear.
Function of the Ventricles as Pumps
Filling of the Ventricles. During ventricular systole, largeamounts of blood accumulate in the right and left atria because of the closed A-V valves. Therefore, as soon as systole is over and the ventricular pressures fall again to their low diastolic values, the moderately increased pressures that have developed in the atria during ventricular systole immediately push the A-V valves open and allow blood to flow rapidly into the ventricles, as shown by the rise of the left ventricularvolume curve in Figure 9–5. This is called the period of rapid filling of the ventricles.
The period of rapid filling lasts for about the first third of diastole. During the middle third of diastole, only a small amount of blood normally flows into the ventricles; this is blood that continues to empty into the atria from the veins and passes through the atria directly into the ventricles.
During the last third of diastole, the atria contract and give an additional thrust to the inflow of blood into the ventricles; this accounts for about 20 per cent of the filling of the ventricles during each heart cycle.
Emptying of the Ventricles During Systole
Period of Isovolumic (Isometric) Contraction. Immedi-ately after ventricular contraction begins, the ventric-ular pressure rises abruptly, as shown in Figure 9–5, causing the A-V valves to close. Then an additional 0.02 to 0.03 second is required for the ventricle to build up sufficient pressure to push the semilunar (aortic and pulmonary) valves open against the pressures in the aorta and pulmonary artery. Therefore, during this period, contraction is occurring in the ventricles, but there is no emptying. This is called the period of iso-volumic or isometric contraction, meaning that tensionis increasing in the muscle but little or no shortening of the muscle fibers is occurring.
Period of Ejection. When the left ventricular pressurerises slightly above 80 mm Hg (and the right ventricu-lar pressure slightly above 8 mm Hg), the ventricular pressures push the semilunar valves open. Immedi-ately, blood begins to pour out of the ventricles, with about 70 per cent of the blood emptying occurring during the first third of the period of ejection and the remaining 30 per cent emptying during the next two thirds. Therefore, the first third is called the period ofrapid ejection, and the last two thirds, the period of slow ejection.
Period of Isovolumic (Isometric) Relaxation. At the end ofsystole, ventricular relaxation begins suddenly, allow-ing both the right and left intraventricular pressures to decrease rapidly. The elevated pressures in the dis-tended large arteries that have just been filled with blood from the contracted ventricles immediately push blood back toward the ventricles, which snaps the aortic and pulmonary valves closed. For another 0.03 to 0.06 second, the ventricular muscle continues to relax, even though the ventricular volume does not change, giving rise to the period of isovolumic or iso-metric relaxation. During this period, the intraven-tricular pressures decrease rapidly back to their low diastolic levels. Then the A-V valves open to begin a new cycle of ventricular pumping.
End-Diastolic Volume, End-Systolic Volume, and Stroke Volume Output. During diastole, normal filling of the ventriclesincreases the volume of each ventricle to about 110 to 120 milliliters. This volume is called the end-diastolicvolume. Then, as the ventricles empty during systole,the volume decreases about 70 milliliters, which is called the stroke volume output. The remaining volume in each ventricle, about 40 to 50 milliliters, is called the end-systolic volume.The fraction of the end-diastolicvolume that is ejected is called the ejection fraction— usually equal to about 60 per cent.
When the heart contracts strongly, the end-systolic volume can be decreased to as little as 10 to 20 milli-liters. Conversely, when large amounts of blood flow into the ventricles during diastole, the ventricular end-diastolic volumes can become as great as 150 to 180 milliliters in the healthy heart. By both increasing the end-diastolic volume and decreasing the end-systolic volume, the stroke volume output can be increased to more than double normal.
Function of the Valves
Atrioventricular Valves. TheA-V valves(thetricuspidand mitral valves) prevent backflow of blood from the ventricles to the atria during systole, and thesemilu-nar valves (the aortic and pulmonary artery valves)prevent backflow from the aorta and pulmonary ar-teries into the ventricles during diastole. These valves, shown in Figure 9–6 for the left ventricle, close and open passively. That is, they close when a backward pressure gradient pushes blood backward, and they open when a forward pressure gradient forces blood in the forward direction. For anatomical reasons, the thin, filmy A-V valves require almost no backflow to cause closure, whereas the much heavier semilunar valves require rather rapid backflow for a few milliseconds.
Function of the Papillary Muscles. Figure 9–6 alsoshows papillary muscles that attach to the vanes of the A-V valves by the chordae tendineae. The papillary muscles contract when the ventricular walls contract, but contrary to what might be expected, they do not help the valves to close. Instead, they pull the vanes of the valves inward toward the ventricles to prevent their bulging too far backward toward the atria during ventricular contraction. If a chorda tendinea becomes ruptured or if one of the papillary muscles becomes paralyzed, the valve bulges far backward during ven-tricular contraction, sometimes so far that it leaks severely and results in severe or even lethal cardiac incapacity.
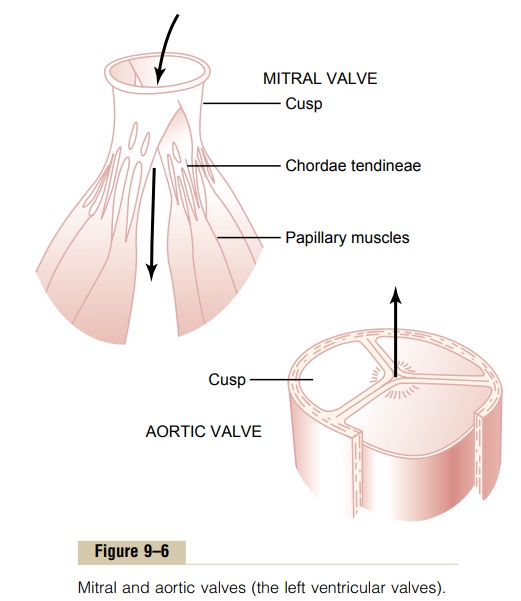
Aortic and Pulmonary Artery Valves. The aortic and pul-monary artery semilunar valves function quite differ-ently from the A-V valves. First, the high pressures in the arteries at the end of systole cause the semilunar valves to snap to the closed position, in contrast to the much softer closure of the A-V valves. Second, because of smaller openings, the velocity of blood ejection through the aortic and pulmonary valves is far greater than that through the much larger A-V valves. Also, because of the rapid closure and rapid ejection, the edges of the aortic and pulmonary valves are subjected to much greater mechanical abrasion than are the A-V valves. Finally, the A-V valves are supported by the chordae tendineae, which is not true for the semi-lunar valves. It is obvious from the anatomy of the aortic and pulmonary valves (as shown for the aortic valve at the bottom of Figure 9–6) that they must be constructed with an especially strong yet very pliable fibrous tissue base to withstand the extra physical stresses.
Aortic Pressure Curve
When the left ventricle contracts, the ventricular pres-sure increases rapidly until the aortic valve opens. Then, after the valve opens, the pressure in the ventri-cle rises much less rapidly, as shown in Figure 9–5, because blood immediately flows out of the ventricle into the aorta and then into the systemic distribution arteries.
The entry of blood into the arteries causes the walls of these arteries to stretch and the pressure to increase to about 120 mm Hg.
Next, at the end of systole, after the left ventricle stops ejecting blood and the aortic valve closes, the elastic walls of the arteries maintain a high pressure in the arteries, even during diastole.
A so-called incisura occurs in the aortic pressure curve when the aortic valve closes. This is caused by a short period of backward flow of blood immediately before closure of the valve, followed by sudden cessa-tion of the backflow.
After the aortic valve has closed, the pressure in the aorta decreases slowly throughout diastole because the blood stored in the distended elastic arteries flows continually through the peripheral vessels back to the veins. Before the ventricle contracts again, the aortic pressure usually has fallen to about 80 mm Hg (dias-tolic pressure), which is two thirds the maximal pres-sure of 120 mm Hg (systolic pressure) that occurs in the aorta during ventricular contraction.
The pressure curves in the right ventricle and pul-monary artery are similar to those in the aorta, exceptthat the pressures are only about one sixth as great.
Related Topics