Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Otorhinolaryngologic Surgery
Anesthesia for Head & Neck Cancer Surgery
HEAD & NECK CANCER SURGERY
Surgery for cancer of the head and neck
includes laryngectomy, glossectomy, pharyngectomy, paroti-dectomy,
hemimandibulectomy, and radical neck dissection. An endoscopic examination
following induction of anesthesia often precedes these surgical procedures.
Timing of a tracheostomy, if planned, depends upon the patient’s preoperative
airway compromise. Some procedures may include exten-sive reconstructive
surgery, such as the transplanta-tion of a free microvascular muscle flap.
Preoperative Considerations
The typical patient presenting for head and
neck cancer surgery is older and often has had many years of heavy tobacco and
alcohol use. Common coexist-ing medical conditions include chronic obstructive
pulmonary disease, coronary artery disease, hyper-tension, diabetes,
alcoholism, and malnutrition. Airway management may be complicated by abnormal
airway anatomy, an obstructing lesion, or by preoperative radiation therapy
that has fibrosed, immobilized, and distorted the patient’s airwaystructures.
If there is concern regarding poten-tial airway problems, intravenous inductionmay be
avoided in favor of awake direct or fiberoptic laryngoscopy (cooperative
patient) or direct or fiberoptic intubation following an inhalational
induction, maintaining spontaneous ventilation (uncooperative patient).
Elective tracheostomy under local anesthesia prior to induction of general
anesthesia is often a prudent option. In any case, the appropriate equipment
and qualified personnel required for an emergency tracheostomy must be immediately available.
Intraoperative Management
A. Monitoring
Because many of these procedures are lengthy
and associated with substantial blood loss, and because of the prevalence of
coexisting cardiopulmonary disease, arterial cannulation is often utilized for
blood pressure monitoring and frequent laboratory analyses. If central venous
access is deemed neces-sary, the surgeon should be consulted to ascertain that
planned internal jugular or subclavian venous access will not interfere with
the intended surgical procedures; in such cases, if both internal jugular and
both subclavian veins are unavailable, antecu-bital or femoral veins are
reasonable alternatives. Arterial lines and intravenous cannulas should not be
placed in the operative arm if a radial fore-arm flap is planned. A minimum of
two large-bore intravenous lines and a urinary catheter (preferably with
temperature-monitoring capability) should be placed. A forced-air warming
blanket should be positioned over the lower extremities to help main-tain
normal body temperature. Intraoperative hypo-thermia and consequent
vasoconstriction can be detrimental to perfusion of a microvascular free flap.
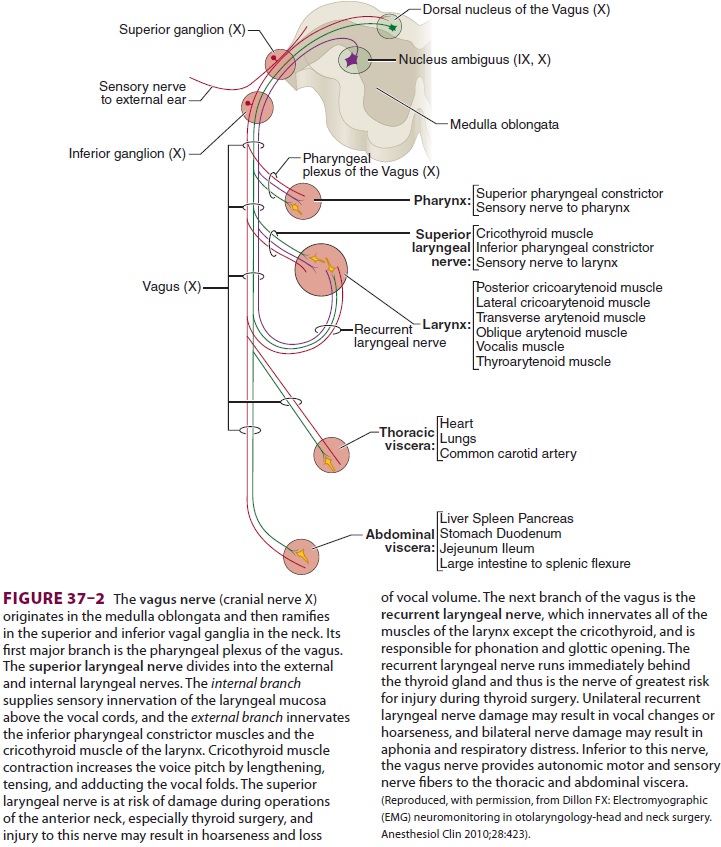
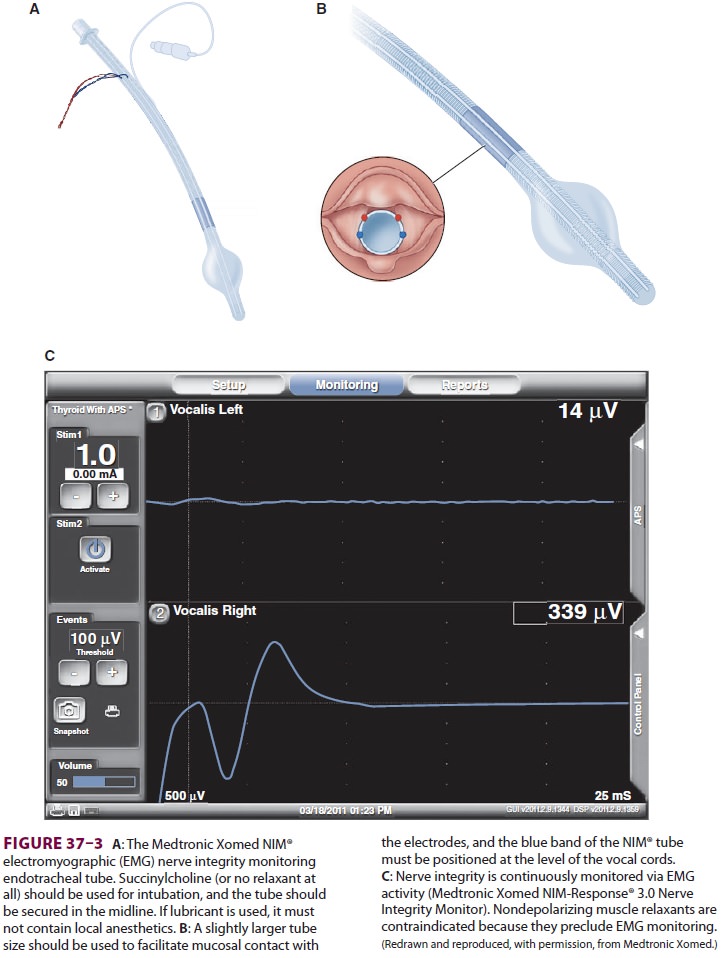
Intraoperative nerve monitoring is increasingly utilized by surgeons in
anterior neck operations to help preserve the superior laryngeal, recur-rent
laryngeal, and vagus nerves (Figure 37–2), and the anesthesia provider may be asked to place a specialized nerve
integrity monitor endotracheal tube (Medtronic Xomed NIM® endotracheal tube) to
facilitate this process (Figure 37–3).
B. Tracheostomy
Head and neck cancer surgery often includes tra-cheostomy. Immediately
prior to surgical entry into the trachea, the endotracheal tube and
hypo-pharynx should be thoroughly suctioned to limit the risk of aspiration of
blood and secretions. If electrocautery is used during the surgical
dissec-tion, the Fio2 should be lowered to 30% or
less, if possible, in order to minimize the risk of fire as the trachea is
surgically entered. In any case, the easiest way to avoid an airway fire in
this circumstance is for the surgeon NOT to use the cautery to enter the
trachea. After dissection down to the trachea, the tracheal tube cuff is
deflated to avoid perforation by the scalpel. When the tracheal wall is
transected, the endotracheal tube is withdrawn so that its tip is immediately
cephalad to the incision. Ventilation during this period is difficult because
of the large leak through the tracheal incision. A sterile wire-reinforced
endotracheal tube or L-shaped cuffed laryngectomy tube is placed in the trachea,
the cuff is inflated, and the tube is connected to a ster-ile breathing
circuit. As soon as correct position is confirmed by capnography and bilateral
chest auscultation, the original endotracheal tube is removed. An increase in
peak inspiratory pressure immediately after tracheostomy usually indicates a
malpositioned endotracheal tube, bronchospasm, debris or secretions in the
trachea, or, rarely, pneumothorax.
C. Maintenance of Anesthesia
The surgeon may request the omission of NMBs during neck dissection or parotidectomy to identify nerves (eg, spinal accessory, facial nerves) by direct stimulation and to preserve them. If a nerve integrity monitor endotracheal tube is utilized, succinylcholine (or propofol with no relax-ant) may be used to facilitate intubation. Moderate controlled hypotension may be helpful in limiting blood loss; however, cerebral perfusion may be com-promised with moderate hypotension when a tumor invades the carotid artery or jugular vein (the latter may increase cerebral venous pressure). If head-up tilt is utilized, it is important that the arterial blood pressure transducer be zeroed at the level of the brain (external auditory meatus) in order to most accurately determine cerebral perfusion pressure. In addition, head-up tilt may increase the chance of venous air embolism.Following reanastomosis of a microvascular free flap, blood pressure should be maintained at the patient’s baseline level. The use of vasoconstric-tive agents (eg, phenylephrine) to maintain systemic blood pressure should be minimized because of potential decrease in flap perfusion due to vaso-constriction. Similarly, the use of vasodilators (eg, sodium nitroprusside or hydralazine) should be avoided in order to minimize any decrease in graft perfusion pressure.
D. Transfusion
Transfusion decisions must balance the
patient’s immediate surgical risks with the possibility of an increased cancer
recurrence rate resulting from trans-fusion-induced immune suppression.
Rheological factors make a relatively low hematocrit (eg, 27% to 30%) desirable
when microvascular free flaps are performed. Excessive diuresis should be
avoided dur-ing microvascular-free flap surgery in order to allow adequate
graft perfusion in the postoperative period.
E. Cardiovascular Instability
Manipulation of the carotid sinus and
stellate ganglion during radical neck dissection (theright side more than the
left) has been associated with wide swings in blood pressure, bradycardia,
arrhythmias, sinus arrest, and prolonged QT inter-vals. Infiltration of the
carotid sheath with local anesthetic will usually moderate these problems.
Bilateral neck dissection may result in postoperative hypertension and loss of
hypoxic drive due to dener-vation of the carotid sinuses and carotid bodies.
Related Topics