Chapter: Obstetrics and Gynecology: Infectious Diseases in Pregnancy
Hepatitis - Infectious Diseases in Pregnancy
HEPATITIS
Viral hepatitis is one of the
most common and potentially serious infections that can occur in pregnant
women. Six forms of viral hepatitis have now been identified, two of which,
hepatitis A and hepatitis B, can be prevented effec-tively through vaccination.
Hepatitis A
Hepatitis
A virus (HAV) is transmitted from person toperson primarily
through fecal–oral contamination. Good hygiene and proper sanitation are
important to prevent in-fection. However, vaccination is the most effective
means of preventing transmission. The hepatitis A vaccine is available as both
a single-antigen vaccine and as a combination vac-cine (containing both HAV and
HBV antigens). Prior to vaccine availability, HAV accounted for one-third of cases
of acute hepatitis in the United States. HAV infection does not progress to
chronic infection. Diagnosis is confirmed by demonstration of anti-HAV IgM
antibodies. HAV infection has no specific effects on pregnancy or the fetus. Vaccinationsafety during pregnancy has not
been established, but the risk to the developing fetus is minimal because the
vaccine contains inacti-vated purified viral proteins. Vaccination is
recommended forindividuals who are intravenous (IV) drug users, who have
certain medical disorders (chronic liver disease or receiving clotting factor
concentrates), are employed in specific occu-pations (e.g., working in primate
labs or research labs), and who travel to countries with endemic HAV infection.
HAVimmune globulin is effective for both
pre- and post-exposure pro-phylaxis and can be used during pregnancy.
Hepatitis B
Hepatitis
B virus (HBV) infection is more serious thanHAV infection
regardless of pregnancy status. HBV is transmitted by the parenteral route and
through sexual contact. Ten to fifteen percent of infected adults develop
chronic infection and, of those, some will become carriers. Testing for hepatitis B surface antigen
(HBsAg) during preg-nancy is routine, as about half of pregnant women infected
lack traditional high-risk factors. Vertical transmission of
hepatitisoccurs to a significant but variable extent and is related to the
presence or absence of maternal HBeAg: if the patient is positive for the “e”
antigen, indicating a high viral load and active viral replication, her fetus
has 70% to 90% risk of becoming infected; and most of such infants will become
chronic carriers. The risk of fetal
infection is higher if mater-nal infection occurs in the third trimester. Neonatal
infectioncan also occur via breast milk.
Women who
are HBsAg negative with risk factors for HBV infection should be offered
vaccination during pregnancy.
Patients who have been exposed to
HBV should be treated as soon as possible with hepatitis B immune glob-ulin
(HBIG) and begin the vaccination series. All infants now receive vaccination
against hepatitis B, with the ini-tial injection given between 2 days and 2
months of deliv-ery. Infants of mothers
who are HBsAg positive should receivethe vaccine and HBIG within 12 hours of
birth. Breastfeedingis not contraindicated in women who are chronic
carriers if their infants have received both the vaccination and HBIG within 12
hours of delivery.
Hepatitis C
Hepatitis
C virus (HCV) infection is a growing problemin the United
States and has obstetric implications. Similar to HBV in transmission (sexual,
parenteral, vertical), HCV infection is often asymptomatic. Diagnosis is made
by serologic evidence of anti-HCV IgG. However, antibod-ies may not be
detectable until up to 10 weeks after onset of clinical illness. PCR
identification of HCV RNA may be a useful adjunct to diagnosis in early and
chronic infection. The presence of anti-HCV antibody does not confer im-munity
or prevent transmission of infection. Fifty percent of infected individuals go
on to have chronic infection.
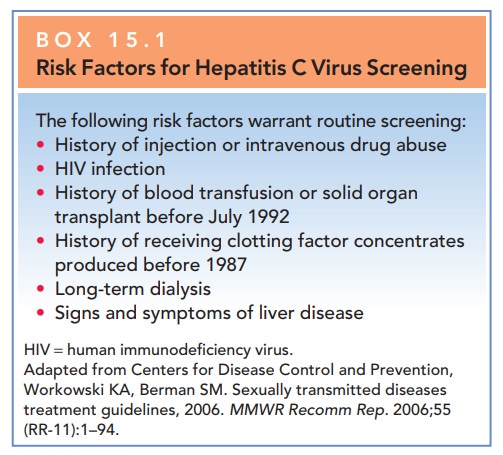
Screening for evidence of HCV infection is not rou-tine. However, the CDC recommends routine screening for cer-tain groups (Box 15.1). Vertical transmission occurs in 2%to 12% of cases, with the risk of fetal infection directly re-lated to the quantity of hepatitis C RNA virus in maternal blood. Vertical transmission is rare with an undetectable hepatitis C RNA viral load. Maternal co-infection with human immunodeficiency virus (HIV) is also associatedwith a higher risk of vertical transmission of HCV.
Other risk factors for fetal infection
include prolonged rupture of membranes in labor and use of invasive fetal
monitoring. Currently, there are no
preventive measures known to reduce the risk of mother-to-child transmission;
cesarean delivery has not been consistently associated with a decreased rate of
vertical trans-mission and should be performed for usual obstetric indications
in HCV-infected women. Breastfeeding is not contraindicatedin women with
HCV. Newer therapies for HCV infection that clear detectable virus in the blood
and normalize transaminase levels are promising in nonpregnant adults. Immune
globulin does not contain antibodies to HCV and has no role in postexposure
prophylaxis.
Hepatitis D and E
Hepatitis
D virus (HDV) is an incomplete viral particlethat can only
cause infection in the presence of HBV. Transmission of HDV is through the
parenteral route; chronic infection can occur, resulting in severe disease in
70% to 80% of chronically infected individuals and mortal-ity rates as high as
25%. Vertical transmission has been
docu-mented but is uncommon. Diagnosis is made by identificationof HDV
antigen and anti-HDV IgM in acute disease; IgG antibodies develop, but are not
protective. No vaccine is currently available. Measures to prevent HBV
infection are effective in the prevention of HDV transmission.
Hepatitis
E virus (HEV) infection is a waterbornedisease and is
uncommon in the United States. The
diseaseis typically self-limited, but has been associated with higher rates of
fulminant hepatitis E and mortality in pregnant women, which can be as high as
20% after infection in the third tri-mester. Co-infection with HIV results
in severe diseaseand high mortality in pregnancy. Diagnosis is made by
serologic testing for HEV-specific antibodies in women with travel exposure.
The risk of vertical transmission is very low, but cases have been reported. No
vaccine is cur-rently available.
Related Topics