Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Otorhinolaryngologic Surgery
Anesthesia for Endoscopy
ENDOSCOPY
Endoscopy includes laryngoscopy (diagnostic and operative),
microlaryngoscopy (laryngoscopy aided by an operating microscope),
esophagos-copy, and bronchoscopy. Endoscopic procedures may be accompanied by
laser surgery.
Preoperative Considerations
Patients presenting for endoscopic surgery
are often being evaluated for voice disorders (often present-ing as
hoarseness), stridor, or hemoptysis. Possible diagnoses include foreign body
aspiration, trauma to the aerodigestive tract, papillomas, tracheal stenosis,
tumors, or vocal cord dysfunction. Thus, a preopera-tive medical history and
physical examination, with particular attention to potential airway problems,
must precede any decisions regarding the anes-thetic plan. In some patients,
flow–volume loops or radiographic, computed tomogra-phy, or magnetic resonance
imaging studies may be available for review. Many patients will have under-gone
preoperative indirect laryngoscopy or fiberop-tic nasopharyngoscopy, and the
information gained from these procedures may be of critical importance.
Important initial questions that must be answered are whether the
patient can be provided with positive-pressure ventilation with a face mask and
rebreathing bag, and whether the patient can be intubated using conventional
direct or video laryngoscopy. If the answer to either question is not “yes,”
the patient’s airway should be secured prior to induction using an alternative
technique (eg, use of a fiberoptic bronchoscope or a tracheostomy under local
anesthesia; see Case Discussion). However, even the initial securing of an
airway with tracheostomy does not prevent intraoperative air-way obstruction
due to surgical manipulation and techniques.
Sedative premedication should be avoided in a patient with medically
important upper airway obstruction. Glycopyrrolate (0.2–0.3 mg
intramus-cularly) 1 hr before surgery may prove helpful by minimizing
secretions, thereby facilitating airway visualization.
Intraoperative Management
The anesthetic goals for laryngeal endoscopy
include an immobile surgical field and adequate masseter muscle relaxation for
introduction of the suspension laryngoscope (typically the result of profound
muscle paralysis), adequate oxygenation and ventilation, and cardiovascular
stability despite rapidly varying levels of surgical stimulation.
A. Muscle Relaxation
Intraoperative muscle relaxation can be
achieved by intermittent boluses or infusion of intermediate-duration
nondepolarizing neuromuscular block-ing agents (NMBs) (eg, rocuronium,
vecuronium, cisatracurium), or with a succinylcholine infusion. However,
profound degrees of nondepolarizing block may prove difficult to reverse and
may delay return of protective airway reflexes and extubation. Given that
profound relaxation is often needed until the very end of the surgery,
endoscopy remains one of the few remaining indications for succinylcholine
infusions. Rapid recovery is important, as endos-copy is often an outpatient
procedure.
B. Oxygenation & Ventilation
Several methods have successfully been used
to provide oxygenation and ventilation during endos-copy, while simultaneously
minimizing interference with the operative procedure. Most commonly, the
patient is intubated with a small-diameter endo-tracheal tube through which
conventional posi-tive-pressure ventilation is administered. Standard tracheal
tubes of smaller diameters, however, are designed for pediatric patients, and
therefore are too short for the adult trachea and have a low-volume cuff that
will exert high pressure against the tra-cheal mucosa. A 4.0-, 5.0-, or 6.0-mm
specialized microlaryngeal tracheal tube (Mallinckrodt MLT®, Mallinckrodt
Critical Care) is the same length as an adult tube, has a disproportionately
large high-vol-ume low-pressure cuff, and is stiffer and less prone to
compression than is a conventional tracheal tube of the same diameter. The
advantages of intubation in endoscopy include protection against aspiration and
the ability to administer inhalational anesthetics and to continuously monitor
end-tidal CO 2.
In some cases (eg, those involving the poste-rior commissure or vocal
cords), intubation with a tracheal tube may interfere with the surgeon’s
visualization or performance of the procedure. A simple alternative is
insufflation of high flows of oxygen through a small catheter placed in the
tra-chea. Although oxygenation may be maintained in patients with good lung
function, ventilation will be inadequate for longer procedures unless the
patient is allowed to breathe spontaneously.
Another option is the intermittent apnea tech-nique, in which
ventilation with oxygen by face mask or endotracheal tube is alternated with
peri-ods of apnea, during which the surgical procedure is performed. The
duration of apnea, usually 2–3 min, is determined by how well the patient
maintains oxygen saturation, as measured by pulse oximetry. Risks of this
technique include hypoventilation with hypercarbia, failure to reestablish the
airway, and pulmonary aspiration.
Another attractive alternative approach
involves connecting a manual jet ventilator to a side port of the laryngoscope.
During inspiration (1–2 s), a high-pressure (30–50 psi) jet of oxygen is
directed through the glottic opening and entrains a
mixture of oxygen and room air into the lungs
(Venturi effect). Expiration (4–6 s duration) is passive.
It is crucial to monitor chest wall motion and to
allow sufficient time for exhalation to avoid air trapping and barotrauma. This
technique requires total intravenous anesthesia. A variation of this technique
is high-frequency jet ventilation, which utilizes a small cannula or tube in
the trachea, through which gas is injected 80–300 times per min-ute .
Capnography will not provide an accurate estimate of end-tidal CO 2 during
jet ven-tilation due to constant and sizable dilution of alveo-lar gases.
C. Cardiovascular Stability
Blood pressure and heart rate often fluctuate strik-ingly during
endoscopic procedures for two rea-sons. First, some of these patients are
elderly and have a long history of heavy tobacco and alcohol use that
predisposes them to cardiovascular dis-eases. In addition, the procedure is, in
essence, a series of physiologically stressful laryngoscopies and
interventions, separated by varying periods of minimal surgical stimulation.
Attempting to main-tain a constant level of anesthesia invariably results in
alternating intervals of hypertension and hypo-tension. Providing a modest
baseline level of anes-thesia allows supplementation with short-acting
anesthetics (eg, propofol, remifentanil) or sympa-thetic antagonists (eg, esmolol),
as needed, dur-ing periods of increased stimulation. Alternatively, some
anesthesia providers use regional nerve blockof the glossopharyngeal
nerve and superior laryn-geal nerve to help minimize intraoperative swings in
blood pressure (see Case Discussion).
Laser Precautions
Laser light differs from ordinary light in
three ways: it is monochromatic (possesses one wavelength), coherent
(oscillates in the same phase), and colli-mated (exists as a narrow parallel
beam). These char-acteristics offer the surgeon excellent precision and
hemostasis with minimal postoperative edema or pain. Unfortunately, lasers
introduce several major hazards into the operating room environment.
The uses and side effects of a laser vary
with its wavelength, which is determined by the medium in which the laser beam
is generated. For example, a CO2 laser produces a long wavelength (10,600 nm), whereas a
yttrium–aluminum–garnet (YAG) laser produces a shorter wavelength (1064- or
1320-nm). As the wavelength increases, absorption by water increases, and
tissue penetration decreases. Thus, the effects of the CO2 laser are much more localized and
superficial than are those of the YAG laser.
General laser precautions include the
evacuation of toxic fumes (laser plume) from tissue vaporiza-tion; these have
the potential to transmit microbio-logical diseases. When significant laser
plume is generated, fitted respiratory filter masks compliant with Occupation
Safety and Health Administration standards should be worn by all operating room
personnel. In addition, during laser procedures, all operating room personnel
should wear laser eye protection, and the patient’s eyes should be taped shut.
The greatest risk of laser airway surgery (if an endotracheal tube is used) is
an airway fire.This risk can be moderated by using a technique of ventilation
that minimizes the fraction of inspired oxygen (Fio2) and can be eliminated if
there is no combustible material (eg, no flammable tube or catheter) in the
airway. If an endotracheal tube is used, it must be relatively resistant to
laser igni-tion (Table 37–1). These tubes not only resist laser beam strikes,
but they also possess double cuffs that should be inflated with saline instead
of air in order to better absorb thermal energy and reduce the risk of
ignition. If the proximal cuff is struck by the laser
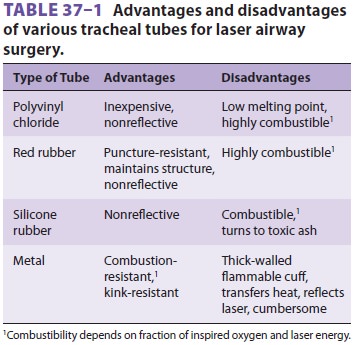
and the saline escapes, the distal cuff will
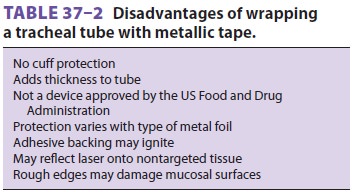
continue to seal the airway. Alternatively, endotracheal tubes can be wrapped
with a variety of metallic tapes; however, this is a suboptimal practice and
should be avoided whenever use of a specialized, commercially available,
flexible, stainless steel laser-resistant endo-tracheal tube is possible (Table
37–2).
Although specialized, laser-resistant
endotra-cheal tubes may be used, it must be emphasized that no endotracheal
tube or currently available endotra-cheal tube protection device is reliably
laser-proof.
Therefore, whenever laser airway surgery is
being performed with an endotracheal tube in place, the following precautions
should be observed:
·
Inspired oxygen
concentration should be as low as possible by utilizing air in the inspired gas
mixture (many patients tolerate an Fio2 of 21%).
·
Nitrous oxide supports combustion and
should be avoided.
·
The endotracheal tube cuffs should be
filled with saline. Some practitioners add methylene blue to signal cuff
rupture. A well-sealed cuffed tube will minimize oxygen concentration in the
pharynx.
·
Laser intensity and duration should
be limited as much as possible.
·
Saline-soaked pledgets (completely
saturated) should be placed in the airway to limit risk of endotracheal tube
ignition and damage to adjacent tissue.
·
A source of water (eg,
60-mL syringe) should be immediately available in case of fire.
These precautions limit, but do not eliminate, the risk of an airway
fire; anesthesia providers must proactively address the hazard of fire whenever
laser or electrocautery is utilized near the airway (Table 37–3).
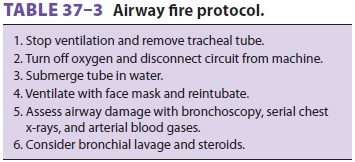
If an airway fire should occur, all air/oxygen should immediately be
turned off at the anesthe-sia gas machine, and burning combustible material
(eg, an endotracheal tube) should be removed from the airway. The fire can be
extinguished with saline, and the patient’s airway should be examined to be
certain that all combustible fragments have been removed.
Related Topics