Chapter: Modern Medical Toxicology: General Principles: General Management of Poisoning
Evaluation - General Management of Poisoning
Evaluation
In all those poisoned patients where there appears to be no immediate crisis, a detailed and thorough clinical examination should be made with special reference to the detection and treatment of any of the following abnormalities :
Hypothermia
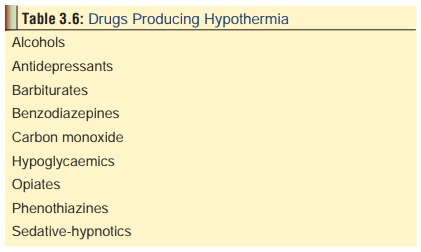
Some
common drugs which produce hypothermia are mentioned in Table 3.6. It is essential to use a low reading rectal thermometer.
Electronic thermometers with flexible probes are best which can also be used to
record the oesopha-geal and bladder temperatures.
Treatment:
·
Rewarming
o
For mild cases, a warm water bath (115oF) is
sufficient until the core temperature rises to 92o F, when the
patient is placed in a bed with warm blankets. The rate of rewarming should not
exceed 5o F per hour.
o
Heating the inspired air is recommended by some as very
effective in raising the core temperature.
o
Others advocate gastric lavage with warmed fluids, or
peritoneal lavage with warmed dialysate.
·
In addition, it may be necessary to correct other associated
anomalies such as hypotension, hypoventilation, acidosis,and hypokalaemia.
Hyperthermia
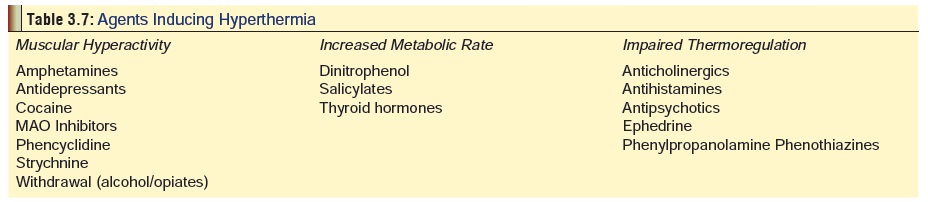
Oral temperature above 102oF is referred to as hyperthermia.If it exceeds 106oF (which is very rare), there is imminent danger of encephalopathy. In a few individuals there is a danger of encephalopathy. In a few individuals there is a genetic susceptibility to hyperthermia, especially on exposure to skeletal muscle relaxants, inhalation anaesthetics, and even local anaesthetics—malignant hyperthermia. This should be distinguished from neuroleptic malignant syndrome, which is also characterised by high fever apart from other neurological signs, but is the result of adverse reaction to antipsychotic or neuroleptic drugs, and has no genetic basis. Table 3.7 lists some of the important toxicological causes of hyperthermia along with postulated mechanism. Complications include coagulopathy, rhabdomyolysis, renal failure, and tachyarrhythmias.
Treatment :
·
Remove all clothes, and pack the neck and groin with ice.
·
Immersion in cold water bath (77oF) is very effective
but dangerous in the elderly and in heart patients.
·
Stop cooling measures when core temperature falls below 102oF,
and nurse the patient in bed in a cool room.
·
Administration of dantrolene may be beneficial in some
cases.
·
Do not use antipyretic drugs like paracetamol. They are
ineffective.
Acid-Base Disorders
Serum electrolytes to evaluate for metabolic acidosis should be obtained if there is any possibility of mixed ingestion or based on arterial blood gas, pH, PaCO2, bicarbonate, and serum electrolyte disturbances.
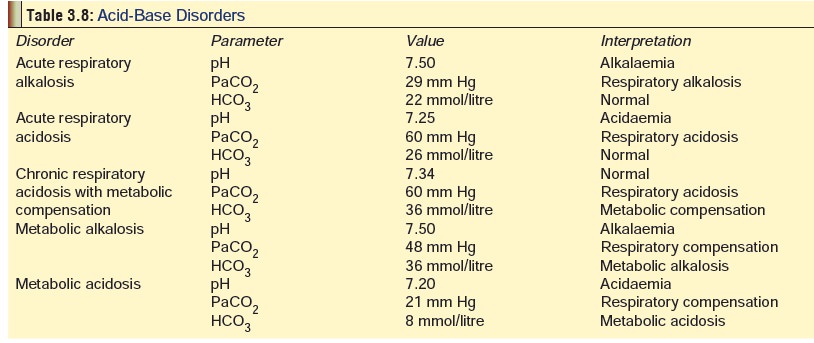
It must be
first determined as to which abnormalities are primary and which are
compensatory, based on the pH (Table 3.8).
If the pH is less than 7.40, respiratory or metabolic alkalosis is primary.
In the case of metabolic acidosis,
it is necessary to calculate the anion
gap. The anion gap is calculated as follows:
(Na+ + K+)–(HCO3-
+ Cl-)
Normally this translates as 140–(24
+ 104) = 12 mmol/L (Range: 12 to 16
mmol/L)
If the anion gap is greater than 20
mmol/L, a metabolic acidosis is present regardless of the pH or serum
bicarbonate concentration. Several poisons are associated with increased anion
gap (Gap acidosis), while others do
not alter it (Non- gap acidosis).
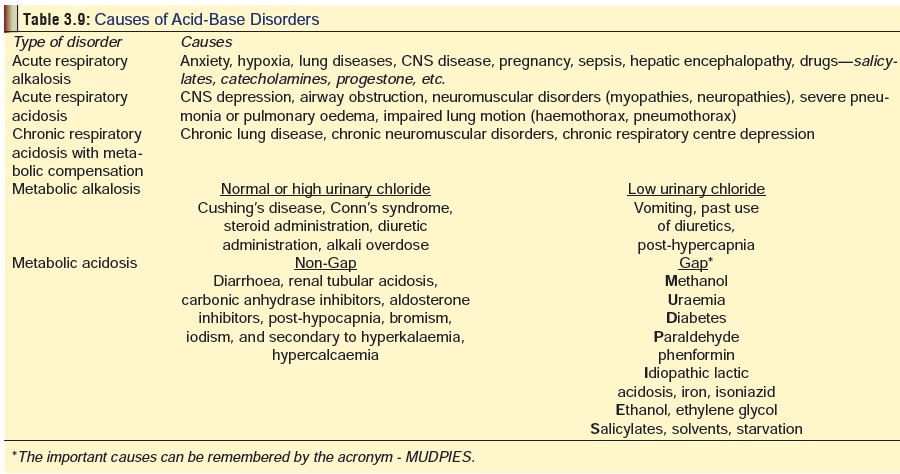
The common causes for the various acid-base disorders are mentioned in Table 3.9. Treatment of metabolic acidosis:
The drug of choice is sodium
bicarbonate. It is widely considered to be the best antidote for acidosis of
almost any aetiology.
Convulsions (Seizures)
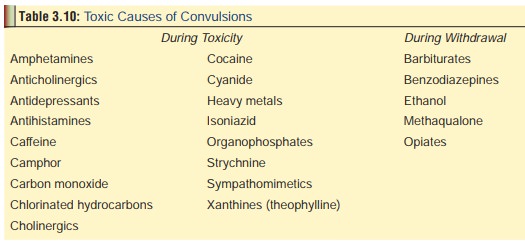
There
are several drugs and poisons which cause convulsions (Table 3.10). Improper treatment or mismanagement can lead to status
epilepticus which is a life-threatening condition.
Treatment:
·
Administer oxygen by nasal cannula
or mask.
·
Position patient’s head for optimal
airway patency.
·
Establish IV line.
·
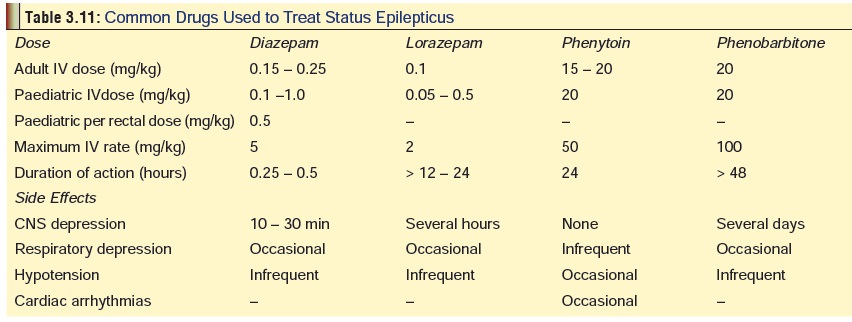
Begin drug therapy with
benzodiazepines (Table 3.11).
·
Either lorazepam (0.1 mg/kg) at a
rate of 2 mg/min,or diazepam (0.2 mg/kg) at a rate of 5 mg/min can be
administered IV. If status persists, administer 15–20 mg/kg phenytoin at 50
mg/min (adults), or 1 mg/kg/min (children), by IV.*
·
If status still persists, administer
20 mg/kg phenobarbitone IV at 100 mg/min. If this measure also fails, give
anaes-thetic doses of phenobarbitone, pentobarbitone, thiopen-tone, or
halothane. In such cases obviously, ventilator assistance and vasopressors
become mandatory.
·
Monitor ECG, hydration, and
electrolyte balance. Watch out for hypoglycaemia and cerebral oedema.
Box 3.1 Sodium Bicarbonate
Uses :
·
Salicylate overdose (to alkalinise
urine)
·
Tricyclic antidepressant overdose (to
alkalinise blood)
·
Correction of metabolic acidosis
(especially in methanol and ethylene glycol poisoning)
·
Adjuvant in poisoning with
barbiturates, phenothiazines, cocaine, and carbamazepine
·
Drug or toxin-induced myoglobinuria
·
As stomach wash for iron poisoning
·
Possible use in lactic acidosis,
diabetic keto-acidosis, and cardiac resuscitation
Formulation :
·
50 ml ampoules of 8.4 and 7.5% solution
containing 50 and 44.6 mEq of sodium bicarbonate respectively.
Dose :
·
Add 2 to 3 ampoules of 8.4% NaHCO3
to 1 litre of 5% dextrose in water, infused intravenously over 3 to 4 hours. In
paediatric patients, add 1 to 2 mEq NaHCO3/Kg in 15 ml/Kg 5%
dextrose on 0.45% normal saline over 3 to 4 hours.
·
Check urine pH in 1 hour. It should be
at least 7.5, preferably 8. Maintain alkalinisation with continuous infusion of
100 to 150 mEq in 1 litre of 5% dextrose in water at 150 to 200 ml/hr. Half of
this dose suffices for a child.
Mechanism of action :
·
Alters drug ionisation of weak acids.
Alkalinisation of blood prevents movement of ionised drug within the tissues.
Cellular membranes are impermeable to ionised compounds.
·
Changes sodium gradients and partially
reverses the fast sodium channel blockade seen especially in tricyclic
antidepressant overdose.
·
Titrates acid, and reverses
life-threatening acidaemia.
Dangers :
·
Can precipitate fatal arrhythmia if
given in the presence of hypokalaemia.
·
Can result in alkalaemia, if
administered negligently.
Agitation
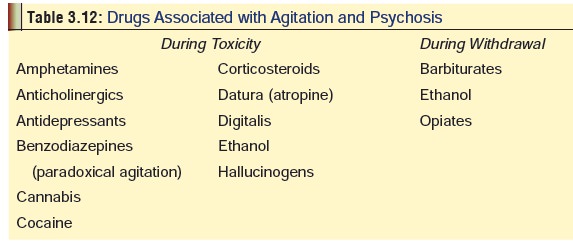
Several drugs and poisons are
associated with increased aggression which may sometimes progress to psychosis
and violent behaviour (Table 3.12).
This is especially likely if there are other predisposing factors such as
existing mental disorder, hypoglycaemia, hypoxia, head injury, and even anaemia
and vitamin deficiencies. Delirium
is the term which is often used to denote such acute psychotic episodes, and is
characterised by disorientation, irrational fears, hyperexcit-ability,
hallucinations, and violence. Dementia
refers to a more gradual decline in mental processes mainly resulting in
confusion and memory loss, and though it is often organic in nature due to
degenerative diseases, there are some drugs which can cause this especially on
chronic exposure. Elderly patients are more vulnerable. Dementia due to drugs
is usually reversible.
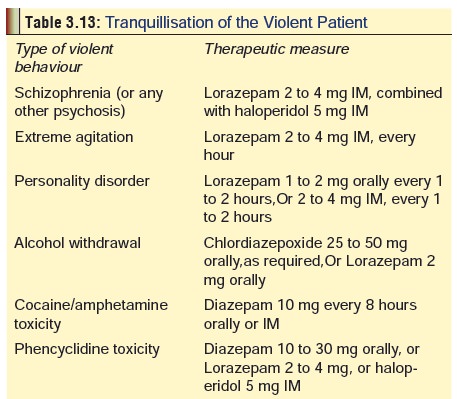
Treatment :
Delirium is managed by
chlorpromazine, diazepam, or haloperidol. Caution is however necessary, since
sedation which is inevitable with these preparations may sometimes result in
more harm than benefit. Table 3.13
outlines measures for managing a violent patient in the casualty (Emergency
department).
Movement Disorders
Exposure to several drugs and toxins can result in a wide variety of movement disorders ranging from full blown Parkinson’s disease to isolated tremors. The most frequent culprits for parkinsonian manifestations are phenothiazines and majortranquillisers, though there are several others which have also been implicated. Symptoms of Parkinsonism usually appear in the first three months of exposure and may be indistinguishable from idiopathic Parkinson’s disease.
Drug-induced myopathies may result from a direct toxic effect which may be local
(e.g. injection of drug into muscle), or more diffuse when the drug is taken
systemically. Repeated injections of antibiotics or drugs of addiction often
lead to severe muscle fibrosis and contractures (myositis fibrosa,myositis ossificans). Clofibrate and aminocaproic
acid cancause an acute necrotising
myopathy with myoglobinuria and renal failure. Other drugs that can induce
toxic myopathies ![]() include succinylcholine, halothane, corticosteroids,
chloroquine, D-penicillamine, alcohol, phenytoin, thiazide diuretics,
ampho-tericin, procainamide, penicillin, and lipid-lowering drugs.
Environmental causes include exposure to silica, certain types of food (e.g.
adulterated rape seed oil), and medical devices such as silicone implants.
include succinylcholine, halothane, corticosteroids,
chloroquine, D-penicillamine, alcohol, phenytoin, thiazide diuretics,
ampho-tericin, procainamide, penicillin, and lipid-lowering drugs.
Environmental causes include exposure to silica, certain types of food (e.g.
adulterated rape seed oil), and medical devices such as silicone implants.
Tricyclic antidepressants, monoamine
oxidase inhibitors, fluoxetine, lithium, buspirone, and levadopa are the
principal causes of drug-induced akathisia.
This is characterised by extreme restlessness with constant movement and
muscular quivering. Dystonia usually
manifests as facial grimacing or torticollis, and is mainly associated with
phenothiazines, buty-rophenones, metoclopramide, tricyclic antidepressants,
pheny-toin, and chloroquine. Chorea,
which causes involuntary writhing movements of limbs is most commonly seen with
anticonvul-sants (especially phenytoin), anabolic steroids, amphetamines,
levodopa, and sometimes with cimetidine, ethanol, and cocaine. Phenothiazines
and metoclopramide are most often the culprits in drug-induced tardive dyskinesia, which is
characterised by stereotyped, slow, rhythmic movements.
Myasthenic crisis, a sudden onset of severe
muscularweakness, may be precipitated by aminoglycosides, polymyxin,
penicillamine, tetracycline, quinidine, lignocaine, quinine, curare,
succinylcholine, procainamide, and some opiates.
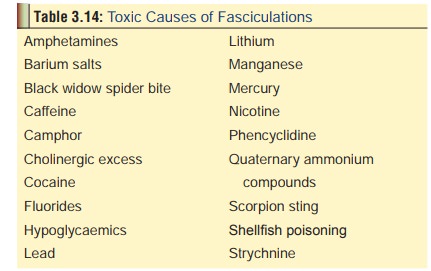
Fasciculations are contractions of muscle fibres withinan individual motor
unit, and appear as twitching of affected muscles. Table 3.14 lists the major toxicological causes of fasciculations.
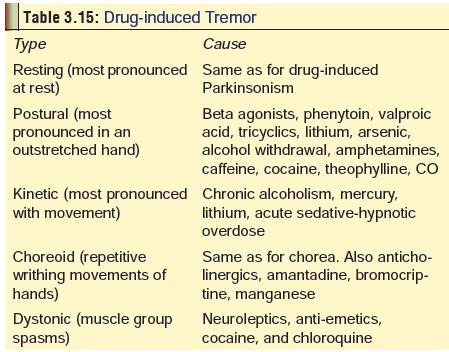
Drug induced tremors are of several
types, and are listed in Table 3.15.
Treatment of movement disorders:
Most of the movement disorders
induced by toxins or drugs are dose and duration related. Withdrawal of the
incriminating agent commonly results in recovery. The usual measures
under-taken in the management of the respective drug overdose (or abuse) must
be instituted wherever applicable.
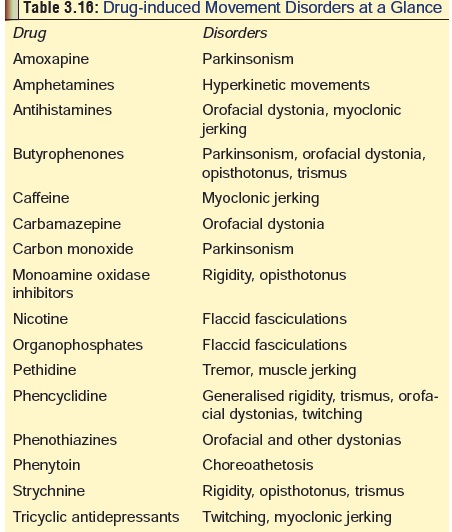
Table 3.16 will serve as a quick reference source forcommon culprits of
drug or toxin induced movement disorders.
Electrolyte Disturbances
1. Hyperkalaemia—(i.e. potassium level more than 5.5 mEq/L)The causes include digitalis, beta-2 antagonists, potassium sparing diuretics, NSAIDs, fluoride, heparin, succinylcholine, and drugs producing acidosis. Manifestations include abdominal pain, diarrhoea, myalgia, and weakness. ECG changes are impor-tant – tall, peaked T waves, ST segment depression, prolonged PR interval, and QRS prolongation. In severe cases there is ventricular fibrillation.
Treatment: Glucose, insulin
infusion, sodium bicarbonate, and calcium gluconate. Haemodialysis and exchange
resins may be required.
2. Hypokalaemia—(i.e. potassium level less than 3.5
mEq/L)
The causes include beta2
agonists, theophylline, insulin, chloroquine, caffeine, dextrose, loop
diuretics, thiazide diuretics, oral hypoglycaemics, salicylates,
sympathomi-metics, drug-induced gastroenteritis, and metabolic acidosis.
Manifestations include muscle weakness, paralytic ileus, and ECG changes—flat
or inverted T waves, prominent U waves, ST segment depression. In severe cases
there is A-V block and ventricular fibrillation.
Treatment: Oral or IV potassium.
3. Hypernatraemia—(i.e. sodium level more than 150
mEq/L)
The
causes include colchicine, lithium, propoxyphene, rifampicin, phenytoin,
alcohol, mannitol, sorbitol, sodium salts, excessive water loss, IV saline
solutions, and salt emetics.
Treatment:
Water restriction with or without loop diuretics.
4. Hyponatraemia—(i.e., sodium level less than 130
mEq/L)The causes include carbamazepine, chlorpropamide, NSAIDs, amitryptiline, biguanides, sulfonylureas, captopril and
other ACE inhibitors, lithium, imipramine, oxytocin, and excessive water intake.
Treatment: Hypertonic saline.
5. Hypocalcaemia—(i.e. calcium level less than 4
mEq/L)The causes include hydrogen fluoride, oxalates, amino- glycosides, ethanol, phenobarbitone,
phenytoin, theophylline, and ethylene glycol.
Treatment: Calcium gluconate IV (10%
solution, 10 ml at a time, slowly).
Drug-induced hypercalcaemia is uncommon.
Related Topics