Chapter: Essentials of Anatomy and Physiology: The Vascular System
Pathways of Circulation
PATHWAYS OF CIRCULATION
The two major pathways of circulation are pulmonary and systemic. Pulmonary circulation begins at the right ventricle, and systemic circulation begins at the left ventricle. Hepatic portal circulation is a special segment of systemic circulation that will be covered separately. Fetal circulation involves pathways that are present only before birth and will also be discussed separately.
PULMONARY CIRCULATION
The right ventricle pumps blood into the pulmonary artery (or trunk), which divides into the right and left pulmonary arteries, one going to each lung. Within the lungs each artery branches extensively into smaller arteries and arterioles, then to capillaries. The pul-monary capillaries surround the alveoli of the lungs; it is here that exchanges of oxygen and carbon dioxide take place. The capillaries unite to form venules, which merge into veins, and finally into the two pul-monary veins from each lung that return blood to the left atrium. This oxygenated blood will then travel through the systemic circulation. (Notice that the pul-monary veins contain oxygenated blood; these are the only veins that carry blood with a high oxygen con-tent. The blood in systemic veins has a low oxygen content; it is systemic arteries that carry oxygenated blood.)
SYSTEMIC CIRCULATION
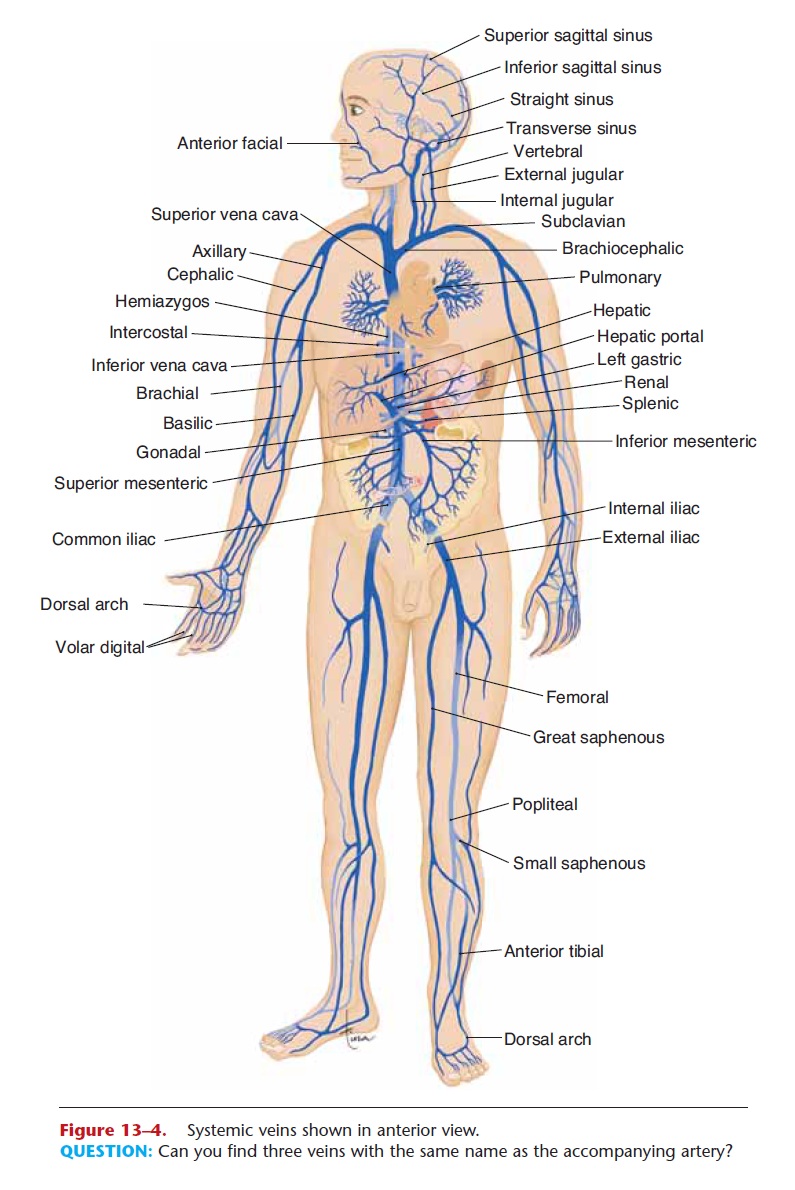
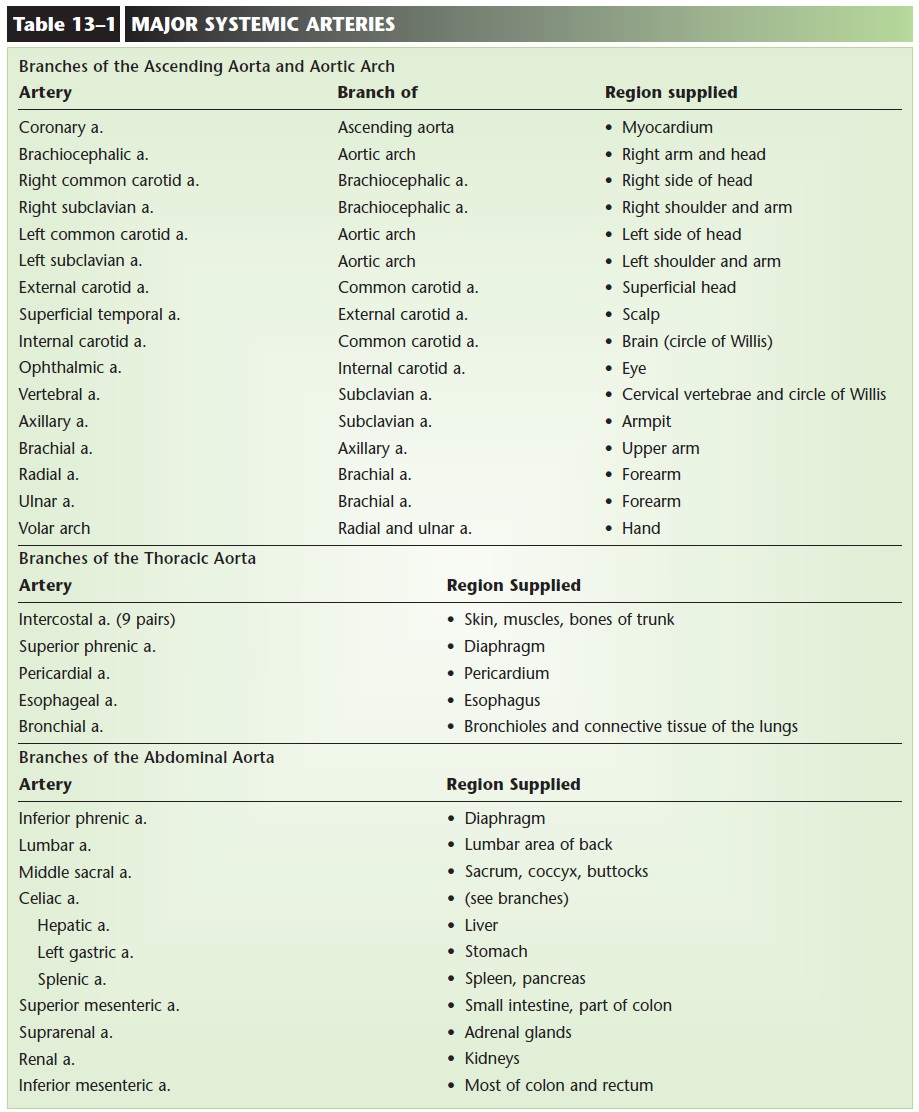
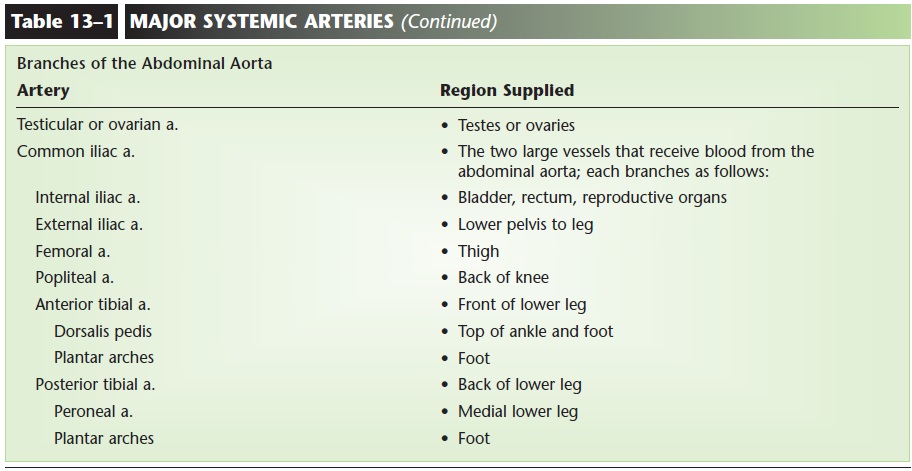
The left ventricle pumps blood into the aorta, the largest artery of the body. We will return to the aorta and its branches in a moment, but first we will sum-marize the rest of systemic circulation. The branches of the aorta take blood into arterioles and capillary net-works throughout the body. Capillaries merge to form venules and veins. The veins from the lower body take blood to the inferior vena cava; veins from the upper body take blood to the superior vena cava. These two caval veins return blood to the right atrium. The major arteries and veins are shown in Figs. 13–3 to 13–5, and their functions are listed in Tables 13–1 and 13–2.
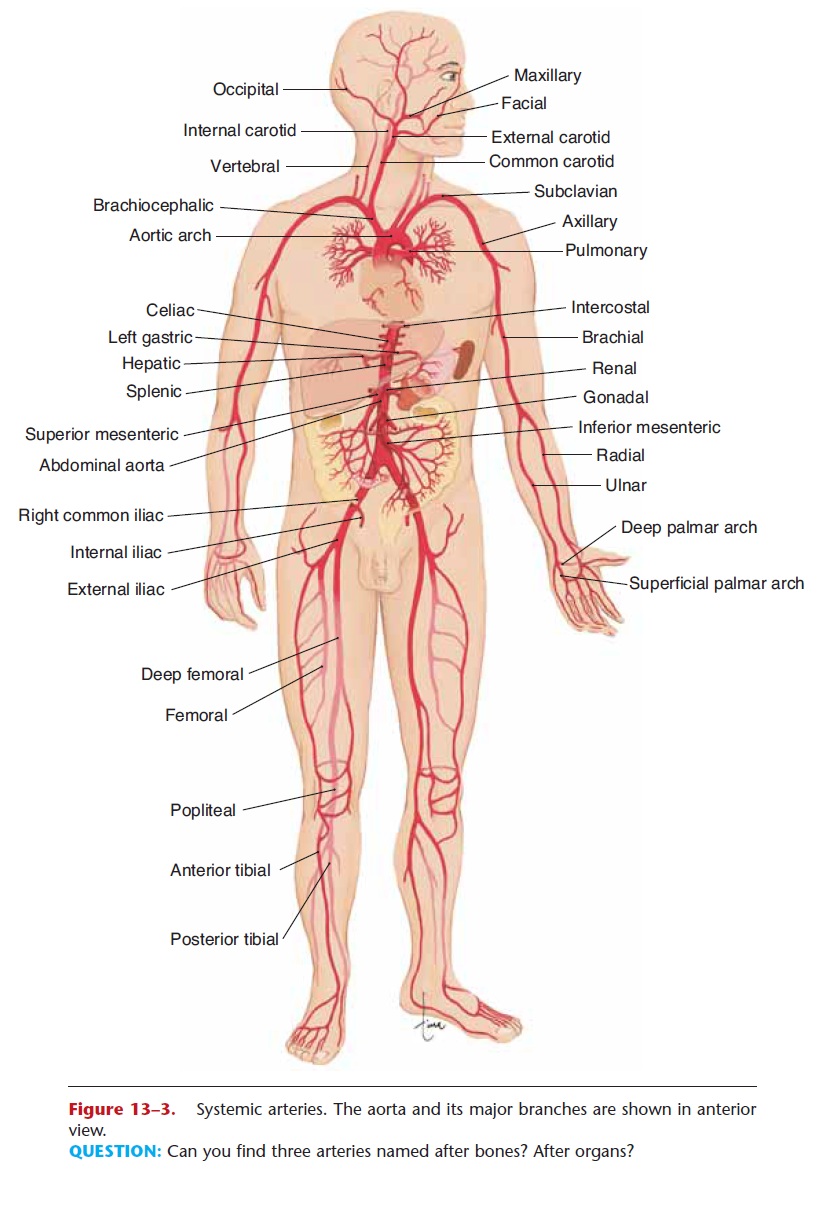
Figure 13–3. Systemic arteries. The aorta and its major branches are shown in anterior view.
QUESTION: Can you find three arteries named after bones? After organs?
The aorta is a continuous vessel, but for the sake of precise description it is divided into sections that are named anatomically: ascending aorta, aortic arch, tho-racic aorta, and abdominal aorta. The ascending aorta is the first inch that emerges from the top of the left ventricle. The arch of the aorta curves posteriorly over the heart and turns downward. The thoracic aorta continues down through the chest cavity and through the diaphragm. Below the level of the diaphragm, the abdominal aorta continues to the level of the 4th lum-bar vertebra, where it divides into the two common iliac arteries. Along its course, the aorta has many branches through which blood travels to specific organs and parts of the body.
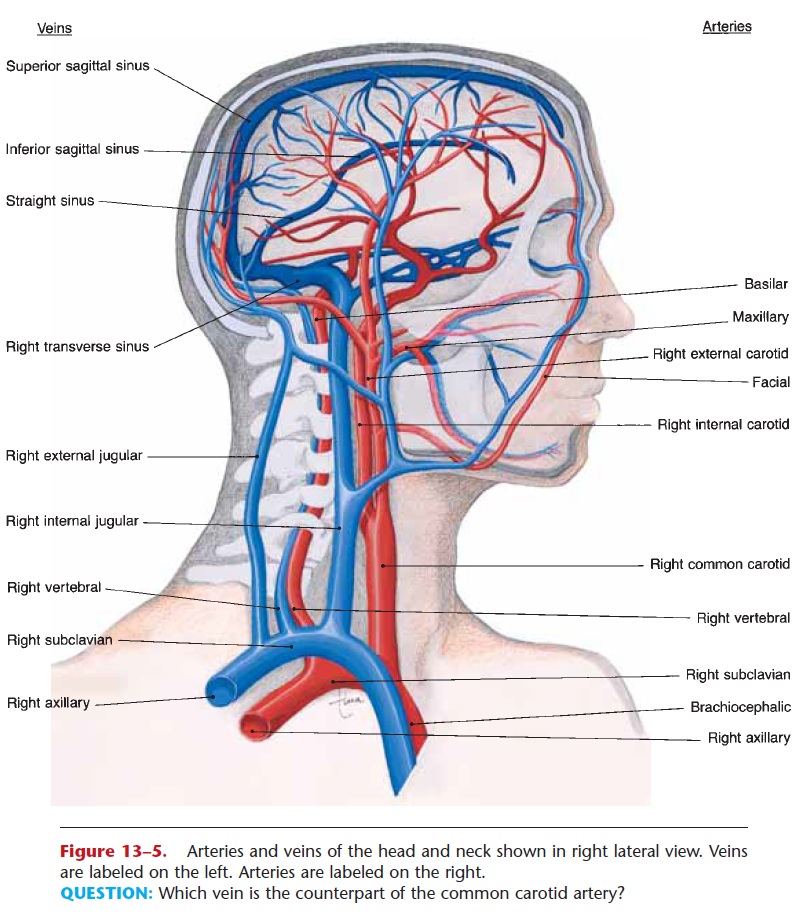
Figure 13–5. Arteries and veins of the head and neck shown in right lateral view. Veins are labeled on the left. Arteries are labeled on the right.
QUESTION: Which vein is the counterpart of the common carotid artery?
The ascending aorta has only two branches: the right and left coronary arteries, which supply blood to the myocardium.
The aortic arch has three branches that supply blood to the head and arms: the brachiocephalic artery, left common carotid artery, and left subclavian artery. The brachiocephalic (literally, “arm-head”) artery is very short and divides into the right common carotid artery and right subclavian artery. The right and left common carotid arteries extend into the neck, where each divides into an internal carotid artery and external carotid artery, which supply the head. The right and left subclavian arteries are in the shoulders behind the clavicles and continue into the arms. As the artery enters another body area (it may not “branch,” simply continue), its name changes: The subclavian artery becomes the axillary artery, which becomes the brachial artery. The branches of the carotid and sub-clavian arteries are diagrammed in Figs. 13–3 and 13–5. As you look at these diagrams, keep in mind that the name of the vessel often tells us where it is. The facial artery, for example, is found in the face.
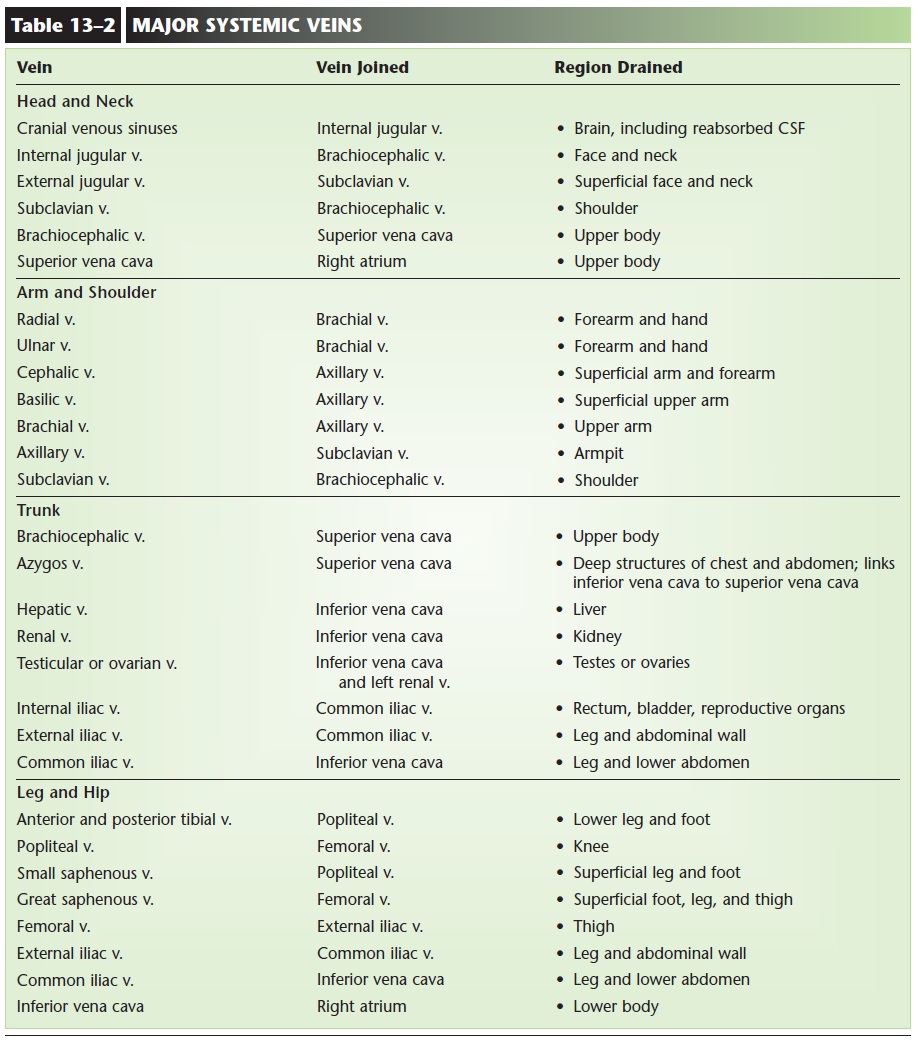
Some of the arteries in the head contribute to an important arterial anastomosis, the circle of Willis (or cerebral arterial circle), which is a “circle” of arter-ies around the pituitary gland (Fig. 13–6). The circle of Willis is formed by the right and left internal carotid arteries and the basilar artery, which is the union of the right and left vertebral arteries (branches of the subclavian arteries). The brain is always active,
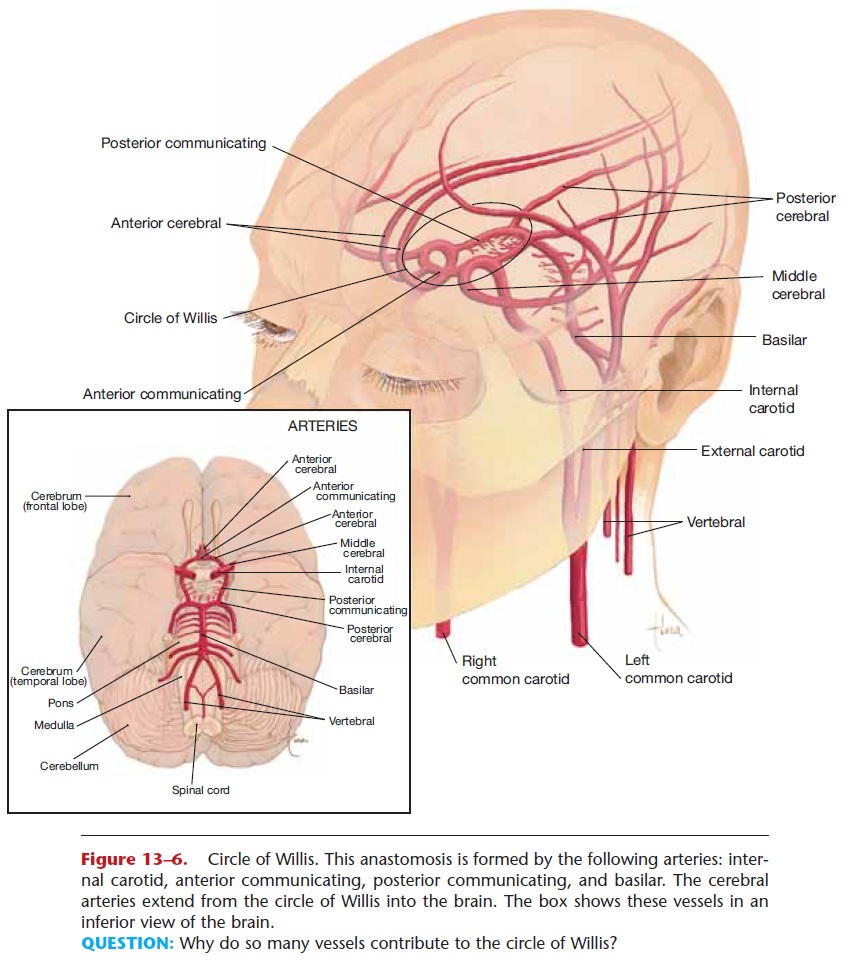
Figure 13–6. Circle of Willis. This anastomosis is formed by the following arteries: inter-nal carotid, anterior communicating, posterior communicating, and basilar. The cerebral arteries extend from the circle of Willis into the brain.
QUESTION: Why do so many vessels contribute to the circle of Willis?
even during sleep, and must have a constant flow of blood to supply oxygen and remove waste products. For this reason there are four vessels that bring blood to the circle of Willis. From this anastomosis, several paired arteries (the cerebral arteries) extend into the brain itself.
The thoracic aorta and its branches supply the chest wall and the organs within the thoracic cavity. These vessels are listed in Table 13–1.
The abdominal aorta gives rise to arteries that sup- ply the abdominal wall and organs and to the common iliac arteries, which continue into the legs. Notice in Fig. 13–3 that the common iliac artery becomes the external iliac artery, which becomes the femoral artery, which becomes the popliteal artery; the same vessel has different names based on location. These vessels are also listed in Table 13–1.
The systemic veins drain blood from organs or parts of the body and often parallel their corresponding arteries. The most important veins are dia-grammed in Fig. 13–4 and listed in Table 13–2.
HEPATIC PORTAL CIRCULATION
Hepatic portal circulation is a subdivision of sys-temic circulation in which blood from the abdominal digestive organs and spleen circulates through the liver before returning to the heart.
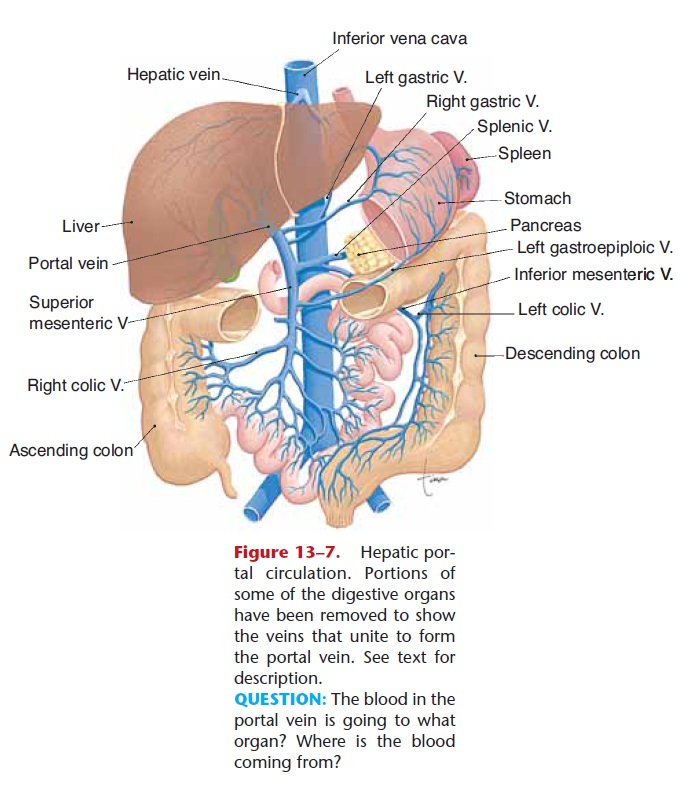
Figure 13–7. Hepatic por-tal circulation. Portions of some of the digestive organs have been removed to show the veins that unite to form the portal vein. See text for description.
Blood from the capillaries of the stomach, small intestine, colon, pancreas, and spleen flows into two large veins, the superior mesenteric vein and the splenic vein, which unite to form the portal vein (Fig. 13–7). The portal vein takes blood into the liver, where it branches extensively and empties blood into the sinusoids, the capillaries of the liver (see also Fig. 16–6). From the sinusoids, blood flows into hepatic veins, to the inferior vena cava and back to the right atrium. Notice that in this pathway there are two sets of capillaries, and keep in mind that it is in capillaries that exchanges take place. Let us use some specific examples to show the purpose and importance of por-tal circulation.
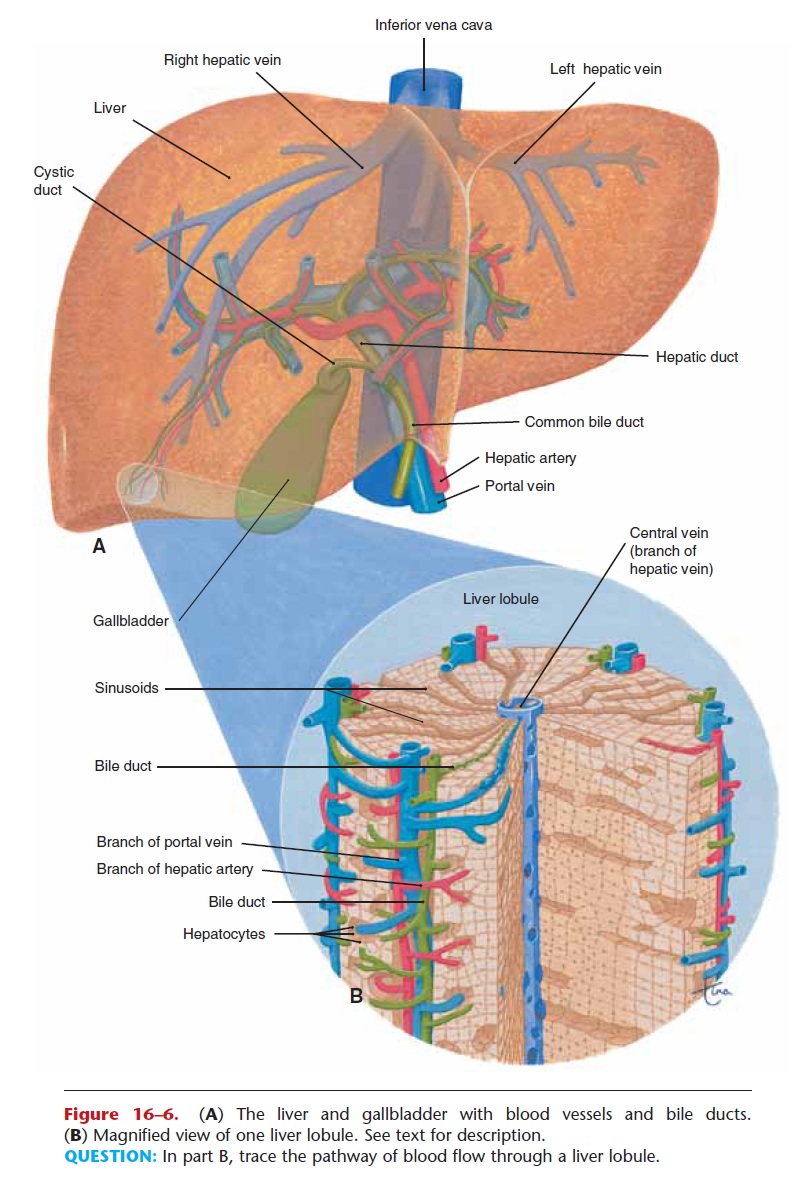
Glucose from carbohydrate digestion is absorbed into the capillaries of the small intestine; after a big meal this may greatly increase the blood glucose level. If this blood were to go directly back to the heart and then circulate through the kidneys, some of the glu-cose might be lost in urine. However, blood from the small intestine passes first through the liver sinusoids, and the liver cells remove the excess glucose and store it as glycogen. The blood that returns to the heart will then have a blood glucose level in the normal range.
Another example: Alcohol is absorbed into the cap-illaries of the stomach. If it were to circulate directly throughout the body, the alcohol would rapidly impair the functioning of the brain. Portal circulation, how-ever, takes blood from the stomach to the liver, the organ that can detoxify the alcohol and prevent its detrimental effects on the brain. Of course, if alcohol consumption continues, the blood alcohol level rises faster than the liver’s capacity to detoxify, and the well-known signs of alcohol intoxication appear.
As you can see, this portal circulation pathway enables the liver to modify the blood from the diges-tive organs and spleen. Some nutrients may be stored or changed, bilirubin from the spleen is excreted into bile, and potential poisons are detoxified before the blood returns to the heart and the rest of the body.
FETAL CIRCULATION
The fetus depends upon the mother for oxygen and nutrients and for the removal of carbon dioxide and other waste products.
The site of exchange between fetus and mother is the placenta, which contains fetal and maternal blood vessels that are very close to one another (see Figs. 13–8 and 21–5). The blood of the fetus does not mix with the blood of the mother; sub-stances are exchanged by diffusion and active trans-port mechanisms.
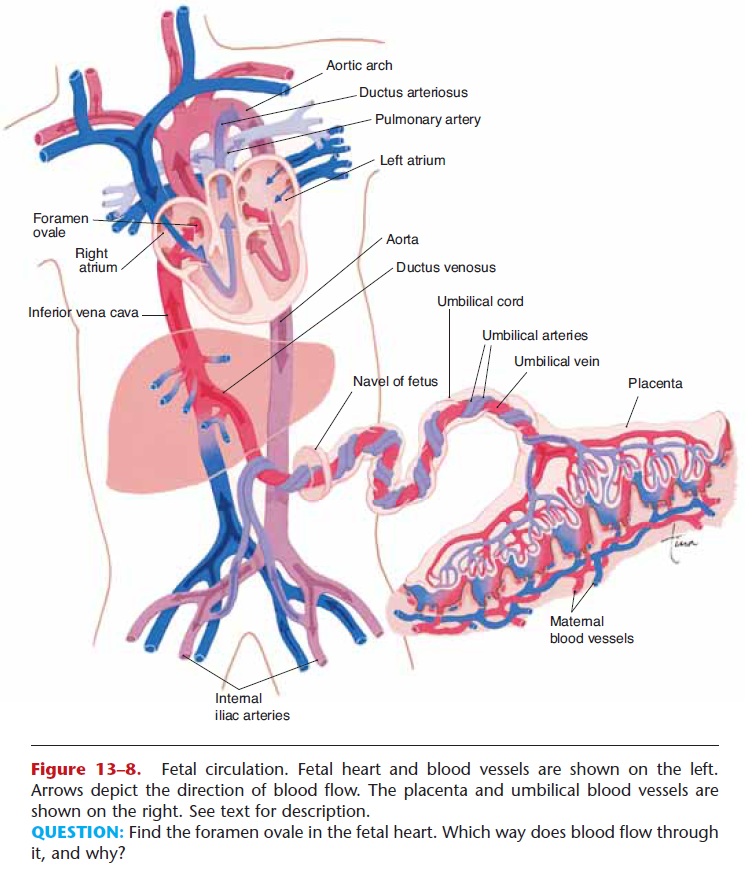
Figure 13–8. Fetal circulation. Fetal heart and blood vessels are shown on the left. Arrows depict the direction of blood flow. The placenta and umbilical blood vessels are shown on the right. See text for description.
QUESTION: Find the foramen ovale in the fetal heart. Which way does blood flow through it, and why?
The fetus is connected to the placenta by the umbilical cord, which contains two umbilical arteries and one umbilical vein (see Fig. 13–8). The umbilical arteries are branches of the fetal internal iliac arteries; they carry blood from the fetus to the placenta. In the placenta, carbon
dioxide and waste products in the fetal blood enter maternal circulation, and oxygen and nutrients from the mother’s blood enter fetal circulation.
The umbilical vein carries this oxygenated blood from the placenta to the fetus. Within the body of the fetus, the umbilical vein branches: One branch takes some blood to the fetal liver, but most of the blood passes through the ductus venosus to the inferior vena cava, to the right atrium. After birth, when the umbilical cord is cut, the remnants of these fetal ves-sels constrict and become nonfunctional.
The other modifications of fetal circulation con-cern the fetal heart and large arteries (also shown in artery to the aorta, to the body. Both the foramen ovale and the ductus arteriosus permit blood to bypass the fetal lungs.
Just after birth, the baby breathes and expands its lungs, which pulls more blood into the pulmonary cir-culation. More blood then returns to the left atrium, and a flap on the left side of the foramen ovale is closed. The ductus arteriosus constricts, probably in response to the higher oxygen content of the blood, and pulmonary circulation becomes fully functional within a few days.
Related Topics