Chapter: Obstetrics and Gynecology: Infectious Diseases in Pregnancy
Chlamydia - Infectious Diseases in Pregnancy
CHLAMYDIA
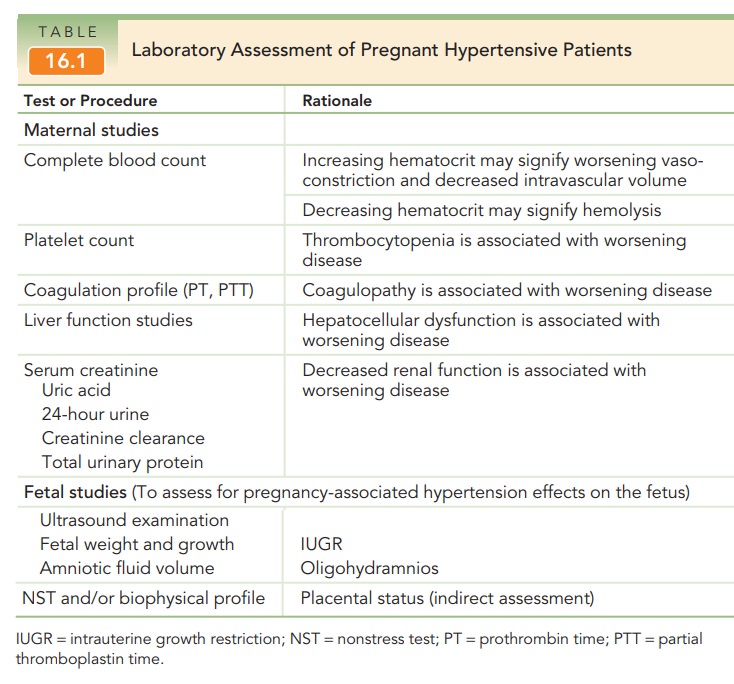
Antepartum screening for Chlamydia
trachomatis should be performed early in pregnancy and repeated in the
third trimester based on risk factors (see Table 16.1). It has been detected in
2% to 13% of pregnant women, depending on the population, and is generally
found in 5% of all popula-tions. In pregnant women, infection is often
asymptomatic but may cause urethritis or mucopurulent cervicitis. Like
gonorrhea, infection of the upper genital tract is uncom-mon during pregnancy,
although chlamydia infection has been associated with postpartum endometritis
and infertil-ity. Diagnosis is made by culture, direct fluorescent anti-body
staining, enzyme immunoassay, DNA probe, or PCR.
Maternal chlamydia infection at
the time of delivery results in colonization of the neonate in 50% of cases.
Neonates colonized at birth may go on to develop puru-lent conjunctivitis soon
after birth or pneumonia at 1 to 3 months of age. Routine prophylaxis against
neonatal gonococcal ophthalmia is not generally effective against chlamydial
conjunctivitis; systemic treatment of the infant is necessary. Fortunately,
neonatal chlamydial ophthalmia and pneumonia are becoming less common with the
insti-tution of universal prenatal screening and treatment. Recommended
treatment of genital infection with C.
tra-chomatis in pregnancy includes azithromycin or amoxicillin.
Doxycycline
and ofloxacin are contraindicated during preg-nancy.
Repeat testing to confirm
successful treatment, preferably by culture performed 3 to 4 weeks after
completion of ther-apy, is recommended in pregnancy.
Related Topics