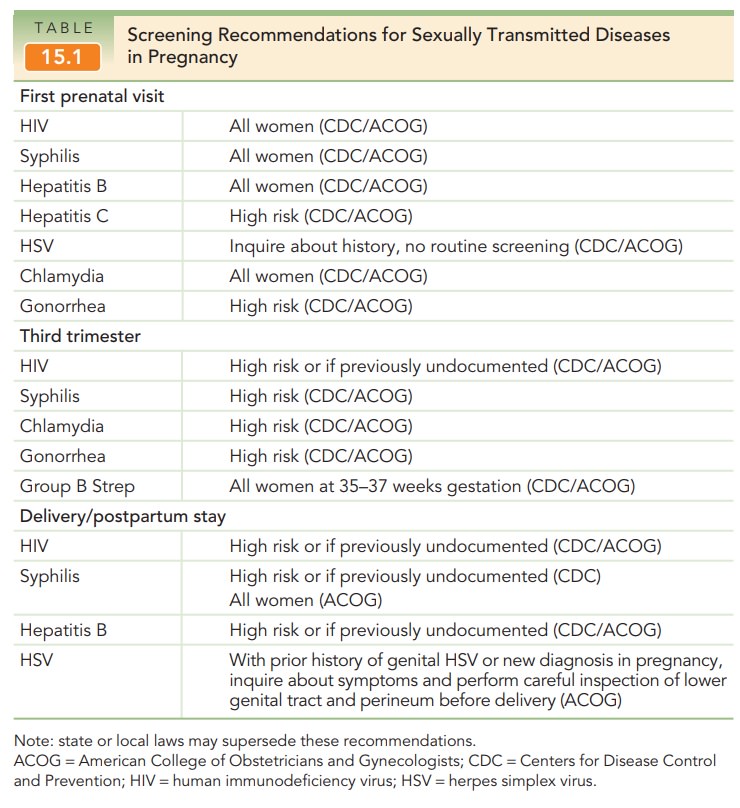
Chapter: Obstetrics and Gynecology: Infectious Diseases in Pregnancy
Herpes - Infectious Diseases in Pregnancy
HERPES
Herpes
simplex virus (HSV) is a double-stranded DNAvirus
that can be differentiated into HSV type 1 (HSV-1)
and HSV type 2 (HSV-2). Herpes
simplex virus type 1 is the primary etiologic agent of herpes labialis,
gingivostomatitis, and keratoconjunctivitis. Most genital infections with HSV
are caused by HSV-2, but genital HSV-1 infections are be-coming increasingly
common, particularly among adoles-cent and young women. Up to 80% of new
genital infections among women may be due to HSV-1, with the highest rates
occurring in adolescents and young adults. Herpes infec-tions are categorized
as follows:
· Primary occurs in
a woman with no evidence of priorHSV infection (seronegative to both HSV-1 and
HSV-2).
· Nonprimary first episode occurs in
a woman with ahistory of heterologous infection (first HSV-2 infection with a
prior HSV-1 infection).
·
Recurrent
disease occurs in a woman with clinical orserologic
evidence of prior genital herpes (of the same serotype).
The primary form poses the
greatest risk to the fetus. The fetus/neonate is infected either from
ascending infection following
spontaneous rupture of membranes, or from passage through an infected lower
genital tract at delivery. With a primary
infection at the time of delivery, the risk of neonatal infection approaches
50%; it is far lower (approxi-mately 3%) with recurrent infection, as the size
of the inoculum is much decreased. In utero fetal infection can occur,
al-though this is much less common. Most infants with local-ized herpes
infection ultimately do well; as a rule, infants with disseminated infection do
very poorly.
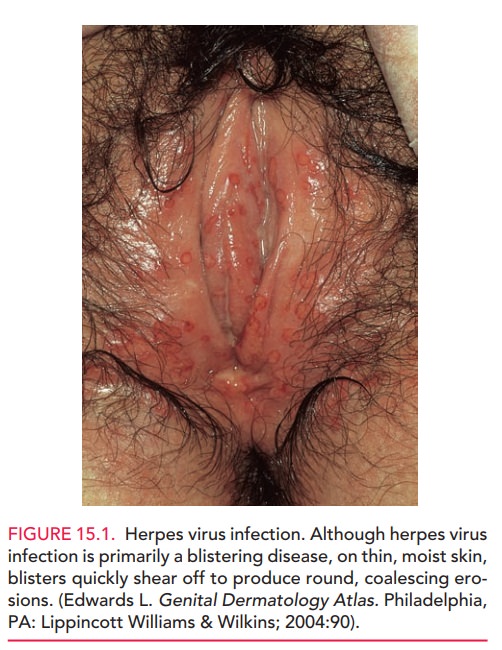
The diagnosis of HSV infection is
suspected when clinical examination shows the characteristic tender vesi-cles
with ulceration followed by crusting (Figure 15.1). Confirmation is by
identification of the virus in cell cul-ture, with most positive results
reported within 72 hours. Polymerase chain reaction (PCR) testing is
commercially available and is more sensitive than culture. Serologic test-ing
for HSV-1 and HSV-2 immunoglobulin is also avail-able and a helpful ancillary
test because cultures of crusted or healing lesions can often be negative.
Type-specific serologic testing that accurately distinguishes between
anti-HSV-1 and -2 immunoglobulin is recommended.
All pregnant women should be asked about a history of HSV infection at their initial prenatal visit. If infection withherpes virus is suspected during the course of pregnancy in a woman with undocumented history of HSV, a culture from a le-sion should be obtained to confirm the diagnosis. In such patients,or any patient with a history of herpes virus infection, care-ful inspection of the lower genital tract is important at the onset of labor or when rupture of membranes occurs. If no lesions are identified, vaginal delivery is deemed safe.
Cesarean delivery is recommended if herpes lesions are iden-tified on the cervix, in the vagina, or on the vulva at the time of labor or if spontaneous rupture of membranes occurs. This is true whether or not the lesions are associated with primary or recurrent infection due to the severity of neo-natal disease.
Acyclovir and related compounds
are safe in pregnancy and can be used if symptoms are severe. Additionally, in
pa-tients with recurrent HSV, these medications should be of-fered for
suppression of outbreaks starting at 36 weeks of gestation to reduce the risk
of viral shedding and cesarean delivery due to active lesions. Routine
antepartum genital HSV cultures in asymptomatic women are not recom-mended, as
these tests do not predict viral shedding at de-livery. Routine type-specific serologic screening for HSV is notcurrently
recommended. However, serologic screening maybe considered in certain
populations to identify women who may benefit from suppressive therapy or
preventive measures.
Related Topics