Chapter: Modern Medical Toxicology: General Principles: General Management of Poisoning
Decontamination - General Management of Poisoning
Decontamination
EYE
Irrigate
copiously for at least 15 to 20 minutes with normal saline or water. Do not use
acid or alkaline irrigating solutions. As a first-aid measure at home, a victim
of chemical burns should be instructed to place his face under running water or
in a shower while holding the eyelids open. During transportation to hospital
the face should be immersed in a basin of water (while ensuring that the patient
does not inhale water).
SKIN
Cutaneous absorption is a common
occurrence especially with reference to industrial and agricultural substances
such as phenol, hydrocyanic acid, aniline, organic metallic compounds,
phosphorus, and most of the pesticides. The following measures can be
undertaken to minimise absorption*—
■■ Exposed
persons should rinse with cold water and then wash thoroughly with a
non-germicidal soap. Repeat the rinse with cold water.
■■ Corroded
areas should be irrigated copiously with water or saline for at least 15
minutes. Do not use “neutralising solutions”.
■■ Remove
all contaminated clothes. It is preferable to strip the patient completely and
provide fresh clothes, or cover with clean bedsheet.
■■ Some
chemical exposures require special treatment :
· Phenolic burns should be treated by
application of polyethylene.
· Phosphorus burns should be treated
with copper sulfate solution.
· For hydrofluoric acid burns, use of
intradermal or intra-arterial calcium gluconate decreases tissue necrosis.
· For tar, bitumen, or asphalt burns,
first irrigate the affected skin with cold water and then clean and apply
solvents such as kerosene, petrol, ethanol, or acetone. However, since these
substances can not only be locally cytotoxic, but also be absorbed through the
skin, it is preferable to use mineral oil, petrolatum, or antibacte-rial
ointments in a petrolatum base. Prolonged irrigating applications may be
required.
GUT
The various methods of poison
removal from the gastrointes-tinal tract include:
■■ Emesis
■■ Gastric
lavage
■■ Catharsis
■■ Activated
charcoal
■■Whole bowel irrigation
Emesis
The
only recommended method of inducing a poisoned patient to vomit is
administration of syrup of ipecacuanha
(or ipecac). However, the initial
enthusiasm associated with the use of ipecac in the 1960s and 1970s in western
countries has declined substantially in recent years owing to doubts being
raised as to its actual efficacy and safety. The current consensus is thatsyrup of ipecac must NOT be used, except
in justifiable circumstances.
Syrup of Ipecac
·
Source—Root of a small shrub (Cephaelis ipecacuanha or C. acuminata) which grows well in West
Bengal (Fig 3.1).
·
Active principles: Cephaeline,
emetine, and traces of psychotrine.
·
Indications: Conscious and alert
poisoned patient who has ingested a poison not more than 4 to 6 hours earlier.
·
Mode of action:
o Local
activation of peripheral sensory receptors in the gastrointestinal tract.
o Central
stimulation of the chemoreceptor trigger zone with subsequent activation of the
central vomiting centre.
·
Dose:
o
30 ml (adult), or 15 ml (child), followed by 8 to 16 ounces,
i.e. 250 to 500 ml approximately, of water.
o
The patient should be sitting up.
o
If vomiting does not occur within 30 minutes, repeat the
same dose once more. If there is still no effect, perform stomach wash to
remove not only the ingested poison but also the ipecac consumed. However the therapeutic doses of ipecac
recommended above are not really harmful.
■■ Contra-indications:
·
Relative
:
––
Very young (less than 1 year), or very old patient –– Pregnancy
–– Heart disease
–– Bleeding diathesis
–– Ingestion of cardiotoxic poison
–– Time lapse of more than 6 to 8 hours
·
Absolute
:
––
Convulsions, or ingestion of a convulsant poison –– Impaired gag reflex
–– Coma
––
Foreign body ingestion –– Corrosive ingestion
––
Ingestion of petroleum distillates, or those drugs which cause altered mental
status (phenothiazines, antihistamines, opiates, ethanol, benzodiazepines,
tricyclics).
––
All poisons which are themselves emetic in nature
·
Complications:
Cardiotoxicity (bradycardia, atrial
fibrillation, myocar- ditis).
Aspiration pneumonia.
Oesophageal mucosal or Mallory Weiss tears
(due toprotracted vomiting).
Other Emetics
The only other acceptable method of
inducing emesis that is advocated involves the use of apomorphine. Given subcu-taneously, it causes vomiting within 3 to
5 minutes by acting directly on the chemoreceptor trigger zone. The recommended
dose is 6 mg (adult), and 1 to 2 mg (child). Since apomorphine is a respiratory
depressant it is contraindicated in all situations where there is likelihood of
CNS depression.
In some cases, stimulation of the posterior pharynx with a finger or a blunt
object may induce vomiting by provoking the gag reflex. Unfortunately, such
mechanically induced evacua-tion is often unsuccessful and incomplete, with
mean volume of vomitus about one third of that obtained by the other two
methods.
Obsolete Emetics
The
use of warm saline or mustard water as an emetic is not only
dangerous (resulting often in severe hypernatraemia), but also impractical
since many patients, especially children refuse (fortunately) to drink this
type of concoction and much valuable time is lost coaxing them to do so. One
tablespoon of salt contains at least 250 mEq of sodium, and if absorbed can
raise the serum level by 25 mEq/L in for instance, a 3-year old child.* It is
high time that the use of salt water as an emetic be deleted once and for all
from every first-aid chart or manual on poisoning.
Copper sulfate induces
emesis more often than commonsalt, but significant elevations of serum copper
can occur leading to renal and hepatic damage. It is also a gastrointestinal
corrosive.
Zinc sulfate is
similar in toxicity to copper sulfate, and hasin addition a very narrow margin
of safety.
Gastric Lavage (Stomach Wash)
The
American Academy of Clinical Toxicology (AACT), and the European Association of
Poison Centres and Clinical Toxicology (EAPCCT) have prepared a draft of a
position paper directed to the use of gastric lavage, which suggests that
gastric lavage should not be employed routinely in the management of poisoned
patients. There is no certain evidence that its use improves outcome, while the
fact that it can cause significant morbidity (and sometimes mortality) is
indisputable. Lavage should be considered only if a patient has ingested a
life-threatening amount of a poison and presents to the hospital within 1 to 2
hours of ingestion.
But
in India, very often caution is thrown to the wind and the average physician in
an average hospital embarks on gastric lavage with gusto the moment a poisoned
patient is brought in. A sad commentary on the existing lack of awareness and a
reluctance to change old convictions in spite of mounting evidence against the
routine employment of such “established procedures”.
■■ Indications—
·
Gastric lavage is recommended mainly for patients whohave
ingested a life-threatening dose, orWho exhibit significant morbidity and
present within1 to 2 hours of ingestion. Lavage beyond this periodmay be
appropriate only in the presence of gastricconcretions, delayed gastric
emptying, or sustainedrelease preparations. Some authorities still
recommendlavage upto 6 to 12 hours post-ingestion in the case ofsalicylates,
tricyclics, carbamazepine, and barbiturates
·
Precautions—
o
Never undertake lavage in a patient who has ingested a
non-toxic agent, or a non-toxic amount of a toxic agent.
o
Never use lavage as a deterrent to subsequent inges- tions.
Such a notion is barbaric, besides being incorrect.
·
Contraindications—
o
Relative: Haemorrhagic diathesis,
oesophageal varices, recent surgery, advanced pregnancy, ingestion of alkali,
coma.
o
Absolute: Marked hypothermia, prior
significant vomiting, unprotected airway in coma, and ingestion of acid or
convulsant or petroleum distillate, and sharp substances.
·
Procedure—
o Explain the exact procedure to the
patient and obtain his consent. If refused, it is better not to undertake
lavage because it will amount to an assault, besides increasing the risk of
complications due to active non-co-operation.
o Endotracheal
intubation must be done prior to lavage in the comatose patient.
o Place
the patient head down on his left lateral side (20o tilt
on the table).
o Mark
the length of tube to be inserted (50 cm for an adult, 25 cm for a child).*\
o The
ideal tube for lavage is the lavacuator
(clear plastic or gastric hose).
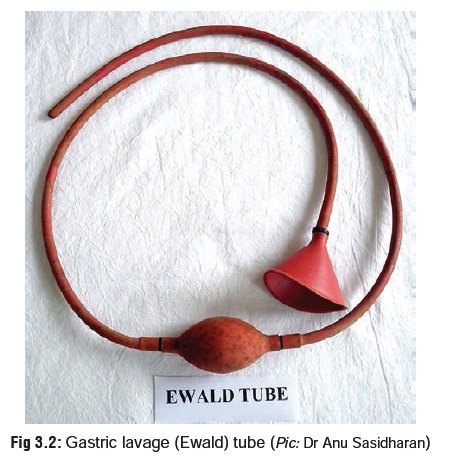
o In India however, the Ewald tube is most often used which is a soft rubber tube with a funnel at one end (Fig 3.2). Whatever tube is used, make sure that the inner diameter corresponds to at least 36 to 40 French size.** A nasogastric tube used for gastric aspiration is inadequate and should never be used. In a child, the diameter should be at least 22 to 28 French, (Ryle’s tube may be sufficient – Fig 3.3).
o The
preferred route of insertion is oral. Passing the tube nasally can damage the
nasal mucosa considerably and lead to severe epistaxis. Lubricate the inserting
end of the tube with vaseline or glycerine, and pass it to the desired extent.
Use a mouth gag so that the patient will not bite on the tube.
o Once
the tube has been inserted, its position should be checked either by air
insufflation while listening over the stomach, or by aspiration with pH testing
of the aspirate, (acidic if properly positioned).
o Lavage
is carried out using small aliquots (quantities) of liquid. In an adult, 200 to
300 ml aliquots of warm (38o C) saline
or plain water are used. In a child, 10 to 15 ml/kg body weight of warm saline
is used each time. Water should preferably be avoided in young children because
of the risk of inducing hyponatraemia and water intoxication. It is advisable
to hold back the first aliquot of washing for chemical analysis.
o In
certain specific types of poisoning, special solutions may be used in place of
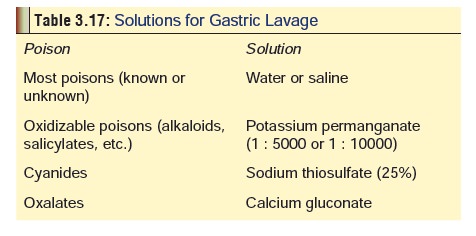
water or saline (Table 3.17).
o Lavage
should be continued until no further particulate matter is seen, and the
efferent lavage solution is clear. At the end of lavage, pour a slurry of
activated charcoal in water (1 gm/kg), and an appropriate dose of an ionic
cathartic into the stomach, and then remove the tube.
Complications –
·
Aspiration pneumonia.
·
Laryngospasm.
·
Sinus bradycardia and ST elevation
on the ECG.
·
Perforation of stomach or oesophagus
(rare).
Catharsis
Catharsis is a very appropriate term when used in connection with poisoning, since it means purification. It is achieved by purging the gastrointestinal tract (particularly the bowel) of all poisonous material.
The
two main groups of cathartics* used in toxicology include
·
Ionic
or Saline:
––
These cathartics alter physico-chemical forces within the intestinal lumen
leading to osmotic retention of fluid which activates motility reflexes and
enhances expulsion. However, excessive doses of magnesium-based cathartics can
lead to hypermagnesaemia which is a serious complication.
––
The doses of recommended cathartics are as follows:
-- Magnesium citrate: 4 ml/kg
--
Magnesium sulfate: 30 gm (250 mg/kg in a child)
-- Sodium sulfate: 30 gm (250 mg/kg in a child).
·
Saccharides:
––
Sorbitol (D-glucitol) is the cathartic of choice in adults because of better
efficacy than saline cathartics, but must not be used as far as possible in
young children owing to risk of fluid and electrolyte imbalance (especially
hypernatraemia).
––
It occurs naturally in many ripe fruits and is prepared industrially from
glucose, retaining about 60% of its sweetness. Sorbitol is used as a sweetener
in some medicinal syrups, and the danger of complications is enhanced in
overdose with such medications when sorbitol is used as a cathartic during
treatment.
–– Dose of sorbitol: 50 ml of 70% solution
(adult).
·
Efficacy of catharsis:
While
cathartics do reduce the transit time of drugs in the gastrointestinal tract,
there is no real evidence that it improves morbidity or mortality in cases of
poisoning.
·
Contraindications:
–– Corrosives
––
Existing electrolyte imbalance
––
Paralytic ileus
–– Severe diarrhoea
––
Recent bowel surgery
––
Abdominal trauma
––
Renal failure.
Oil
based cathartics should never be used in poisoning since they increase the risk
of lipoid pneumonia, increase the absorption of fat soluble poisons, and
inactivate medicinal charcoal’s effects when administered along with them. The
last mentioned reason also applies to conventional laxatives, and hence they
are also not recommended in poisoning.
Activated (Medicinal) Charcoal
A
number of studies have documented clearly the efficacy of activated charcoal as
the sole decontamination measure in ingested poisoning, while emesis and lavage
are increasingly being associated with relative futility.
Activated
charcoal is a fine, black, odourless, tasteless powder (Fig 3.4) made from burning wood, coconut shell, bone, sucrose, or
rice starch, followed by treatment with an activating agent (steam, carbon
dioxide, etc.). The resulting particles are extremely small, but have an
extremely large surface area. Each gram of activated charcoal works out to a
surface area of 1000 square metres.

·
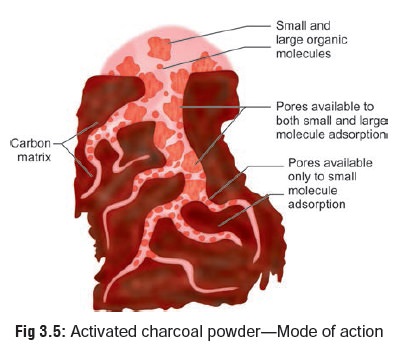
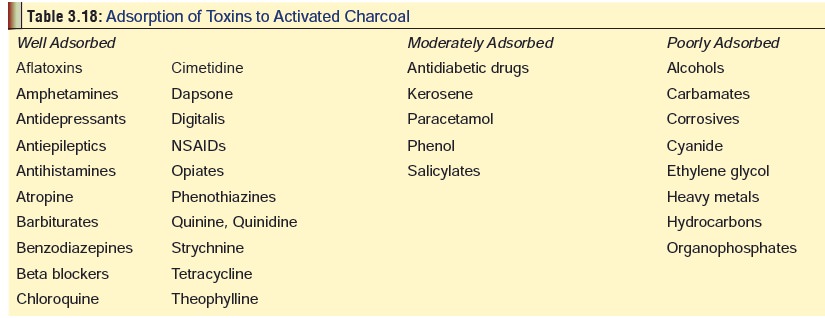
Mode of action—
Decreases
the absorption of various poisons by adsorbing them on to its surface (Fig 3.5). Activated charcoal is
effec-tive to varying extent, depending on the nature of substance ingested (Table 3.18).
·
Dose—
1 gm/kg body
weight (usually 50 to 100 gm in an adult, 10 to 30 gm in a child).
·
Procedure—
·
Activated charcoal is most effective
when administered within one hour of ingestion. Administration in the prehospital setting has the potential to
significantly decrease the time from toxin ingestion to activated charcoal
administration, although it has not been shown to affect outcome.
·
Add four to eight times the quantity
of water to the calculated dose of activated charcoal, and mix to produce a
slurry or suspension. This is administered to the patient after emesis or
lavage, or as sole inter- vention. The slurry should be shaken well before
administration.
Multiple-dose Activated Charcoal: The use of repeated doses
(amounting to 150 to 200 gm of activated charcoal) has been demonstrated to be
very effective in the elimination of certain drugs such as theophylline,
phenobarbitone, quinine, digitoxin, phenylbutazone, salicylates and
carbamazepine. The actual dose of activated charcoal for multiple dosing has
varied consider- ably in the available medical literature, ranging from 0.25 to
0.5 gm/kg every 1 to 6 hours, to 20 to 60 gm for adults every 1, 2, 4, or 6
hours. The total dose administered is more important than frequency of
administration.
·
Disadvantages—
o Unpleasant
taste*
o Provocation
of vomiting
o Pulmonary
aspiration
o Intestinal
obstruction (especially with multiple-dose activated charcoal).
·
Contraindications—
o Absent
bowel sounds or proven ileus
o Small
bowel obstruction
o Caustic
ingestion
o Ingestion
of petroleum distillates.
Whole Bowel Irrigation (Whole Gut Lavage)
This
is a method that is being increasingly recommended for late presenting
overdoses when several hours have elapsed since ingestion. It involves the
instillation of large volumes of a suit-able solution into the stomach in a
nasogastric tube over a period of 2 to 6 hours producing voluminous diarrhoea.
Previously, saline was recommended for the procedure but it resulted in
electrolyte and fluid imbalance. Today, special solutions are used such as PEG-ELS ( i.e. polyethylene glycol and
electro-lytes lavage solution combined together, which is an isosmolar
electrolyte solution), and PEG-3350
(high molecular weight polyethylene glycol) which are safe and efficacious,
without producing any significant changes in serum electrolytes, serum
osmolality, body weight, or haematocrit.
·
Indications—
·
Ingestion of large amounts of toxic
drugs in patients presenting late ( > 4 hours post-exposure)
·
Overdose with sustained-release
preparations.
·
Ingestion of substances not adsorbed
by activated char- coal, particularly heavy metals.
·
Ingestion of foreign bodies such as
miniature disc batteries (button cells), cocaine filled packets (body packer syndrome),** etc.
·
Ingestion of slowly dissolving
substances: iron tablets, paint chips, bezoars, concretions, etc.
·
Procedure—
·
Insert a nasogastric tube into the
stomach and instil one of the recommended solutions at room temperature, at a
rate of 2 litres per hour in adults, and 0.5 litre per hour in children. The
patient should preferably be seated in a commode. The use of metoclopramide IV,
(10 mg in adults, 0.1 to 0.3 mg/ kg in children) can minimise the incidence of
vomiting. The procedure should be continued until the rectal effluent is clear,
which usually occurs in about 2 to 6 hours.
·
Complications—
o Vomiting
o Abdominal
distension and cramps
o Anal
irritation.
·
Contraindications—
o Gastrointestinal
pathology such as obstruction, ileus, haemorrhage, or perforation.
Related Topics