Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Ophthalmic Surgery
General Anesthesia for Ophthalmic Surgery
General Anesthesia for Ophthalmic Surgery
The choice between general and local
anesthesia should be made jointly by the patient, anesthesiolo-gist, and
surgeon. Patients may refuse to considerlocal anesthesia due to fear of being
awake during the operation, fear of the eye block procedure, or unpleas-ant recall
of a previous eye block or local eye proce-dure. General anesthesia is
indicated in children and uncooperative patients, as even small head move-ments
can prove disastrous during microsurgery.
PREMEDICATION
Patients undergoing eye surgery may be apprehen-sive, particularly if
they have undergone multiple procedures or there is a possibility of permanent
blindness. However, premedication must be admin-istered with caution and only
after careful consider-ation of the patient’s medical status. Adult patients
are often elderly, with myriad systemic illnesses, such as hypertension,
diabetes mellitus, and coro-nary artery disease. Pediatric patients may have
associated congenital disorders.
INDUCTION
The choice of induction technique for eye
surgery usually depends more on the patient’s other medical problems than on
the patient’s eye disease or the specific operation contemplated. One exception
isthe patient with a ruptured globe. The key to inducing anesthesia in a
patient with an openeye injury is controlling intraocular pressure with a
smooth induction. Specifically, coughing during intubation must be avoided by
achieving a deep level of anesthesia and profound paralysis. The intraocu-lar
pressure response to laryngoscopy and endotra-cheal intubation can be moderated
by prior administration of intravenous lidocaine (1.5 mg/kg) or an opioid (eg,
remifentanil 0.5–1 mcg/kg or alfen-tanil 20 mcg/kg). A nondepolarizing muscle
relax-ant or succinylcholine may be used. Despite theoretical concerns,
succinylcholine has not been shown to increase the likelihood of vitreous loss
with open eye injuries. Many patients with open globe injuries have full
stomachs and require a rapid-sequence induction technique because of the risk
of aspiration (see Case Discussion below).
MONITORING & MAINTENANCE
Eye surgery necessitates positioning the
anesthesia provider away from the patient’s airway, making close monitoring of
pulse oximetry and the cap-nograph particularly important. Endotracheal tube
kinking, breathing circuit disconnection, and unin-tentional extubation may be
more likely because of the surgeon working near the airway. Kinking and
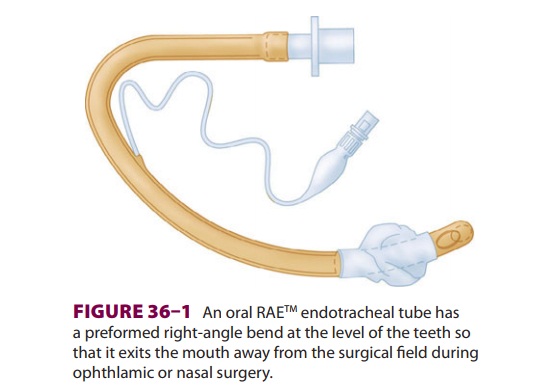
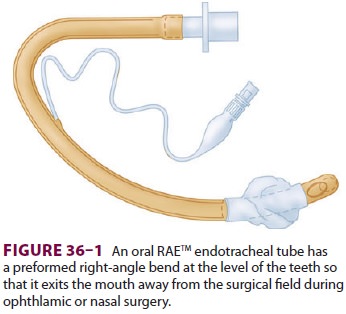
obstruction can be minimized by using a wire-rein-forced or preformed oral RAE® (Ring-Adair-Elwyn)
endotracheal tube (see Figure 36–1).
The possibil-ity of arrhythmias caused by the oculocardiac reflex increases the
importance of constantly scrutinizing the electrocardiogram (ECG) and making
sure that
the pulse tone is audible. In contrast to
most other types of pediatric surgery, infant body temperature may rise during
ophthalmic surgery because of head-to-toe draping and insignificant body
surface exposure. End-tidal CO 2 analysis helps to differenti-ate this phenomenon from malignant
hyperthermia.
The pain and stress evoked by eye surgery are considerably less than
during a major intraabdominal or intrathoracic procedure. A lighter level of
anesthe-sia would be satisfactory if the consequences of patient movement were
not so potentially catastrophic. The lack of cardiovascular stimulation
inherent in most eye procedures combined with the need for adequate anesthetic
depth can result in hypotension in elderly individuals. This problem is usually
avoided by ensur-ing adequate intravenous hydration and administer-ing small
doses of ephedrine or phenylephrine. The practice of substituting muscle
relaxation with non-depolarizing muscle relaxants for sufficient depth of
anesthesia requires constant attention to the level of neuromuscular blockade
to avoid patient movement, injury to the eye, and a malpractice claim.
Emesis caused by vagal
stimulation is a common postoperative problem following eye surgery,
partic-ularly with strabismus repair. The Valsalva effect and the increase in
central venous pressure that accom-pany vomiting can be detrimental to the
surgical result and will increase the risk of aspiration. Intraoperative
intravenous administration of a 5-HT3 antagonist (eg, ondansetron)
decreases the incidence of postopera-tive nausea and vomiting (PONV).
Dexamethasone (8–10 mg in adults) should also be considered for patients with a
strong history of PONV.
EXTUBATION & EMERGENCE
A smooth emergence from general anesthesia is
very important in order to minimize the risk of postop-erative wound dehiscence.
Coughing or gagging due to stimulus from the endotracheal tube can be minimized
by extubating the patient at a moderately deep level of anesthesia. As the end
of the surgical procedure approaches, muscle relaxation is reversed, and
spontaneous respiration is allowed to return. Anesthetic agents may be
continued during gentle suction of the airway. Nitrous oxide, if used, is then
discontinued, and intravenous lidocaine (1.5 mg/ kg) can be given to blunt
cough reflexes temporar-ily. Extubation proceeds 1–2 min after the lidocaineadministration
and during spontaneous respira-tion with 100% oxygen. Proper airway maintenance
is crucial until the patient’s cough and swallowing reflexes return. Obviously,
this technique is not appropriate in patients at increased risk of aspiration.
Severe discomfort is unusual following eye
sur-gery. Scleral buckling procedures, enucleation, and ruptured globe repair
are the most painful opera-tions. Modest incremental doses of intravenous
opi-oid (eg, fentanyl 25 mcg or hydromorphone 0.25 mg for an adult) usually
provide sufficient analgesia. The surgeon should be alerted if severe pain is
noted fol-lowing emergence from general anesthesia, as it may signal
intraocular hypertension, corneal abrasion, or other surgical complications.
Related Topics