Chapter: Essentials of Psychiatry: Sexual Disorders
Sexual Disorders: The Sexual Dysfunctions
The Sexual Dysfunctions
Significance of Sexual Dysfunction
While sex is widely thought of as recreation, psychiatrists rec-ognize
it as an important means of establishing and reaffirming emotional attachments.
Sexual competence – the ability to desire a partner, become aroused and attain
orgasm in a cooperative manner when together – is a valuable developmental
accom-plishment because it enables a person to experience the physical
expressions and emotional complexities of love. Mutually pleas-urable sexual
behavior tends to recur far more often in couples than unilaterally satisfying
behavior. Mutually pleasurable sex-ual behavior allows both partners to be
comforted and stabilized by loving and feeling loved. The dysfunctions are
symptomatic deficits in the quest for these widespread ideals: sexual compe-tence,
fun and stabilization of the self.
DSM-IV Diagnoses
DSM-IV specifies three criteria for each sexual dysfunction (American
Psychiatric Association, 1994). The first criterion describes the
psychophysiologic impairment – for example, ab-sence of sexual desire, arousal,
or orgasm. The second and third criteria are the same for each impairment: the
dysfunction causes marked distress or interpersonal difficulty and the
dysfunction is not better accounted for by another Axis I diagnosis or not due
exclusively to the direct physiological effects of a substance (e.g., a drug of
abuse, a medication) or a general medical condition. Table 57.2 lists the first
criterion of each of the 12 sexual dysfunc-tion diagnoses. DSM-IV gives the
clinician additional latitude
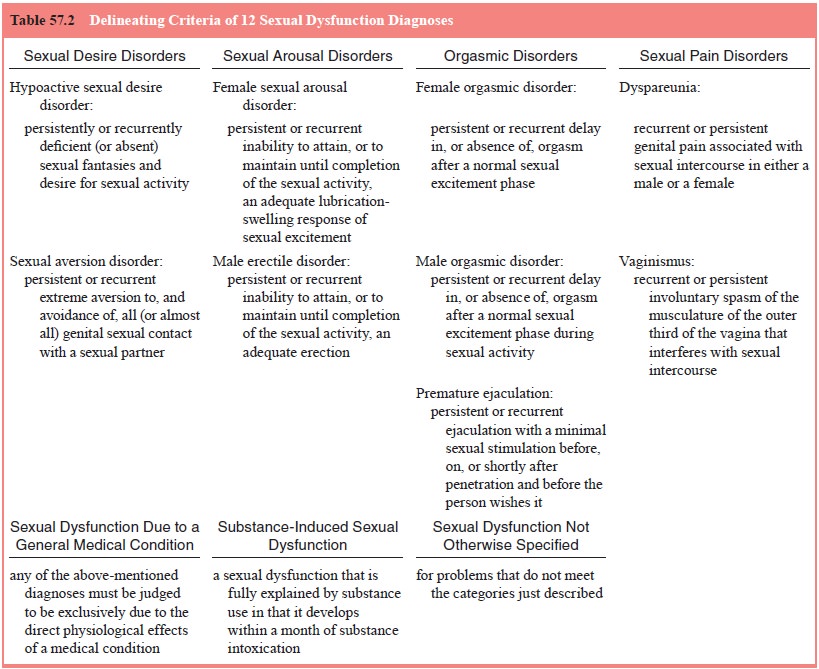
for deciding when a person who meets the first criterion qualifies for a
disorder. The doctor is asked to consider the effects of the individual’s age,
experience, ethnicity and cultural background, the degree of subjective
distress, adequacy of sexual stimulation and symptom frequency. No instructions
are provided about how to exercise this judgment. In this way DSM-IV makes it
clear that understanding sexual life requires more than counting symptoms; it
requires judgment.
Epidemiology
Numerous attempts to describe the prevalence of sexual dys-function have
been made in the previous 25 years. These range from attempts to define the
frequency of a particular dysfunc-tion, for instance male erectile disorder, to
attempts to esti-mate the prevalence of a series of separate dysfunction, for
example, desire, arousal and orgasmic disorders of women. All such efforts
quickly confront methodological influences of sampling, means of obtaining the
information, definition of each dysfunction, purpose of the study and
perspective of its authors. These data not surprisingly, therefore, demonstrate
a range of prevalence depending on the problem studied. Gender identity
disorders are relatively rare (,1–2%).
Lifelong sexual desire disorders among women may involve 15% but are less
frequent among men. Acquired desire disorders among older individuals are
probably three times as common. Perhaps more than half of women at age 55 years
have recognized a deterio-ration in their sexual function. Perhaps 25% of women
in their twenties have difficulty having orgasm and 33% of men less than age 40
claim to ejaculate too rapidly. The majority of men by age 70 years are likely
to be having erection problems. The recent careful epidemiologic study,
designed by sociologists, successfully generated a representative sample of the
USA (Laumann et al., 1994a). They
interviewed men and women between age 18 and 59 years and found that sexual
dysfunc-tion is common, particularly among young women and older men. This is
noteworthy for psychiatrists because our stud-ies of sexual dysfunction caused
by medications or acquired psychiatric disorders tend to assume that patients
are gener-ally functionally intact prior to becoming ill or taking
medica-tions. This assumption is not tenable based on a generation of
epidemiologic studies.
Sexual Equilibrium
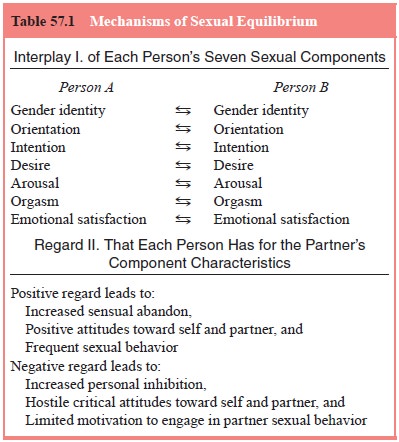
Etiologic ideas about sexual dysfunction are a relatively simple
conceptual challenge involving notions about the individual’s psychology and
his or her cultural expectations. In contrast, for couples, they involve two
individual psychologies, their interpersonal impact on one another and their
cultures. The cli-nician must be wary when one coupled person is presented as
having a sexual dysfunction and the partner is presented as “nor-mal”. Sexual
dysfunction in a couple is a two-person problem in terms of immediate effects
and often in terms of cause as well (Table 57.1). How a partner regards the
sexual characteristics of the other is a subtle ingredient of sexual comfort,
competence and dysfunction. For instance, a young woman’s new inability to
attain orgasm with her husband may be traced to her embarrass-ment at sharing
her excitation with him because she perceives him to be generally critical of
her. Similarly, the origin of a hus-band’s erectile dysfunction may be traced
to the emergence of his wife’s negative regard for him, which stemmed from
something other than his sexual behavior. This ordinary connectivity of a couple’s sexual function is referred to
as the couple’s sexual equilibrium (Levine, 1998). The sexual equilibrium
explains five observations:
·
Improvement and deterioration of
sexual function can rapidly occur;
·
When a couple’s nonsexual
relationship is good, their sexual life may not be;
·
Individual psychotherapy is often
insufficient to help coupled patients improve their sexual life;
·
A negative attitude from the
partner can block improvement in a couple’s sexual life regardless of the
therapy format and therapist skill;
·
A conversation with a therapist
who is attuned to the emotional meanings of a couple’s interaction can shift a
dysfunctional equilibrium back to mutually satisfying sexual behavior
The Problems of Sexual Desire
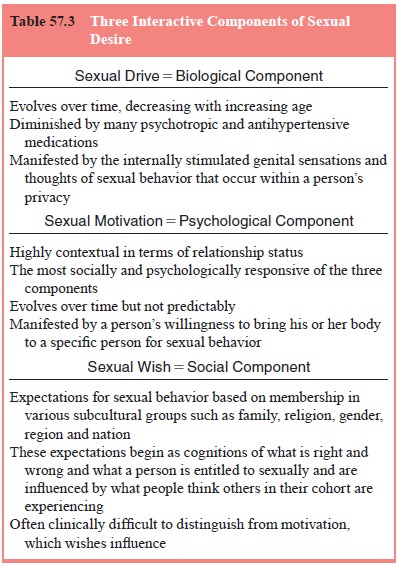
Sexual desire manifestations are diverse: erotic fantasies, sexual
dreams, initiation of sexual behavior, receptivity to partner-initiated sexual
behavior, masturbation, genital sensa-tions, heightened responsivity to erotic
environmental cues and sincere statements about wanting to behave sexually. For
most of the 20th century, these have been referred to as manifestations of
libido. Psychiatrists spoke of libido as if it was a homogeneous instinctive
force. Clinicians will find it far more useful to concep-tualize that the
diverse and changeable desire manifestations are produced by the intersection
of three mental forces: drive (biol-ogy), motive (psychology) and wish
(culture).
Drive
By only partially understood psychoneuroendocrine mecha-nisms, the preoptic
area of the anterior-medial hypothalamus and the limbic system periodically
produce sexual drive. Drive is
recognized by genital tingling, heightened responsivity to erotic environmental
cues, plans for self or partner sexual behavior, nocturnal orgasm and increased
erotic preoccupations. These are often spontaneous. Although people can become
aroused and at-tain orgasm without evident drive, it propels the entire sexual
psychophysiological process. Without drive, the sexual response system is far less
efficient and capable. While men as a group seem to have significant more drive
than women as a group, in both sexes, drive requires the presence of a modest
amount of testosterone. Drive is frequently dampened by medications that act
within the central nervous system, substances of abuse, psy-chiatric illness,
systemic physical illness, despair and aging. It is heightened by low doses of
a few often-abused substances such as alcohol or amphetamine, manic mechanisms,
falling in love, joy, and some dopaminergic compounds such as those used to
treat Parkinson’s disease.
Motive
The psychological aspect of desire is referred to as motive and is recognized by willingness
to bring one’s body to the part-ner for sexual behavior either through
initiation or receptivity. Motive often directly stems from the person’s
perception of the context of the nonsexual and sexual relationship. Sexual
desire diagnoses are often made in persons who have adequate drive
manifestations. Most sexual desire problems in physically healthy adults are
simply generated by one partner’s unwill-ingness to engage in sexual behavior.
This is often a secret, however. Sexual motives are originally programmed by
social and cultural experiences. Children and adolescents acquire values, beliefs,
expectations and rules for sexual expression. Young people have to find a way
to negotiate their way through the fact that their early motives to behave
sexually frequently coexist with their motives not to engage in sexual behavior. Conflicted motives often persist
throughout life but the reasons for the conflict evolve. A teenager possessed
of considerable drive and motive to make love may inhibit all sexual
activi-ties because of moral considerations emanating from religious education
or the sense that he or she is just not developmentally ready yet.
Wish
An 80-year-old man who had no drive manifestations and had avoided all
sexual contact with his wife for a decade because he could not get an erection,
passionately answered a doctor’s query about his sexual desire, “Of course, I
have sexual desire! I am a red-blooded American male! Why do you think I am
here?” In fact, he was only speaking about his wish to be sexually capable now
that an effective treatment for erectile problems existed. The doctor asked an
imprecise question. The doctor should have sepa-rately explored his drive
manifestations, his sexual motivation to exchange sexual pleasure with his wife
in recent years and his wish for sexual rejuvenation.
The appearance and disappearance of sexual desire is of-ten enigmatic to
a patient, but its ebb and flow result from the ever-changing intensities of
its components, biological drive,
psychological motive and socially
acquired concepts, wish (Table 57.3)
(Levine, 2002). In women, this interplay is generally more difficult to
delineate because drive and motive are some-times inseparable.
Sexual Desire Diagnoses
Two official diagnoses are given to men and women whose desires for partner sexual behavior are deficient: hypoactive sex-ual desire disorder (HSDD) and sexual aversion disorder (SAD). The differences between the two revolve around the emotional intensity with which the patient avoids sexual behavior. When visceral anxiety, fear, or disgust is routinely felt as sexual behav-ior becomes a possibility, sexual aversion is diagnosed. HSDD is far more frequently encountered. It is present in at least twice as many women than men; female to male ratio for aversion is far higher. Like all sexual dysfunctions, the desire diagnoses may be lifelong or may have been acquired after a period of ordinary fluctuations of sexual desire. Acquired disorders may be partner specific (“situational”) or may occur with all subsequent partners (“generalized”).
When the psychiatrist concludes that the patient’s acquired generalized
HSDD is either due to a medical condition, a medica-tion, or a substance of
abuse, the diagnosis is further elaborated to sexual dysfunction due to general
medical condition (for in-stance, HSDD due to multiple sclerosis). The
frequency of the specific etiologies are heavily dependent on the clinical
setting. In oncology settings, medical causes occur in high frequency; in drug
rehabilitation programs, methadone maintenance will be a common cause. In
marital therapy clinics, anger and loss of respect for the partner, hidden
incompatibility of sexual identity between the self and the partner because of
covert homosexuality or paraphilia, an affair, or childhood sexual abuse will
commonly be the basis. In general psychiatry settings, medication side ef-fects
will often be the top layer of several causes. When a major depression disorder
is diagnosed, for instance, the desire disorder is often assumed to be a
symptom of the depression. This usually is incorrect. The desire disorder often
preceded the decompensa-tion into depression.
From a Desire Diagnosis to Dynamics
Those with lifelong
deficiencies of sexual desire are often per-ceived to be struggling with
either: 1) sexual identity issues in-volving gender identity, orientation, or a
paraphilia; 2) having failed to grow comfortable as a sexual person due to
extremely conservative cultural backgrounds, developmental misfortunes, or
abuses. Occasionally the etiology is enigmatic, raising the im-portant question
whether it is possible to never have any sexual drive manifestations on a
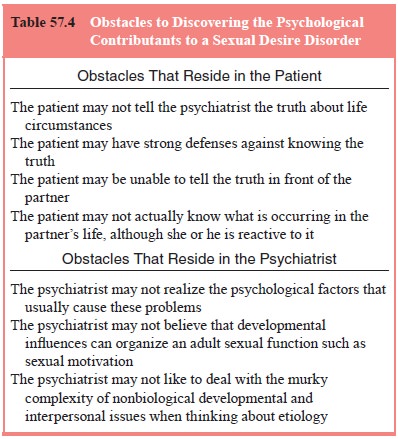
biological basis. (Theoretically, the answer is yes.) Both acquired and
lifelong desire disorders are often associated with past or chronic mood
disorders. Disorders of desire are often listed as “of unknown etiology”, but
clinicians should be skeptical of this idea because:
·
The patient may not tell the doctor
the truth early in the relationship;
·
The patient may have strong
defenses against knowing the truth;
·
The patient may not be able to
speak freely in front of the partner;
·
The patient may not know what is
occurring in the partner’s life, despite being influenced negatively by it;
·
The doctor may not realize the
usual causes of the problem;
·
The doctor may not believe in
developmental influences on the organization of adult sexual function.
Sexual aversion should strongly suggest three possibilities to the
clinician:
·
that a remote traumatic
experience is being relived by the partner’s expression of interest in sexual
behavior;
·
that without the symptom the
patient feels powerless to say “no” to sexual advances;
·
the patient feels guilty about
her own sexual behavior with another person.
The doctor’s attention should focus on the patient’s sexual devel-opment
as a child, adolescent and young adult when the aversion is lifelong, whereas
when it is acquired, the focus of
the his-tory should be on the period immediately prior to the onset of the
symptom.
Desire disorders require the clinician to think both in terms of
development and personal meanings of sex to their indi-vidual patients (Table
57.4). Because all explanations are specu-lative, they should at least make
compelling sense of the patients’ life experiences. Some explanations are based
on the influence
of remote developmental processes. The term madonna–whore complex misleads
us into thinking this is only a male pattern. The syndrome is manifested by normal sexual capacity with anyone
but the fiancé or spouse. Freud interpreted this as a sign of incomplete
resolution of the oedipal complex. The man was thought to be unable sexually to
desire his beloved because he had unconsciously made her into his mother. He
withdrew his sexual interest from her to protect himself from symbolic incest.
Some women are comparably unable sexually to enjoy their part-ners because they
unconsciously confuse their beloved with their father. Another form can be seen
among patients whose parents were grossly inadequate caregivers. When these men
and women find a reliable, kind, supportive person to marry, they quickly
discover a strong motive to avoid sexual behavior with their fiancé. The
patient makes the partner into a good-enough parent, experiences anxiety as an
unconscious threat of incest associ-ated with the possibility of sex, and
becomes skillful at avoiding sexual opportunities.
Most sexual desire disorders are difficult to overcome quickly. Brief
treatment generally should not be undertaken. Serious individual or couple
issues frequently underlie these diagnoses. They have to be afforded time to
emerge and to be worked through. However, clinicians need not be pessimistic
about all of these conditions. For example, helping a couple re-solve a marital
dispute may return them to their usual normal sexual desire manifestations. For
many individuals and couples, therapy assists the couple to accept more calmly
the profound implications of continuing marital discord, infidelity,
homosexu-ality, or other contributing factors. Some treatment failures lead to
divorce and the creation of a relationship with a new partner. There is then no
further sign of the desire problem. Problems rooted in early developmental
experiences are particularly diffi-cult to overcome. While DSM-IV asks the
clinician to make many distinctions among the desire disorders, no follow-up
study has been published in which either the subtypes (lifelong, acquired,
situational, generalized) or etiologic organizers (relationship de-terioration
with and without extramarital affairs, sexual identity incompatibilities,
parental, and medical) are separated into good and poor prognosis categories.
Developmental and identity matters are typically approached in long-term
individual psychotherapy. In these ses-sions women often discuss the
development of their femininity from adolescence to young womanhood, focusing
on issues of body image, beauty, social worth to others, moral sensibilities, social
awkwardness and whether they consider themselves de-serving of personal
physical pleasure. Men often discuss similar issues in terms of masculinity.
Anger, loss of respect, marital discord and extramarital af-fairs may be
approached in either individual or conjoint formats. In either setting,
patients often formulate the etiology as having fallen out of love with the
partner. Those whose cultural back-grounds limit their ease in being a sexual
person are often en-couraged in educational and cultural experiences that might
help them outgrow their earliest notions about what is proper sexual behavior.
The Problems of Sexual Arousal
The emotion interchangeably referred to as sexual arousal or sexual
excitement generates changes in respiration, pulse and muscular tension as well
as an increased blood flow to the geni-tals. Genital vasocongestion creates
vaginal lubrication, clitoral tumescence, labial color changes, and penile
erection, testicu lar elevation and penile color changes. How arousal is centrally
coordinated in either sex remains mysterious. During lovemak-ing, men and women
do not necessarily maintain or progressively increase their arousal; rather
often there is a fluctuating intensity of arousal which is reflected in
variations in vaginal wetness and penile turgidity and nongenital signs of
arousal.
Female Sexual Arousal Disorder
The specificity and validity of this disorder is unclear. In women it is
far more difficult to separate arousal and desire problems than in men. The
perimenopausal period is now recognized as generating complaints about
decreased drive, motivation, lubri-cation and arousal in at least 35 to 50% of
women. However, it is unclear whether to label the problem as primarily of
desire or arousal. It is assumed to be endocrine in origin even though
estrogen, progesterone and testosterone replacement do not reli-ably reverse
the pattern. Even in younger regularly menstruating women, however, diminished
motivation and dampened drive makes it difficult to sustain arousal. Many have
called into ques-tion the accepted notions that desire necessarily precedes
arousal and that they are separate physiological processes. Female arousal
disorder implies that drive and motivation are relatively intact although
arousal is difficult. The disorder is usually an ac-quired diagnosis. Premenopausal women who have it focus on the lack of moisture in the vagina or
their failure to be excited by the behaviors that previously reliably brought
pleasure. They have drive and motive and wish, but enigmatically are unable to
sustain arousal. Some mental factor arises to distract them from their
excitement during lovemaking. Therapy is focused, therefore, on the meaning of
what preoccupies them. This often involves the dynamics of their current
individual or partnered life or the influence of their past relationships on
their present. With therapy the diagnosis often is changed to a HSDD.
In peri- and postmenopausal women, arousal problems are more often
focused on the body as a whole rather than just genital moisture deficiencies.
Skin insensitivity, often a euphemism for decreased pleasure in response to
oral and manual nipple, breast and vulvar stimulation, is often initially
treated as a symptom of “estrogen” deficiency. Early in the menopause, a small
minority of women have an increase in drive due to changing
testoster-one–estrogen ratios. Yet, they may still subjectively experience
arousal as different than it used to be. Therapy often focuses on the women’s
concerns about estrogen replacement and the con-sequences of menopause in terms
of body image, attractiveness, fears of partner infidelity, loss of health and
vigor, and aging.
Aging of the female arousal mechanisms, whether simply due to shifts in
ovarian endocrine production or systemic aging mechanisms, occurs earlier than
deterioration of orgasmic physi-ology. Women with decreasing arousal are often,
therefore, still reliably orgasmic with the use of vaginal lubricants well into
old age. Women who have been treated with chemotherapy for breast cancer are a
particularly problematic group to offer as-sistance to for their new arousal problems.
Fear of stimulating remaining cancerous cells makes systemic estrogen
replacement contraindicated.
In 1999 a
renewed interest in female arousal disorder, some-times casually called female
sexual dysfunction surfaced in response to the efficacy of Viagra for men’s
arousal problems. It was reasoned that since the penis and clitoris are
embryologic homologues with comparable adult histology, the drug would improve
women’s arousal. Placebo-controlled trials concluded that the drug did not
improve arousal any more than placebo (Basson et al., 2002).
Male Erectile Disorder
The mechanisms of erection – the sequestering and maintaining arterial
blood within the corpora cavernosa – are being elucidated by urological
research. Their research has led to a diminishing emphasis on “psychogenic
impotence” diagnosis. Urologists may refer to male erectile disorders (ED) of a
psychogenic origin as “adrenergic” ED, a reference to the preponderance of
sympa-thetic tone on the corporal mechanisms that maintain flaccidity.
Adrenergic dominance of the penile arterial tone is created by a mind that
perceives the sexual context as a dangerous, frighten-ing, or as unwanted.
The prevalence of ED rises dramatically in the sixth dec-ade of life
from less than 10 to 30%; it increases further during the seventh decade.
Aging, medical conditions such as diabe-tes, prostatic cancer, hypertension and
cardiovascular risk fac-tors predict the most common pattern of ED due to a
medical condition in this age group. While medication-induced, neuro-logical,
endocrine, metabolic, radiation and surgical causes of erectile dysfunction
also exist, in population studies diabetes, hypertension, smoking, lipid
abnormalities, obesity and lack of exercise are correlated with the progressive
deterioration of erec-tile functioning in the sixth and seventh decades. These
factors are thought to create a relative penile anoxemia which stimulates the
conversion of corporal smooth muscle cells into fibrocytes. The gradual loss of
elasticity of the corpora interferes with fill-ing and sequestering of arterial
blood. Erections at first become unreliable and finally impossible to obtain or
sustain.
At every age, selectivity of
erectile failure is the single most important diagnostic feature of primary
erectile dysfunc-tion. Clinicians should inquire about the relative firmness
and duration of erections under each of these circumstances: mas-turbation, sex
other than intercourse, sex with other female or male partners, upon
stimulation with explicit media materials, in the middle of the night and upon
awakening. If under some circumstances the erection is firm and lasting, the
clinician can usually assume that the man’s neural, endocrine and vascular
physiology is sufficiently normal and that the problem is psycho-genic in
origin. This is true even for men in their fifties and older. Clinicians often
feel more certain about this diagnosis when no diseases thought to lead to
erectile dysfunction are present.
Lifelong male ED typically is psychogenic and involves ei-ther a sexual
identity dilemma: such as transvestism, gender iden-tity disorder, a homoerotic
orientation, a paraphilia, or another diagnosis that expresses the patient’s
fear of being sexually close to a partner. Sexual identity problems are often initially
denied unless the clinician is nonjudgmental and thorough during the inquiry.
However, obsessive–compulsive disorder, schizoid per-sonality, a psychotic
disorder, or severe character disorders may be present. Occasionally, a
reasonably normal young man with an unusually persistent fear of sexual
intercourse seeks attention. These good prognosis cases are sometimes
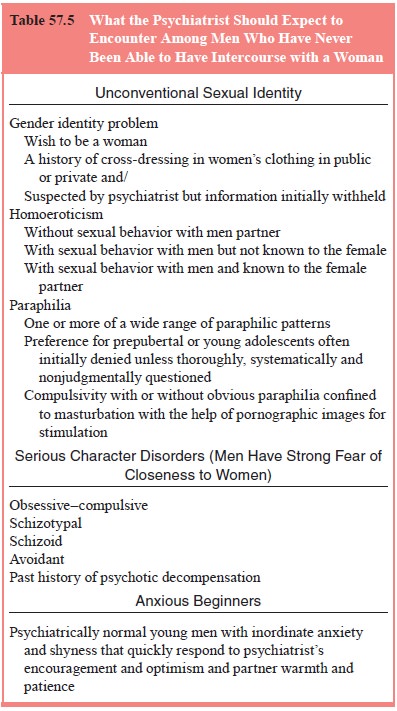
informally referred to as anxious beginners (Table 57.5). With that exception,
men with lifelong male arousal disorder (MAD), when taken into in-dividual
therapy are usually perceived as having a strong motive to avoid sexual
behavior and while dysfunctional with a partner during much of their therapy
might equally be diagnosed as hav-ing HSDD with normal drive but a motive to
avoid partner sex. The prognosis with older men with lifelong erectile
dysfunction is poor even with modern erectogenic agents. Long-term therapy,
even if it does not enable regular intercourse, may enable more emotional and
sexual closeness to a partner. Some reasonably masculine appearing men with
mild gender identity problems
can quickly become potent if they can reveal their need during sexual
relationship to cross-dress (use a fetish article of clothing) to a partner who
calmly accepts his requirement. However, most of these men have inordinate
fears of sexually bonding to any woman and, in therapy, become preoccupied with
basic devel-opmental issues. Some of them marry and form companionate
relationships that are rarely or never consummated.
In dramatic contrast, men with long-established good po-tency who have
recently lost their erectile capacities with their partner – acquired
psychogenic ED – have a far better prognosis (Table 57.6). They may be treated
in individual or couples format, depending on the precipitants of the sexual
problem and the status of their relationship with their partner. Many of these
therapies become focused on resentments that have not been identified,
dis-cussed and worked through by the couple. Such distressed couples are most
efficiently helped in a conjoint format. When extramari-tal affairs are part of
the relationship deterioration and cannot be discussed, most clinicians simply
work with one spouse. Potency is frequently lost following a separation or
divorce. Impaired potency after a spouse’s death is either about unresolved
grief or problems that exist prior to the wife’s terminal illness. Men are also
often worried about their potency when their financial or
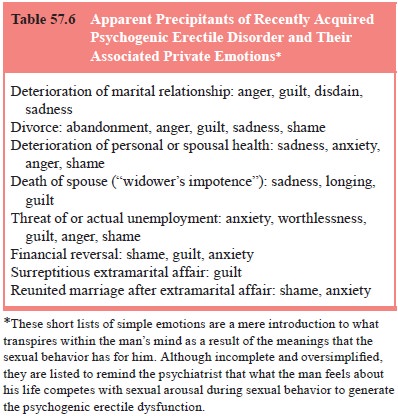
vocational lives crumble, when they have a serious new physical illness
such as a myocardial infarction or stroke, or when their wives become seriously
ill. The esthetics of lovemaking require a context of reasonable physical
health; when one spouse becomes chronically ill or disfigured by illness or
surgery, either one of the couple may lose their willingness to be sexual. This
may be reflected in impaired erections or sexual avoidance.
Regardless of the precipitating factors, men with arousal disorders have
performance anxiety. They anticipate erectile failure before sex begins and
vigilantly monitor their state of tumescence during sex (Masters and Johnson,
1970). Perform-ance anxiety is present in almost all impotent men. Performance
anxiety is efficiently therapeutically addressed by identifying it to the
patient and asking him to make love without trying inter-course on several
occasions to demonstrate to himself how dif-ferent lovemaking can feel for him
when he is not risking failure. This enables many to relax, concentrate on
sensation and return to previous states of sensual abandon during lovemaking.
This technique is known as sensate focus.
The psychological treatment of acquired arousal disorders is often
highly satisfying for the professional because many of the men are anxious for
help. Motivation to behave sexually is often present, fear can be allayed and
men can learn to appreci-ate the emotional complexity of their lives. They can
be shown how their minds prevented intercourse until they could acknowl-edge
what has been transpiring within and around them. Many recently separated men,
for example, are grieving, angry, guilty, uncertain and worried about their
finances. Yet, they may pro-pel themselves into a new relationship. Two
characteristics seem to predispose to erectile problems at key life
transitions: 1) The pursuit of the masculine standard that men ought to be able
to perform intercourse with anyone, anywhere, under any circum-stances; 2) The
inability to readily grasp the nature and signifi-cance of his inner
experiences. “Yes, my schizophrenic daughter became homeless in another city,
my wife was depressed and be-gan drinking to excess in response, and I had a financially
costly affair with my secretary. What do these have to do with my loss of
potency?” (Table 57.7).

Sildenafil revolutionized the treatment of erectile dysfunc-tion in
1998. This phosphodiesterase type 5 inhibitor maintains corporal vasodilatation
by preventing the degradation of cGMP. Sexual arousal leads to the corporal
secretion of nitric oxide which is converted by an enzyme into cGMP. Sildenafil
is in-creasingly effective as the dose is increased from 25 to 50 up to 100 mg.
The drug must not be used when any organic nitrate is being taken because it
dangerously potentiates the hypoten-sive effect of the nitrates risking brain
and myocardial infarction. Sildenafil is dramatically underutilized by
psychiatrists.
Prior to sildenafil, urologists argued that most erectile dys-function
was organic in origin, but since the drug works at about the same rate
regardless of the pretreatment etiology, most erec-tile dysfunction is now
recognized to be of mixed – organic and psychosocial – origin. Three conditions
have unique response profiles: after prostatectomy the response rate is
approximately 34%, among diabetics it is approximately 43%, and among the
spinal cord injured it is approximately 80%; the same rate seems to improve
psychogenic ED. Other medical interventions are also effective in varying
degrees for largely organic erectile dysfunc-tion: vacuum pump, the
intracavernosal injection of vasodilating substances, intraurethral aprostadil,
the surgical implantation of a penile prostheses and, outside the USA,
sublingual apomor-phine. Because sildenafil’s rate of improving erections is
sig-nificantly higher than the restoration of a mutually satisfactory sexual
equilibrium (approximately 44%), psychological ED that persists after medication
should be treated by a mental health professional.
Related Topics