Chapter: Obstetrics and Gynecology: Infectious Diseases in Pregnancy
Syphilis - Infectious Diseases in Pregnancy
SYPHILIS
Syphilis is a
systemic disease caused by the motile spirocheteTreponema pallidum. The spirochete is transmitted by directcontact,
invading intact mucous membranes or areas of abraded skin. A painless ulcer at
the site of inoculation fol-lows, usually within 6 weeks following exposure.
The ulcer is firm, with elevated edges; it lasts for several weeks. One to 3
months later, a skin rash occurs, or, in some patients, raised lesions (condyloma lata) appear on the
genitalia.
T.
pallidum is generally considered to cross the placentato the
fetus after 16 weeks of gestation. Transmission can occur at any stage of
maternal infection and has been doc-umented at as early as 6 weeks of
gestation.
Spontaneous abortion, stillbirth,
and neonatal death are more frequent in any untreated patient, whereas neonatal
infection is more likely in primary or secondary rather than latent syphilis.
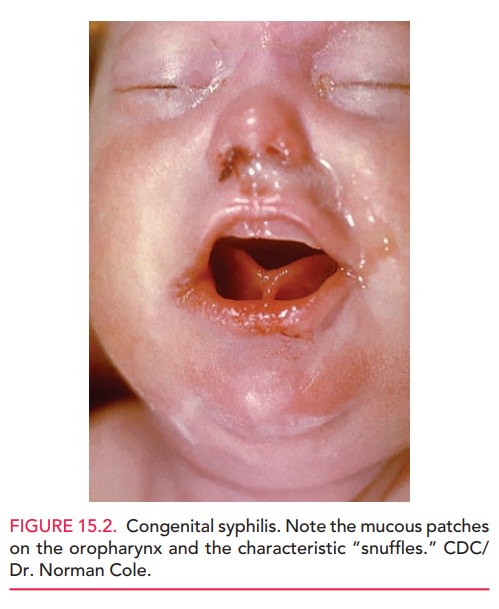
Newborns with congenital syphilis may be asymptomatic or have the classic signs
of the syndrome, al-though most infants do not develop evidence of disease for
10 to 14 days after delivery. Early evidence of the disease includes a
maculopapular rash, “snuffles,” mucous patches on the oropharynx,
hepatosplenomegaly, jaundice, lymph-adenopathy, and chorioretinitis (Fig.
15.2). Later signs in-clude Hutchinson teeth, mulberry molars, saddle nose, and
saber shins.
Congenital
syphilis is readily preventable with promptand appropriate
maternal treatment. Therefore, all preg-nant women should be screened
serologically as early as possible and again at delivery (and if exposed to an
infected partner). Serologic testing is the mainstay of diagnosis. Nontreponemal screening tests (Venereal
Disease Re-search Laboratory [VDRL], rapid plasma reagin [RPR]) are sometimes
falsely positive; treponemal-specific
tests (fluorescent treponemal antibody absorbed [FTA-ABS], T.pallidum particle agglutination [TP-PA])
are used to confirm infection and identify antibodies specific for T. pallidum. A positive
treponemal-specific test result in-dicates either active disease or previous
exposure; re-gardless of treatment, the test remains positive for life in most
individuals.
Therapy differs by stage of
disease and is generally the same as that recommended for nonpregnant adults.
There are no proven alternative therapies to penicillin for treating syphilis
in pregnancy. Therefore, patients with penicillin sensitivity require skin
testing, followed by de-sensitization for those with a true penicillin allergy.
The Jarisch-Herxheimer reaction occurs most often among patients with early
syphilis and is an acute febrile reaction that typically occurs in the first 24
hours after treatment. In pregnancy, this
reaction may precipitate preterm labor or cause fetal distress and may warrant
close observation of mothers after treatment. Post-treatment titers (RPR or
VDRL)should be followed serially for at least one year. A fourfold increase in
serologic titer, or persistent or recurrent signs or symptoms, may indicate
inadequate treatment or re-infection. Retreatment is indicated in either case.
Response to therapy is again evaluated by following serologic titers.
Related Topics