Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Ophthalmic Surgery
Anesthesia for Intraocular Pressure Dynamics
INTRAOCULAR PRESSURE DYNAMICS
Physiology of Intraocular Pressure
The eye can be considered a hollow sphere
with a rigid wall. If the contents of the sphere increase, the intraocular pressure (normal: 12–20 mm Hg) must rise. For example, glaucoma is caused by an
obstruction to aqueous humor outflow. Similarly, intraocular pressure will rise
if the volume of blood within the globe is increased. A rise in venous
pres-sure will increase intraocular pressure by decreasing aqueous drainage and
increasing choroidal blood volume. Extreme changes in arterial blood pressure
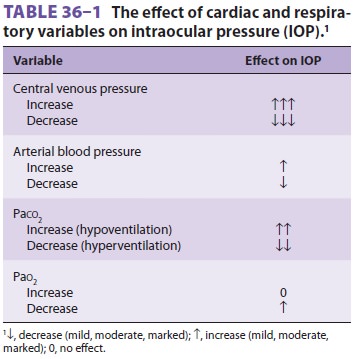
and ventilation can also affect intraocular pressure (Table
36–1). Any event that alters these parameters
(eg, laryngoscopy, intubation, airway obstruction, coughing, Trendelenburg
position) can affect intra-ocular pressure.
Alternatively, decreasing the size of the
globe without a proportional change in the volume of its contents will increase
intraocular pressure. Pressure on the eye from a tightly fitted mask, improper
prone positioning, or retrobulbar hemorrhage can lead to a marked increase in
intraocular pressure.
Intraocular pressure helps to maintain the
shape, and therefore the optical properties, of the eye. Temporary variations
in pressure are usually well tolerated in normal eyes. For example, blinking
raises intraocular pressure by 5 mm Hg, and squint-ing (forced contraction of
the orbicularis oculi muscles) may increase intraocular pressure greater than
50 mm Hg. However, even transient episodes of increased intraocular pressure in
patients with underlying low ophthalmic artery pressure (eg,
deliberate hypotension, arteriosclerotic involvement of the retinal
artery) may jeopardize retinal perfu-sion and cause retinal ischemia.
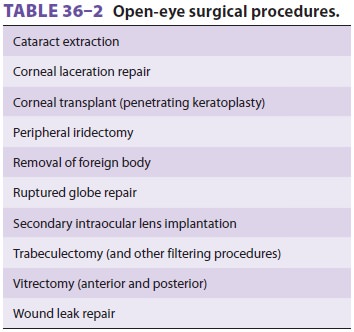
When the globe is open by surgical incision (Table
36–2) or traumatic perforation, intraocularpressure approaches atmospheric pressure.
Any factor that increases intraocular pressure in the
setting of an open globe may cause drainage
of aque-ous or extrusion of vitreous through the wound. The
latter is a serious complication that can permanently worsen vision.
Effect of Anesthetic Drugs on Intraocular Pressure
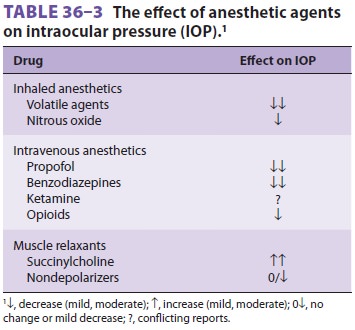
Most anesthetic drugs either lower
intraocular pres-sure or have no ef fect (Table 36–3). Inhalational anesthetics decrease intraocular pressure in propor-tion
to the depth of anesthesia. The decrease has multiple causes: a drop in blood
pressure reduces choroidal volume, relaxation of the extraocular mus-cles
lowers wall tension, and pupillary constriction facilitates aqueous outflow.
Intravenous anesthetics also decrease intraocular pressure, with the excep-tion
of ketamine, which usually raises arterial blood pressure and does not relax
extraocular muscles.
Topically administered anticholinergic drugs
result in pupillary dilation (mydriasis), which may precipitate or worsen
angle-closure glaucoma. Systemically administered atropine or glycopyrrolate
for premedication are not associated with intraocu-lar hypertension, even in
patients with glaucoma.Succinylcholine increases intraocular pressure by 5–10
mm Hg for 5–10 min after administration, principally through prolonged
contracture of the extraocular muscles. However, in studies of hundreds of
patients with open eye injuries, no patient experienced extrusion of ocular
contents after administration of succinylcholine. Unlike other skeletal muscle,
extraocular muscles contain myo-cytes with multiple neuromuscular junctions,
and repeated depolarization of these cells by succinyl-choline causes the
prolonged contracture. The result-ing increase in intraocular pressure may have
several effects. It will cause spurious measurements of intra-ocular pressure
during examinations under anes-thesia in glaucoma patients, potentially leading
to unnecessary surgery. Lastly, prolonged contracture of the extraocular
muscles may result in an abnor-mal forced duction test, a maneuver utilized in
stra-bismus surgery to evaluate the cause of extraocular muscle imbalance and
determine the type of surgical correction. Nondepolarizing neuromuscular block-ers
(NMBs) do not increase intraocular pressure.
Related Topics