Chapter: Medical Surgical Nursing: Management of Patients With Infectious Diseases
Preventing Infection in the Community
PREVENTING INFECTION IN THE COMMUNITY
Prevention and control
of infection in the community are goals shared by the CDC and state and local
public health depart-ments. Much of public health emphasis is placed on
prevention to avoid outbreaks and other situations that require control.
Methods of infection prevention include sanitation techniques (eg, water
purification, disposal of sewage and other potentially infectious materials),
regulated health practices (eg, handling, storage, packaging, preparation of
food by institutions), and im-munization programs. In the United States,
immunization pro-grams have markedly decreased the incidence of infectious
diseases.
Vaccination Programs
The goal of vaccination
programs is to use wide-scale efforts to prevent specific infectious diseases
from occurring in a popula-tion. Public health decisions about vaccine campaign
implemen-tation efforts are complex. Risks and benefits for the individual and
the community must be evaluated in terms of morbidity, mortality, and financial
benefit.
The most successful
vaccine programs are those for the pre-vention of smallpox, measles, mumps,
rubella, chicken pox, polio, diphtheria, pertussis, and tetanus. Concerns that
smallpox may be reintroduced as an act of biowarfare have led to a decision
that medical first responders and selected others should again re-ceive small
pox vaccine.
More than 25 vaccines
are licensed in the United States. Vac-cines are made of antigen preparations
in a suspension and are in-tended to produce a human immune response to protect
the host from future encounters with the organism. No vaccine is com-pletely
safe for all recipients. Some people are allergic to the anti-gen or the
carrier substance. When live organisms are used as antigen, the actual disease
(often with a modified course) may fol-low. Contraindications on package
inserts of a vaccine must be heeded. These guidelines detail studied experience
with allergy and other complications and provide crucial information about
refrigeration, storage, dosage, and administration.
Variations to the
recommended vaccination schedule should be made on a case-by-case basis,
depending on the patient’s risk factors and ability to return for follow-up
vaccinations at the ap-pointed time. For example, although the first dose of
measles vac-cine is recommended at the age of 12 to 15 months, babies in
developing countries (where measles contributes significantly to childhood
morbidity and mortality) should be vaccinated at 9 months.
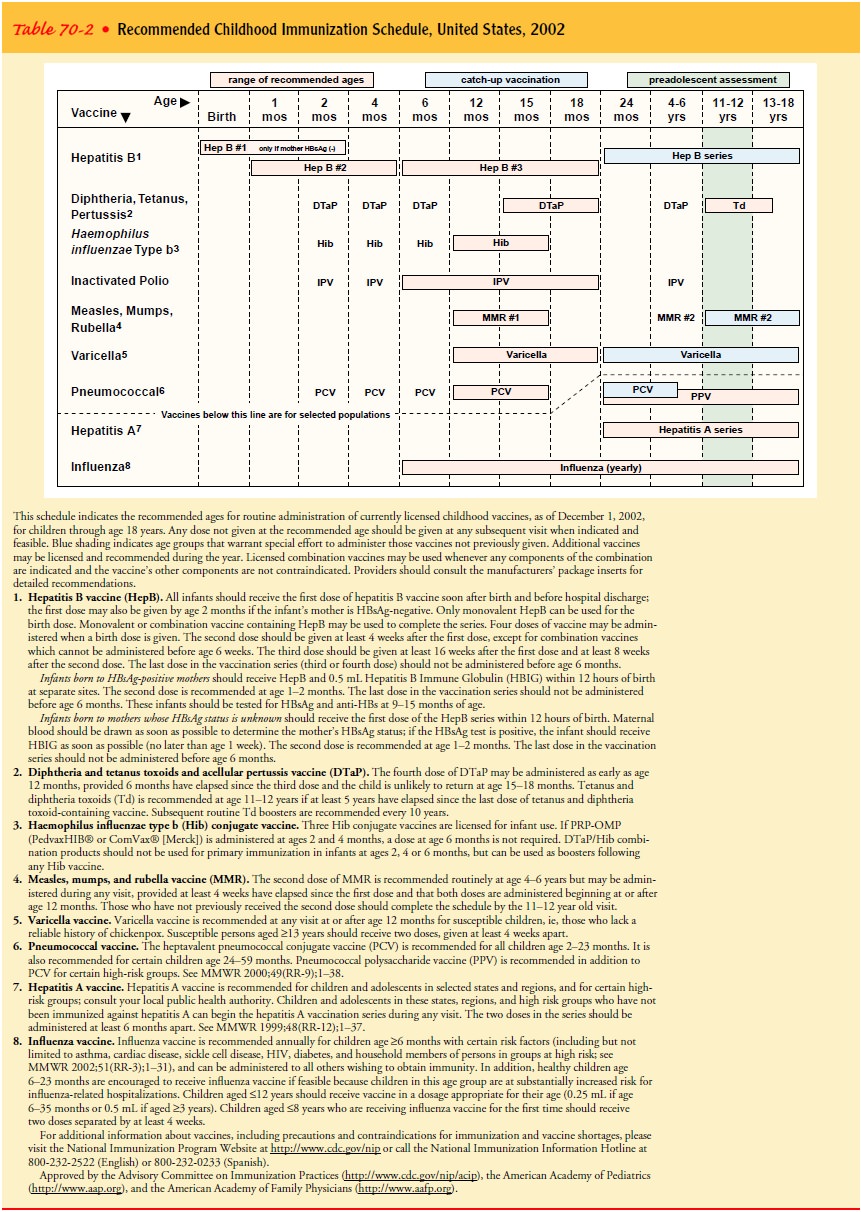
The standard recommended
vaccination schedule for infants and children as developed by the CDC is shown
in Table 70-2. The schedule is revised as epidemiologic evidence warrants, and
nurses are advised to consult the CDC to determine the most recent schedule.
Vaccine recommendations
for adults are designed to protect those with underlying diseases that increase
infection risk, those with potential for occupational exposure, and those who
may be exposed to infectious agents during travel. Immunosuppressed adults
(including those who have had splenectomy) should be vaccinated for
pneumococcus (Streptococcus pneumoniae),
menin-gococcus (Neisseria meningitidis),
and Haemophilus influenzae. Health care
workers should be immune to measles, mumps, rubella, hepatitis B, and
varicella. It is strongly recommended that all of the previously described
adult groups and those with asthma or other chronic respiratory conditions
receive annual influenza vaccine.
Information about
individual vaccines or the most current vaccine schedules may be found on the
Internet. The CDC also provides a 24-hour telephone hotline (800-232-2522) for
information about routine pediatric or adult vaccine advice. Advice about op-timal
vaccination for travelers is available on the Internet, by phone
(877-FYI-TRIP), and by a toll-free fax number (888-232-3299) to request
information.
Nurses should ask
parents or adult vaccine recipients to pro-vide information about any problems
encountered after vaccina-tion. As mandated by law, a Vaccine Adverse Event
Reporting System (VAERS) form must be completed with the followinginformation:
type of vaccine received, timing of vaccination, onset of the adverse event,
current illnesses or medication, history of adverse events after vaccination
and demographic information about the recipient. Forms are obtained by phoning
1-800-822-7967 or through the Internet.
The incidence of
vaccine-preventable diseases, such as measles, mumps, rubella, and diphtheria,
is affected by immigration from developing countries. Vaccine campaigns in
developing countries are often financially and logistically constrained, and
immigrants from such areas may be more likely than U.S. residents to be
un-protected and may increase the potential pathways for epidemic spread.
Individual risk and epidemic risk are reduced when vac-cination campaigns reach
all communities, including those with a high proportion of immigrants.
CONTRAINDICATIONS
Patients who have experienced previous anaphylaxis or
similar reactions; patients who have developed encephalopathy within 7 days of
a previous diphtheria, tetanus, and pertussis (DTP) dose; and those who have
developed other moderate or severe sequelae after a previous dose should not
receive further doses. DTP is often deferred for the child who previously
developed a fever higher than 40°C (104°F) within 48 hours of vaccination or who had a seizure or
developed a shocklike state within 3 days of previous vaccination. Live
vaccines usually are not indicated for patients or close contacts of patients
with severe immuno-suppression (eg, HIV infection, leukemia, lymphoma,
generalized malignancy, significant corticosteroid use, use of
immuno-suppressive medications to prevent transplant rejection). The measles,
mumps, and rubella vaccine should not be administered to pregnant women.
MEASLES, MUMPS, AND RUBELLA VACCINE
Since the measles,
mumps, and rubella (MMR) vaccines were li-censed, reported cases of these
diseases have decreased by more than 99% in the United States (ie, fewer than
500 cases per year since 1999). All public health departments are encouraged to
vig-orously promote vaccination for all children and for susceptible adults
unless contraindicated. Routine MMR vaccination should be given to children at
12 to 15 months of age, with repeat dosing at 4 to 6 years of age (Atkinson et al.,
2002).
All who work in health care should demonstrate immunity
to these three viruses by one of the following: birth date before 1957,
documented administration of two doses of vaccine, laboratory evidence of
immunity, or documentation of physician-diagnosed measles or mumps.
Side Effects.
Epidemiologic evidence supports that the risk
forside effects is greater in nonimmune vaccine recipients than in those
receiving repeat doses. Patients should be advised that fever, transient
lymphadenopathy, or hypersensitivity reaction might occur. Antipyretics may be
used to decrease the risk for fever, but aspirin should be avoided in infants
and children because of the risk for Reye’s syndrome.
VARICELLA (CHICKENPOX) VACCINE
Varicella zoster is the causative viral agent of chickenpox and herpes zoster. In its natural state, the varicella virus attacks most individuals as children, causing disseminated disease in the form of chickenpox. Chickenpox is often more severe in adults. Transmission occurs by the airborne and contact routes. With rare exception, varicella infects an individual only once.
The incubation period is about
2 weeks (range, 10 to 21 days). During a prodrome of general malaise (often
noticed about 2 days before the rash develops), the newly infected host is
capable of trans-mitting the virus to other susceptible contacts. Typically,
the rash is vesicular and pustular and spreads rapidly from few to many
le-sions in a matter of hours. New lesion formation continues for 2 to 3 days,
with lesions appearing at different stages throughout this time. By the fourth
symptomatic day, the lesions begin to dry, and new lesions usually do not
develop. Fever is common during the 4 to 6 days of rash progression. When the
lesions have crusted, the patient is no longer contagious to others.
Herpes zoster, also
known as shingles, is a localized rash caused by recurrent varicella. Vesicles
are restricted to areas supplied by single associated nerve groups. Varicella
may be transmitted from the rash of those with shingles to people who are
susceptible to varicella.
The varicella vaccine was first recommended as part of
the routine vaccine schedule in the United States in 1996. The vac-cine is
effective in preventing chickenpox in approximately 85% of those vaccinated and
significantly reduces the severity in almost all those who get the disease
despite vaccination (Atkinson et al., 2002). The vaccine should not be given to
those who have de-pressed immune function, are pregnant, have received blood
products in the past 6 months, or have demonstrated allergy to varicella
vaccine.
INFLUENZA VACCINE
Influenza is an acute
viral disease that predictably and periodically causes worldwide epidemics.
Epidemics occur every 2 to 3 years, with a highly variable degree of severity.
An average estimated ex-cess of 20,000 deaths per year have been attributed to
influenza or its sequelae (ie, pneumonia and cardiopulmonary collapse) in
vulnerable groups between 1977 and 1995 (Centers for Disease Control and
Prevention [CDC], 2001d).
Each year, a new vaccine
is available. It is composed of the three virus strains (usually two type A
influenza and one type B influenza strains) considered most likely to occur in
the coming season. When the presumed influenza agents have been correctly
anticipated and included in that year’s vaccine, vaccine offers approximately
70% to 90% protection for healthy children and young adults. Although less
effective in the elderly (as low as 30% to 40% in the frail elderly), it decreases
the severity of illness in those who do get infected, is 50% to 70% effective
in preventing pneumonia and hospitalization, and is 80% effective in
prevent-ing death. In extended care facilities, risk of transmission is greatly
reduced by vaccination of all residents (CDC, 2001d).
The Immunization
Practices Advisory Committee of the Public Health Service recommends annual
influenza vaccinations for the following groups at risk for influenza
complications: those older than 50 years of age, residents of extended care
facilities, those with chronic pulmonary or cardiovascular diseases, and those
with diabetes, immunosuppression, or renal dysfunction. Vaccination is also
advised for children (eg, those with juvenile rheumatoid arthritis) who require
long-term aspirin therapy to reduce the likelihood of developing Reye’s
syndrome. Health care providers and household members of those in high-risk
groups should re-ceive the vaccine to reduce the risk of transmission to those
vul-nerable to influenza sequelae. Vaccine campaigns among health care workers
and patients should be intensified when there is evidence of community
influenza disease.
Related Topics