Chapter: Modern Medical Toxicology: General Principles: General Management of Poisoning
Stabilisation: Assessment - General Management of Poisoning
Stabilisation
ASSESSMENT
The Airway and Breathing
Symptoms of airway obstruction
include dyspnoea, air hunger, and hoarseness. Signs comprise stridor,
intercostal and substernal retractions, cyanosis, sweating, and tachypnoea.
Normal oxygen delivery requires
adequate haemoglobin oxygen saturation, adequate haemoglobin levels, normal
oxygen unloading mechanisms, and an adequate cardiac output. Increasing
metabolic acidosis in the presence of a normal PaO2 suggests a toxin
or condition that either decreases oxygen carrying capacity (e.g. carbon
monoxide, methaemo-globinaemia), or reduces tissue oxygen (e.g. cyanide,
hydrogen sulfide).
The immediate need for assisted
ventilation has to be assessed clinically, but the efficiency of ventilation
can only be gauged by measuring the blood gases. Retention of carbon dioxide
(PaCO2> 45 mmHg or 6 Kpa), and hypoxia (PaO2< 70
mmHg or 9.3 Kpa) inspite of oxygen being given by a face mask are indications
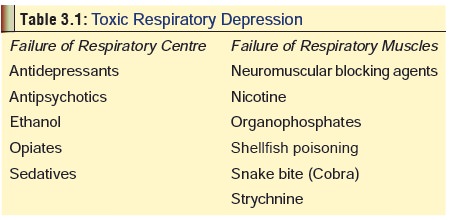
for assisted ventilation. Table 3.1
lists some substances which are known to cause respiratory depression. Some
drugs stimulate the respiratory centre: amphetamines, atropine, cocaine, and
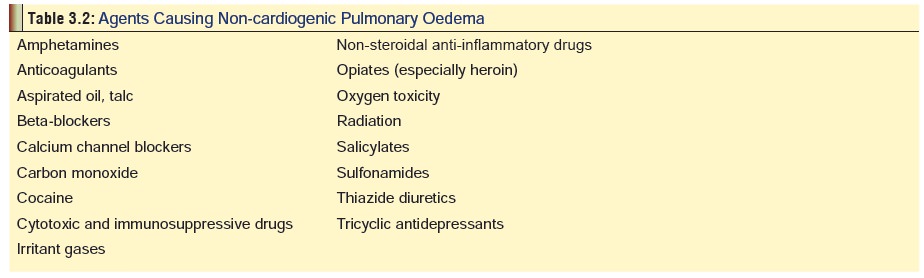
salicylates. Some drugs are associated with non-cardiogenic pulmonary oedema,
characterised by severe hypoxaemia, bilateral infiltrates on chest X-ray, and
normal pulmonary capillary wedge pressure (Table
3.2).
Some drugs cause or exacerbate
asthma. The most impor-tant among them include NSAIDs, antibiotics like
penicillins, cephalosporins, tetracycline, and nitrofurantoin, cholinergic
drugs, chemotherapeutic drugs, and some diuretics.
Circulation
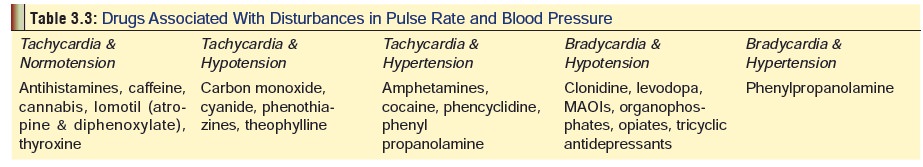
Several drugs produce changes in
pulse rate and blood pressure (Table 3.3),
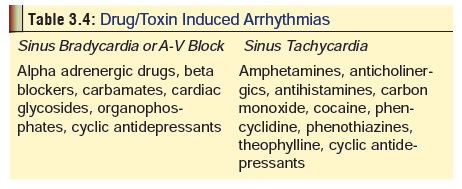
while others induce cardiac arrhythmias and heart block (Table 3.4).
Depression of Central Nervous System
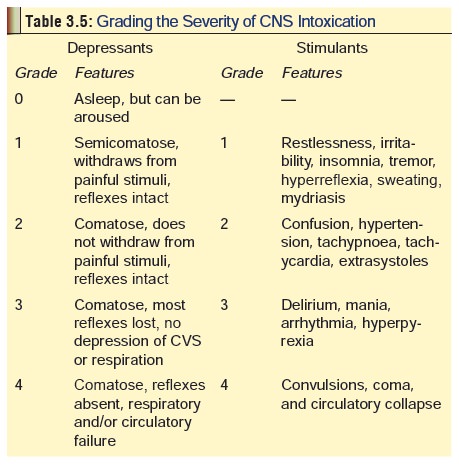
This is generally defined as an
unarousable lack of aware-ness with a rating of less than 8 on the Glasgow ComaScale (Appendix 1). However, the European Association ofPoison Centres and
Clinical Toxicologists (EAPCCT) are of the opinion that this scale while being
very useful for trauma patients is inappropriate for acute poisoning. Several
other scales have been proposed, including Reaction
Level Scale, Comprehensive Level of Consciousness Scale (CLOCS), Coma Recovery
Scale, Innsbruck Coma Scale, Reed’s Classification, etc., but the
predictive value of all these scalesremains to be ascertained. A practical
guide that can be easily applied and is quite reliable is mentioned in Table 3.5, which also has the
additional advantage that it takes into account not only CNS depressants
producing true coma, but also CNS stimulants which produce coma only in the
last stage.
There are numerous causes for coma of which one of the most important is acute poisoning. A number of substances can induce coma, and it will require a great deal of astuteness and expertise to pinpoint the poison. Before proceeding to an elaborate exercise in diagnosis however, it may be desirable to first ascertain for sure that the patient is really comatose and not just pretending (psychogenic or hysterical coma). This is often encountered in cases of “suicide gesture” in contrast to “attempted suicide”. The former is an attention drawing gambit, where there is no real intention of ending one’s life.
The telltale fluttering eyelids, the patient who
is half-walked, half-dragged in by relatives, an elaborate suicide note, a
phone call to a friend or relative informing them of the act, pill bottles
strewn about, all may point to such a suicide gesture. In addition, the signs
and symptoms manifested by the patient usually are out of proportion to the
ingestion itself.
So the question is, how does the
doctor humanely deter-mine whether the coma is true or fake? Several methods
have been recommended of which the following constitute barbaric acts and must
never be employed :
Pinching nipples or genitals, or
repeatedly pinching any part of the body.
Slapping the face hard, repeatedly.
Cotton pledgets or sterile
applicator tips soaked with ammonia solution being inserted into the nostrils.
Instead, the following steps are
recommended:
Perform a quick physical examination
with particular atten-tion to the breathing, vital signs, and the gag reflex.
If these are normal, the coma is almost certainly psychogenic. Another
indication is a tightly clenched jaw when attempts are made to open the mouth.
However, first rule out seizure disorders.
A useful technique is to lift the
patient’s hand directly above his face and letting it drop. A psychogenic
aetiology is almost a certainty if the hand falls gently to his side, rather
than obeying the law of gravity and landing on the face. Pinching the shoulder
may also be tried, but must not be repeated more than twice. Some clinicians
advocate rubbing the patient’s sternum with the knuckles of the clenched fist.
The key to successfully manage a
patient with psycho-genic loss of consciousness is to avoid humiliating the
patient in front of either relatives, friends, or hospital staff. Making it
known (loudly) to the patient that friends and relatives are waiting outside,
and that the poison should be “wearing off about now”, explaining what has to
be done and why infirm, non-emotional tone, and avoiding physical abuse or
humiliation will often enable the patient to “regain conscious-ness” over a
period of a few minutes with his dignity and self respect intact.
If the patient resists all the above
manoeuvres and the attending doctor is sure that he is dealing with a known
inges-tion that is harmless, it is better to leave the patient alone for
sometime. If however there is any doubt as to the seriousness of the ingested
substance, gastric lavage must be initiated ensuring all necessary precautions.
Related Topics