Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Ophthalmic Surgery
Regional Anesthesia for Ophthalmic Surgery
Regional Anesthesia for Ophthalmic Surgery
Options for local anesthesia for eye surgery include topical application of local anesthetic or placement of a retrobulbar block or the more commonly utilized peribulbar or sub-Tenon’s (episcleral) block. All of these techniques are most com-monly combined with intravenous sedation. Local anesthesia is preferred to general anesthesia for eye surgery because local anesthesia involves less physiologic trespass and is less likely to be associ-ated with PONV. However, eye block procedures have potential complications and may not provide adequate akinesia or analgesia of the eye. Some patients may be unable to lie perfectly still for the duration of the surgery. For these reasons, appro-priate equipment and qualified personnel required to treat the complications of local anesthesia and to induce general anesthesia must be readily available.
RETROBULBAR BLOCKADE
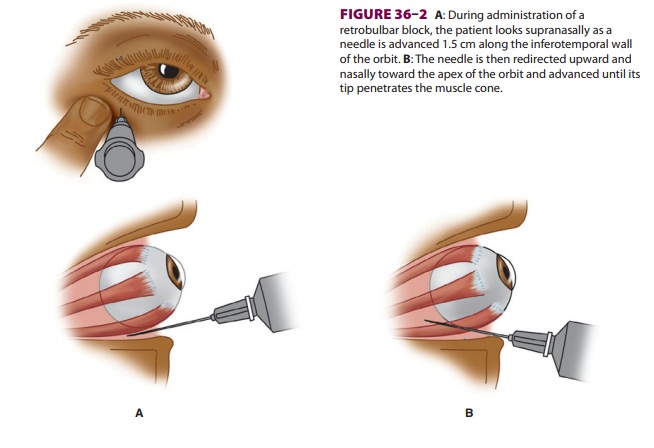
In this technique, local anesthetic is injected behind the eye into the
cone formed by the extra-ocular muscles ( Figure 36–2), and a facial nerve block is
utilized to prevent blinking ( Figure 36–3).
blunt-tipped 25-gauge needle
penetrates the lower lid at the junction of the middle and lateral
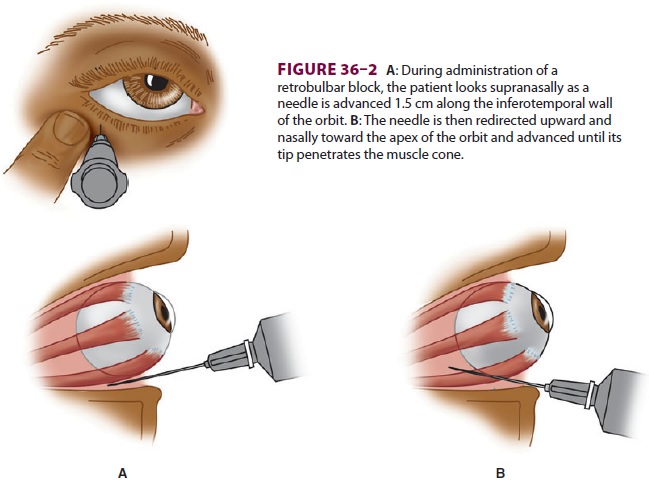
one-third of the orbit (usually 0.5 cm medial
to the lateral canthus). Awake patients are instructed to stare supranasally as
the needle is advanced 3.5 cm toward the apex of the muscle cone. Commonly,
patients undergoing such eye blocks will receive a brief period of deep
sedation during the block (using such agents as etomidate, propofol, and
remifentanil). After aspiration to preclude intra-vascular injection, 2–5 mL of
local anesthetic is injected, and the needle is removed. Choice of local
anesthetic varies, but lidocaine 2% or bupivacaine 0.75% are most common.
Ropivacaine may be used instead of bupivacaine. Addition of epineph-rine
(1:200,000 or 1:400,000) may reduce bleed-ing and prolong the anesthesia.
Hyaluronidase (3–7 U/mL), a hydrolyzer of connective tissue polysaccharides, is
frequently added to enhance the retrobulbar spread of the local anesthetic. A
successful retrobulbar block is accompanied by anesthesia, akinesia, and
abolishment of the oculocephalic reflex (ie, a blocked eye does not move during
head turning).
Complications of retrobulbar injection of
local anesthetics include retrobulbar hemorrhage, perfo-ration of the globe,
optic nerve atrophy, intravascu-lar injection with resultant convulsions,
oculocardiac reflex, trigeminal nerve block, respiratory arrest, and, rarely,
acute neurogenic pulmonary edema. Forceful injection of local anesthetic into
the oph thalmic artery causes retrograde flow toward the brain and may result
in an instantaneous seizure. The postretrobulbar block apnea syndrome is
probably due to injection of local anesthetic into the optic nerve sheath, with
spread into the cerebrospinal fluid. The central nervous system is exposed to
high concentrations of local anesthetic, leading to mental status changes that
may include unconsciousness. Apnea occurs within 20 min and resolves within an
hour. Treatment is support-ive, with positive-pressure ventilation to prevent
hypoxia, bradycardia, and cardiac arrest. Adequacy of ventilation must be
constantly monitored in patients who have received retrobulbar anesthesia.
Retrobulbar injection is usually not performed in patients with bleeding
disorders because of the risk of retrobulbar hemorrhage, extreme myo-pia
because the elongated globe increases the risk of perforation, or an open eye
injury because the pressure from injecting fluid behind the eye may cause
extrusion of intraocular contents through the wound.
PERIBULBAR BLOCKADE
In contrast to retrobulbar blockade, in the
peribul-bar blockade technique, the needle does not pen-etrate the cone formed
by the extraocular muscles. Advantages of the peribulbar technique include less
risk of penetration of the globe, optic nerve, and artery, and less pain on
injection. Disadvantages include a slower onset and an increased likelihood of
ecchymosis. Both techniques will have equal suc-cess at producing akinesia of
the eye.
The peribulbar block is
performed with the patient supine and looking directly ahead (or pos-sibly
under a brief period of deep sedation). After topical anesthesia of the
conjunctiva, one or two
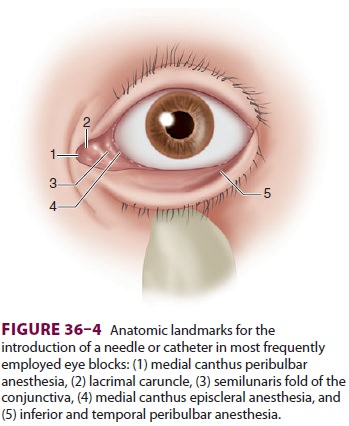
transconjunctival injections are given ( Figure
36–4). As the eyelid is retracted, an
inferotemporal injec-tion is given halfway between the lateral canthus and the
lateral limbus. The needle is advanced under the globe, parallel to the orbital
floor; when it passes the equator of the eye, it is directed slightly medial
(20°) and cephalad (10°), and 5 mL of local
anes-thetic is injected. To ensure akinesia, a second 5-mL injection may be
given through the conjunctiva on the nasal side, medial to the caruncle, and
directed straight back parallel to the medial orbital wall, pointing slightly
cephalad (20°).
Sub-Tenon’s (Episcleral) Block
Tenon’s fascia surrounds the globe and
extraocular muscles. Local anesthetic injected beneath it into the episcleral
space spreads circularly around the sclera and to the extraocular muscle sheaths
(Figure 36–4). A special blunt 25-mm or 19-gauge curved cannula is used for a
sub-Tenon block. After topical anesthe-sia, the conjunctiva is lifted along
with Tenon’s fascia in the inferonasal quadrant with forceps. A small nick is
then made with blunt-tipped scissors, which are then slid underneath to create
a path in Tenon’s fascia that follows the contour of the globe and extends past
the equator. While the eye is still fixed with forceps, the cannula is
inserted, and 3–4 mL of local anesthetic are injected. Complications with the
sub-Tenon blocks are significantly less than with ret-robulbar and peribulbar
techniques. Globe perfora-tion, hemorrhage, cellulitis, permanent visual loss, and local
anesthetic spread into cerebrospinal fluid have been reported.
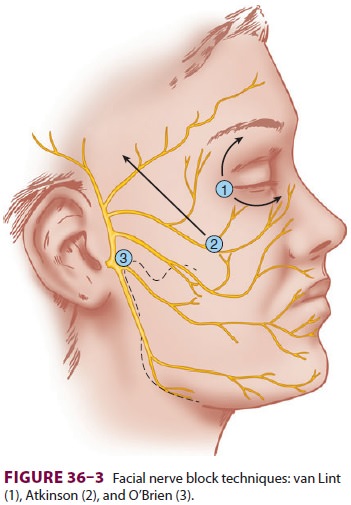
FACIAL NERVE BLOCK
A facial nerve block prevents squinting of the eye-lids during surgery
and allows placement of a lid speculum. There are several techniques of facial
nerve block: van Lint, Atkinson, and O’Brien (Figure 36–3). The major complication
of these blocks is subcutaneous hemorrhage. Another proce-dure, Nadbath’s
technique, blocks the facial nerve as it exits the stylomastoid foramen under
the external auditory canal, in close proximity to the vagus and
glossopharyngeal nerves. This block is not recom-mended because it has been
associated with vocal cord paralysis, laryngospasm, dysphagia, and respi-ratory
distress.
TOPICAL ANESTHESIA OF THE EYE
Simple topical local anesthetic
techniques have evolved for anterior chamber (eg, cataract) and glaucoma
operations, and, increasingly, the trend has been to eliminate local anesthetic
injections entirely. A typical regimen for topical local anes-thesia consists
of application of 0.5% proparacaine (also known as proxymetacaine chlorhydrate)
local anesthetic drops, repeated at 5-min intervals for five applications,
followed by topical application of a local anesthetic gel (lidocaine
chlorhydrate plus 2% methyl-cellulose) with a cotton swab to the infe-rior and
superior conjunctival sacs. Ophthalmic 0.5% tetracaine may also be utilized.
Topical anes-thesia is not appropriate for posterior chamber sur-gery (eg,
retinal detachment repair with a buckle), and it works best for faster surgeons
with a gentle surgical technique that does not require akinesia of the eye.
INTRAVENOUS SEDATION
Many techniques of intravenous sedation are
avail-able for eye surgery, and the particular drug used is less important than
the dose. Deep sedation, although sometimes used during placement of
oph-thalmic nerve blocks, is almost never used intraoper-atively because of the
risks of apnea, aspiration, and unintentional patient movement during surgery.
An intraoperative light sedation regimen that includes midazolam (1–2 mg), with
or without fentanyl (25– 50 mcg) or sufentanil (2.5–5 mcg), is recommended.
Doses vary considerably among patients, but should be administered in small
increments. Concomitant use of more than one type of drug (benzodiazepine,
hypnotic, and opioid) potentiates the effects of other agents, and doses must
be reduced accordingly.
Administration of eye blocks can be quite
uncomfortable, and many anesthesia providers will administer small incremental
doses of etomidate or propofol to produce a brief state of unconscious-ness
during the regional block. Some will substitute a bolus of opioid (remifentanil
0.1–0.5 mcg/kg or alfentanil 375–500 mcg) to produce a brief period of intense
analgesia during the eye block procedure. Administration of an antiemetic
should be considered if an opioid is used. Regardless of the technique
employed, ventilation and oxygenation must be monitored, and equipment to
provide positive-pressure ventilation must be immediately available.
Related Topics