Chapter: Essentials of Psychiatry: Sexual Disorders
Sexual Disorders: Gender Identity Disorders
Gender Identity Disorders
The
organization of a stable gender identity is the first component of sexual
identity to emerge during childhood. The processes that enable this
accomplishment are so subtle that when a daughter consistently acts as though
she realizes that “I am a girl and that is all right”, or when a son’s behavior
announces that “I am a boy and that is all right”, families rarely even
remember their chil-dren’s confusion and behaviors to the contrary. Adolescent
and adult gender problems are not rare. They are however commonly hidden from
social view, sometimes long enough to developmen-tally evolve into other less
dramatic forms of sexual identity
Early Forms
Extremely Feminine Young Boys
Although occasionally the parents of a feminine son have a con-vincing
anecdote about persistent feminine interests dating from early in the second
year of life, boyhood femininity is more typi-cally only apparent by the third
year. By the fourth year playmate preferences become obvious. Same-sex playmate
preference is a typical characteristic of young children.
Cross-gender–identified children consistently demonstrate the opposite sex
playmate pref-erence. The avoidance of other boys has serious consequences in
terms of social rejection and loneliness throughout the school years. The peer
problems of feminine boys cause some of their behavioral and emotional problems
which are in evidence by mid-dle-to-late childhood. However, psychometric
studies support clinical impressions that feminine boys have emotional problems
even before peer relationships become a factor, that is, something more basic
about being cross-gender-identified creates problems. Young feminine boys have
been shown to be depressed and have difficulties with separation anxiety.
Speculations about the origin of boyhood femininity generally suggest
converging cumulative forces. Any child’s cross-gender identifications are
likely to involve a host of fac-tors: constitutional forces, problematic
interactions with parents, problematic internal processing of life experiences
and family misfortune: financial, reproductive, physical disease, emotional
illness, or death of vital persons. These factors are sometimes restated as
temperament, disturbed family functioning, separa-tion–individuation problems
and trauma.
Temperament is a dual phenomenon being both the child’s predisposition
to respond to the world in a certain way and the as-pects of the child to which
others respond. The common tempera-mental factors of feminine boys have been
described as: a sense of body fragility and vulnerability that leads to the
avoidance of rough-and-tumble play; timidity and fearfulness in the face of new
situations; a vulnerability to separation and loss; an unusual capacity for
positive emotional connection to others; an ability to imitate; sensitivities
to sound, color, texture, odor, temperature and pain (Coates et al., 1992).
The development of boyhood femininity may occur within the mind of the
toddler in response to a loss of emotional avail-ability of the nurturant
mother. The child creates a maternal (feminine) self through imitation and
fantasy in order to make up for the mother’s emotional unavailability. This
occurs beyond the family’s awareness and is left in place by the family either
ignoring what has transpired in the son or valuing it. The problem for the
effeminate boy is that reality – the social expectations of other people – is
unyielding on gender issues; the adaptive early life solution becomes
progressively more maladaptive with time.
The answer to the question whether boyhood femininity is entirely
constitutional, an adaptive solution, or due to a combina-tion that includes
some other process is not known. A few reports of femininity giving way to
psychotherapeutic interventions with young boys and their families are of
heuristic value but limited in follow-up duration.
Green prospectively studied a large well-matched group of feminine boys
for over a decade and discovered that boyhood ef-feminacy was a frequent
precursor of adolescent homoeroticism and homosexual behavior rather than
gender identity disorders. He observed, as had others before, that without
therapy feminine gender role behaviors give rise to more masculine behavioral
styles as adolescence emerges (Green, 1987).
Masculine Girls: Tomboys
The masculinity of girls may become apparent as early as age 2 years.
The number of girls brought to clinical attention for cross-gendered behaviors,
self-statements and aspirations is con-sistently less than boys by a factor of
1: 5 at any age of childhood in Western countries (except Poland). It is not
known whether this reflects a genuine difference in incidence of childhood
gen-der disorders, cultural perceptions of femininity as a negative in boys
versus the neutral-to-positive perception of boy-like behav-iors in girls, the
broader range of cross-gender expression per-mitted to girls but not to boys,
or an intuitive understanding that cross-gender identity more accurately
predicts homosexuality in boys than girls.
The distinction between tomboys and gender-disordered girls is often
difficult to make. Tomboys are thought of as not as deeply unhappy about their
femaleness, not as impossible occa-sionally to dress in stereotypic female
clothing, and not thought to have a profound aversion to their girlish and
future womanly physiologic transformations. Tomboys are able to enjoy some
fem-inine activities along with their obvious pleasures in masculine-identified
toys and games and the company of boys. Girls who are diagnosed as gender-disordered
generally seem to have a relentless intensity about their masculine
preoccupations and an insistence about their future. The onset of their
cross-gendered identifications is early in life. Although most lesbians have a
history of tomboyish behaviors, most tomboys develop a heterosexual
orientation.
The Subjectivity of a Well-developed Gender Disorder
Children, teenagers and adults exist who rue the day they were born to
their biological sex and who long for the opportunity sim-ply to live their
lives in a manner befitting the other gender. They repudiate the possibility of
finding happiness within the broad framework of roles given to members of their
sex by their society. Their repudiation is not motivated by an intellectual
attack on sexism, homophobia, or any other injustice imbedded in cultural
mores. A gender-disordered person literally repudiates his or her body,
repudiates the self in that body and rejects performing roles expected of
people with that body. It is a subtle, usually self-contained rebellion against
the need of others to designate them in terms of their biological sex.
The repudiation and rebellion may first occur as a subjec-tive internal
drama of fantasy, as behavioral expression in play, or a preference for the company
of others. Regardless of when and how it is displayed, the drama of the
gender-disordered involves the relentless feeling that “life would be better –
easier, fuller, more enjoyable – if I and others could experience me as a
mem-ber of the opposite sex”.
By mid-adolescence, the extremely gender-disordered have often
envisioned the solution for their paralyzing self-consciousness: to live as a
member of the opposite gender, to transform their bodies to the extent possible
by modern medicine, and to be accepted by all others as the opposite sex. Most
people with these cross-gender preoccupations, however, do not go be-yond the
fantasy or private cross-dressing. Those that do eventu-ally come to
psychiatric attention. When a clinician is called in, the family has one set of
hopes, the patient another. The clinician has many tasks, one of which is to
mediate between the ambitions of the gender-disordered person and society and
see what can be done to help the patient. Negative countertransference may steer
the clinician to deal with the opportunity expeditiously: “Obvi-ously the
patient is sick, maybe psychotic, and needs help. I don’t take care of people
who do these things. Refer it out!” With a lit-tle supervisory encouragement to
perform a thorough evaluation, therapists soon find that these patients possess
many of the ordi-nary aspects of life and one unusual ambition: they often want
to be the opposite sex so badly that they are willing to make it a priority
over family, friends, vocation and material acquisition.
Diagnostic Criteria of Gender Identity Disorder
Adults who permanently change their bodies to deal with their gender
dilemmas represent the far end of the spectrum of adapta-tions to gender
problems. Even the lives of those who reject bod-ily change, however, have
considerable pain because the images of a better gendered self may recur
throughout life, becoming more powerful whenever life becomes strained or
disappointing.
The diagnosis of the extreme end of the gender identity dis-order spectrum
is clinically obvious. The challenging diagnostic task for clinicians is to
suspect a gender problem and inquire about gender identity and its evolution in
those whose manner suggest unisexed or cross-gendered appearance, those with
dissociative gender identity disorder (GID), severe forms of character
pathol-ogy and those who seem unusual in some undefinable manner.
DSM-IV provides the clinician with two Axis I gender diagnoses. To
qualify for the first, a patient of any age must meet four criteria:
Criterion 1: Strong, persistent
cross-gender identifica-tion Because
young children may not verbalize enough about their inner experiences for the clinician to be certain that this
criterion is met, at least four of five manifestations of cross-gen-der
identification must be present: 1) repeatedly stated desire to be, or
insistence that he or she is, the opposite sex; 2) in boys, preference for
cross-dressing or simulating female attire; in girls, insistence on wearing
stereotypical masculine clothing; 3) strong and persistent preferences for
cross-gender roles in fantasy play or persistent fantasies of being the
opposite sex; 4) intense de-sire to participate in the games and pastimes of
the opposite sex; 5) strong preference for playmates of the opposite sex.
In adolescence and adulthood, this criterion is fulfilled when the
patient states the desire to be the opposite sex, has fre-quent social forays
into appearing as the opposite sex, desires to live or be treated as the
opposite sex, or has the conviction that his or her feelings and reactions are
those typical of the opposite sex.
Criterion 2: Persistent
discomfort with one’s gender or the sense of inappropriateness in a gender role
This criterion is fulfilled in boys who assert that their penis or testicles are
dis-gusting or will disappear or that it would be better not to have these
organs; or who demonstrate an aversion toward rough-and-tumble play and
rejection of male stereotypical toys, games and activities. In girls, rejection
of urinating in a sitting position or assertion that they do not want to grow
breasts or menstruate, or marked aversion towards normative feminine clothing
fulfill this criterion.
Among adolescents and adults, this criterion is fulfilled by the
patients’ exhibiting the following characteristics: preoc-cupation with getting
rid of primary and secondary sex charac-teristics; preoccupation with thoughts
about hormones, surgery, or other alterations of the body to enhance the
capacity to pass as a member of the opposite sex such as electrolysis for beard
removal, cricoid cartilage shave to minimize the Adam’s apple, breast
augmentation, or preoccupation with the belief that one was born into the wrong
sex.
Criterion 3: Not due to an
intersex condition In the vast ma-jority of clinical
circumstances the patient possesses normal gen-ital anatomy and sexual
physiology. When a patient with a gender identity disorder and an accompanying
intersex condition such as congenital adrenal hyperplasia, an anomaly of the
genitalia, or a chromosomal abnormality is encountered, the clinician will be
uncertain whether the intersex condition is the cause of the GID. The clinician
may either diagnose gender identity disorder not otherwise specified (GIDNOS)
or classify the patient as hav-ing a GID and list the physical factor on Axis
III as a comorbid condition. The relationship between GID and intersex
conditions is controversial topic that may be clarified with further research
being done in Germany.
Criterion 4: Significant distress
and impairment It is likely that many children, adolescents and adults struggle for a while to
consolidate their gender identity but eventually find an adap-tation that does
not impair their capacities to function socially, academically, or vocationally
as a member of their sex. These persons do not qualify for GID nor do those who
simply are not stereotypic in how they portray their gender roles. Mental
health professionals occasionally encounter parents who are disturbed by their
adolescent child’s gender roles. Parental distress is not the point of
criterion 4; this criterion refers to patient distress.
Diagnostic Criteria of Gender Identity Disorder Not Otherwise Specified (GIDNOS)
If an accurate community-based study of the gender-impaired could be conducted,
most cases would be diagnosed as GIDNOS. The diagnostician needs to understand
that gender identity de-velopment is a dynamic evolutionary process and
clinicians see people at crisis points in their lives. At any given time,
although it is clear that the patient has some form of GID, it may not be that
which is described in DSM-IV as GID. Here is one example: an adult female calls
herself a “neuter”. She wants her breasts re-moved because she hates to be
perceived as a woman. For 2 years she has been exploring “neuterdom” and “I am
definitely not in-terested in being a man!” If in 2 years, she evolves to meet
crite-rion 1, her current GIDNOS diagnosis will change.
GIDNOS is a large category designed to be inclusive of those with
unusual genders who do not clearly fit the criteria of GID. There is no
implication that if a patient is labeled GIDNOS that his or her label cannot
change in the future. GIDNOS would contain the many forms of transvestism:
masculine-appearing boys and teenagers with persistent cross-dressing (former
fet-ishistic transvestites) who are evolving toward GID, socially iso-lated men
who want to become a woman shortly after their wives or mothers die (secondary
transvestites) but express considerable ambivalence about the very matter they
passionately desired at their last visit, extremely feminized homosexuals
including those with careers as “drag queens” who seem to want to change their
sex when depressed, and so on. GIDNOS would also capture men who want to be rid
of their genitals without being feminized, uni-sexual females who imagine
themselves as males but who are terrified of any social expression of their
masculine gender iden-tity, hypermasculine lesbians in periodic turmoil over
their gen-der, and those women who strongly identify with both male and female
who lately want mastectomies. In using gender identity diagnoses, clinicians
need to remember that extremely masculine women or extremely feminine men are
not to be dismissed as ho-mosexual. “Lesbian” or “gay” is only a description of
orientation. They are more aptly described as also cross-gendered.
The Relationship of Gender Identity Disorders to Orientation
The usual clarity of distinctions between heterosexual, bisexual and
homosexual orientations rests upon the assumption that the biological sex and
psychological gender of the person and the partner are known. A woman who
designates herself as a les-bian is understood to mean she is erotically
attracted to other women. “Lesbian” loses its meaning if the woman says she
feels she is a man and lives as one.
She insists, “I am a heterosexual man; men are attracted to women as am I!” The
baffled clini-cian may erroneously think, “You are a female therefore you are a
lesbian!” DSM-IV suggests that adults with GIDs should be subgrouped according
to which sex the patient is currently sexu-ally attracted: males, females,
both, or neither. This makes sense for most gender patients because it is their
gender identity that is most important to them. Some are rigid about the sex of
those to whom they are attracted because it supports their idea about their
gender, others are bierotic and are not too concerned with their orientation,
still others have not had enough experiences to overcome their uncertainty
about their orientation. A few gender patients find all partners too
complicated and are only interested in themselves.
Treatment Options for the Gender Identity Disorders
The treatment of these conditions, although not as well-based on
scientific evidence as some psychiatric disorders, has been carefully
scrutinized by multidisciplinary committees of special-ists within the Harry
Benjamin International Gender Dysphoria Association for over 20 years. For more
details in managing an individual patient, please consult its “Standards of
Care” (Meyer et al., 2001). The
treatment of any GID begins after a careful
evaluation, including parents, other family members, spouses, psychometric
testing, and occasionally physical and laboratory examination. The details will
depend on age of the patient. It is possible, of course, to have a GID as well
as mental retardation, a psychosis, dysthymia, severe character pathology, or
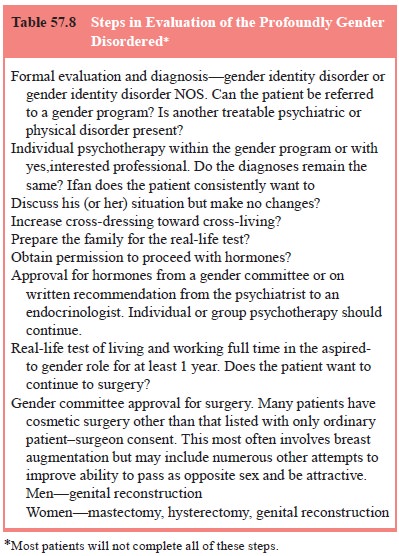
any other psychiatric diagnosis (Table 57.8).
Individual Psychotherapy
No one knows how to cure an adult’s gender problem. People who have lived long with profound cross-gender identifications do not get insight – either behaviorally modified or medicated – and find that they subsequently have a conventional gender identity. Psy-chotherapy is useful, nonetheless. If the patient is able to trust a therapist, there can be much to talk about: family relationships are often painful, barriers to relationship intimacy are profound, work poses many difficult issues, and the patient has to make monumental decisions. The central one is, “How am I going to live my life? Should I go through with cross-gender living, hor-mone therapy, mastectomy, or genital surgery?” The therapist can help the patient recognize the drawbacks and advantages of the various available options and to respect the initially unrecog-nized or unstated ambivalence. Completion of the gender trans-formation process usually takes longer than the patient desires, and the therapist can be an important source of support during and after these changes.
Group Therapy
Group therapy for gender-disordered people has the advantages of
allowing patients to know others with gender problems, of de-creasing their
social isolation, and of being among people who do not experience their
cross-gender aspirations and their past be-haviors as weird. Group members can
provide help with groom-ing and more convincing public appearances. The success
of these groups depends on the therapist’s skills in patient selection and
using the group process. Groups are generally only available in a few
specialized treatment programs.
“Real-life Test”
Living in the aspired-to-gender role – working, relating, conduct-ing
the activities of daily living – is a vital process that enables one of three
decisions: to abandon the quest, to simply live in this new role, or to proceed
with breast or genital surgery (Peterson and Dickey, 1995). Some clinicians use
the real-life test as a cri-terion for recommending hormones but this varies
because some patients’ abilities to present themselves in a new way is
definitely enhanced by prior administration of cross-sex hormones. The reason
for the real-life test is to give the patient, who created a transsexual
solution in fantasy, an opportunity to experience the solution in social
reality. Passing the real-life test is expected to be associated with improved
psychological function.
Hormone Therapy
Ideally, hormones should be administered by endocrinologists who have a
working relationship with a mental health team dealing with gender problems.
The effects of administration of estrogen to a biological male are: breast
development, testicular atrophy, decreased sexual drive, decreased semen volume
and fertility, softening of skin, fat redistribution in a female pattern and
decrease in spontaneous erections. Breast development is often the highest
concern to the patient. Because hair growth is not affected by estrogens,
electrolysis is often used to remove beard growth. Side effects within
recommended doses are minimal but hypertension, hyperglycemia, lipid
abnormalities, thrombophlebitis and hepatic dysfunction have been described.
The most dramatic effect of hormones is on the sense of well-being. Patients
report feeling calmer, happier knowing that their bodies are being
demasculinized and feminized. All results derive from open-labeled studies.
The administration of androgen to females results in an increased sexual
drive, clitoral tingling and growth, weight gain, and amenorrhea and
hoarseness. An increase in muscle mass may be apparent if weight training is
undertaken simultaneously. Hairgrowth depends on the patient’s genetic
potential. Androgens are administrated intramuscularly 200 to 300 mg/month and
are generally safe. It is prudent, however, periodically to monitor he-patic,
lipid and thyroid functioning. Most patients are delighted with their bodily
changes, although some are disappointed that they remain short, wide-hipped,
relatively hairless men with breasts that do not significantly regress.
Surgical Therapy
Surgical intervention is the final external step. It should not occur
without mental health professional’s input, even when the patient provides a
heart-felt convincing set of reasons to bypass the real-life test, hormones and
therapeutic relationship. Genital surgery is expensive, time-consuming, at
times painful, and has frequent anatomic complications and functional
disappointments. Sur-gery can be expected to add further improvements in the
lives of patients: more social activities with friends and family, more
activity in sports, more partner sexual activity and improved vo-cational
status.
Males Surgery consists of penectomy, orchiectomy, vagino-plasty and fashioning
of a labia. The procedures used for the creation of a neovagina have evolved
over the years. Postopera-tively, the patient must maintain the patency of the
neovagina by initially constantly wearing and then periodically using a vaginal
dilator. Vaginal stenosis or shortening is a frequent complication. The quest
for an unmistakable feminine shape leads many young adult patients to
augmentation mammoplasty and the shaving of their cricoid cartilage.
Females The creation of a male-appearing chest through mas-tectomies and
contouring of the chest wall requires only a brief hospital stay. Patients are
usually immediately delighted with their new-found freedom, but their fantasies
of going shirtless are often not fulfilled due to the presence of two
noticeable hori-zontal chest scars. The creation of a neophallus that can
become erect, contain a functional urethra throughout its length (enabling
urination while standing), and pass as an unremarkable penis in a locker room
has been a significant surgical challenge. It is far from perfected. The
surgery is, however, the most time-consum-ing, technically difficult and
expensive of all the sex reassign-ment procedures. Erection is made possible by
a penile prosthe-sis. Many prudent patients consider themselves reassigned when
they have a hysterectomy, oophorectomy and mastectomy. Some just have a
mastectomy. They find a partner who understands the situation and supports the
idea of living with, and loving with, female genitals.
Related Topics