Chapter: Microbiology and Immunology: Bacteriology: Streptococcus and Enterococcus
Streptococcus agalactiae
Streptococcus agalactiae
S. agalactiae is the only species belonging to group B strepto-cocci. This is a pathogen of the cattle causing bovine mastitis, hence named “agalactiae”. S. agalactiae are Gram-positive cocci arranged in pairs and short chains in clinical specimens and are morphologically similar to S. pyogenes. The cocci grow read-ily on enriched medium, such as blood agar and produce large colonies after overnight incubation.
S. agalactiae are found as commensals in the genitourinarytract and lower gastrointestinal tract. Vaginal carriage rate as high as 40–50% has been observed in some pregnant women. More than 50% of infants born to these mothers through vagi-nal delivery are colonized with S. agalactiae.
· S. agalactiae in neonates can cause either early-onset or late-onset infections. Early-onset infection is acquired either inutero or from mother’s vagina during delivery. The clinicalsymptoms develop during the first week of life. The condi-tion is characterized by septicemia, meningitis, or pneumo-nia. Late-onset infection is acquired from mother or from another infant (environment) during 2–12 weeks of life. The condition manifests as septicemia and meningitis.
· S. agalactiae in pregnant women causes urinary tract infec-tion particularly immediately after delivery.
· In nonpregnant women and in men, S. agalactiae can cause infections, such as osteomyelitis, arthritis, peritonitis, and skin infections.
The condition is diagnosed by culturing the specimen in the blood agar and identifying the colonies by various tests as men-tioned below:
1. CAMP test: CAMP (Christie, Atkins, Munch-Peterson) testwas first described in 1944 by Christie, Atkins, and Munch-Peterson. The basis for the test is that S. agalactiae produces a diffusible and heat-stable protein, known as CAMP fac-tor, which accentuates hemolysis of RBCs. The staphylococci
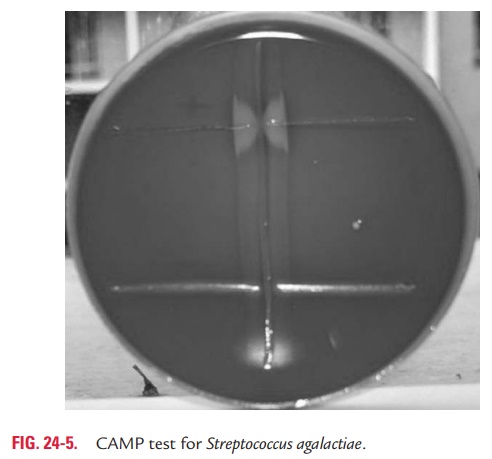
produce an enzyme sphingomyelinase C, which binds to the RBCs present in the blood agar. On exposure to CAMP factor liberated by S. agalactiae, RBCs undergo hemolysis, producing a butterfly appearance (Fig. 24-5, Color Photo 17). In this test, S. aureus is streaked from top to bottom on a blood agar plate.Then perpendicular streaks of S. agalactiae are made on either side, leaving at least 1 cm space from S. aureus. The plate is incu-bated overnight at 37°C in 20% CO2. Haemolysis showing a typ-ical butterfly appearance indicates a positive test. S. agalactiae is CAMP positive.
2.Hippurate hydrolysis test: S. agalactiaeare hippurate posi-tive. They hydrolyze the hippurate to produce hippuric acid.
3.Demonstration of group-specific cell wall antigen: Thebacteria are identified by the group-specific cell wall polysac-charide antigen or B antigen. This antigen is composed of rhamnose, N-acetylglucosamine, and galactose.
4.Demonstration of type-specific capsular antigen:
Depending upon type-specific capsular polysaccharide anti-gens, S. agalactiae strains have been classified into 11 distinct serotypes (Ia, Ia/c, Ib/c, II, IIc, III, IV, V, VI, VII, and VIII). Serum antibodies confer specific protection against these serotypes. Penicillin is the drug of choice for treatment of S. agalactiae infection. Vancomycin is given to persons allergic to penicillins. Recently, strains resistant to erythromycin and tetracycline have been documented.
Related Topics