Chapter: Essentials of Anatomy and Physiology: The Vascular System
Blood Pressure
BLOOD PRESSURE
Blood pressure is the force the blood exerts against the walls of the blood vessels. Filtration in capillaries depends upon blood pressure; filtration brings nutri-ents to tissues, and as you will see, is the first step in the formation of urine. Blood pressure is one of the “vital signs” often measured, and indeed a normal blood pressure is essential to life.
The pumping of the ventricles creates blood pres-sure, which is measured in mmHg (millimeters of mercury). When a systemic blood pressure reading is taken, two numbers are obtained: systolic and dias-tolic, as in 110/70 mmHg. Systolic pressure is always the higher of the two and represents the blood pres-sure when the left ventricle is contracting. The lower number is the diastolic pressure, when the left ventri-cle is relaxed and does not exert force. Diastolic pres-sure is maintained by the arteries and arterioles and is discussed in a later section.
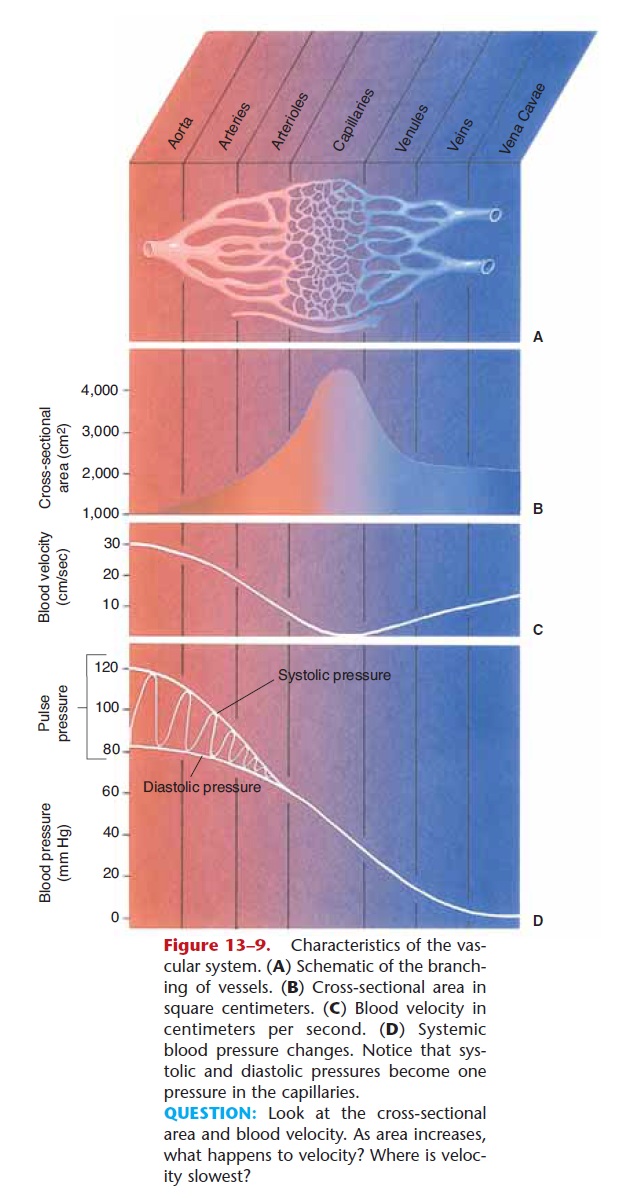
Systemic blood pressure is highest in the aorta, which receives all of the blood pumped by the left ven tricle. As blood travels farther away from the heart, blood pressure decreases (see Fig. 13–9). The brachial artery is most often used to take a blood pressure read-ing; here a normal systolic range is 90 to 120 mmHg, and a normal diastolic range is 60 to 80 mmHg. In the arterioles, blood pressure decreases further, and sys-tolic and diastolic pressures merge into one pressure. At the arterial end of capillary networks, blood pres-sure is about 30 to 35 mmHg, decreasing to 12 to 15 mmHg at the venous end of capillaries. This is high enough to permit filtration but low enough to prevent rupture of the capillaries. As blood flows through veins, the pressure decreases further, and in the caval veins, blood pressure approaches zero as blood enters the right atrium.
The upper limit of the normal blood pressure range is now 120/80 mmHg. The levels of 125 to 139/85 to 89 mmHg, once considered high-normal, are now called “prehypertension,” that is, with the potential to become even higher. A systemic blood pressure con-sistently higher than the normal range is called hyper-tension. A lower than normal blood pressure is called hypotension. The regulation of systemic blood pressure is discussed in a later section.
Pulmonary blood pressure is created by the right ventricle, which has relatively thin walls and thus exerts about one-sixth the force of the left ventricle. The result is that pulmonary arterial pressure is always low: 20 to 25/8 to 10 mmHg, and in pulmonary capillaries is lower still. This is important to prevent filtration in pulmonary capillaries, which in turn prevents tissue fluid from accumulating in the alveoli of the lungs.
MAINTENANCE OF SYSTEMIC BLOOD PRESSURE
Because blood pressure is so important, many physio-logical factors and processes interact to keep blood pressure within normal limits:
1. Venous return—the amount of blood that returns to the heart by way of the veins. Venous return is important because the heart can pump only the blood it receives. If venous return decreases, the cardiac muscle fibers will not be stretched, the force of ventricular systole will decrease (Starling’s law), and blood pressure will decrease. This is what might happen following a severe hemorrhage.
When the body is horizontal, venous return can be maintained fairly easily, but when the body is vertical, gravity must be overcome to return blood from the lower body to the heart. Three mecha-nisms help promote venous return: constriction of veins, the skeletal muscle pump, and the respira-tory pump.
Veins contain smooth muscle, which enables them to constrict and force blood toward the heart; the valves prevent backflow of blood. The second mechanism is the skeletal muscle pump, which is especially effective for the deep veins of the legs. These veins are surrounded by skeletal muscles that contract and relax during normal activities such as walking. Contractions of the leg muscles squeeze the veins to force blood toward the heart. The third mechanism is the respiratory pump, which affects veins that pass through the chest cav-ity. The pressure changes of inhalation and exhala-tion alternately expand and compress the veins, and blood is returned to the heart.
2. Heart rate and force—in general, if heart rate and force increase, blood pressure increases; this is what happens during exercise. However, if the heart is beating extremely rapidly, the ventricles may not fill completely between beats, and cardiac output and blood pressure will decrease.
3. Peripheral resistance—this term refers to the resistance the vessels offer to the flow of blood. The arteries and veins are usually slightly con-stricted, which maintains normal diastolic blood pressure. It may be helpful to think of the vessels as the “container” for the blood. If a person’s body has 5 liters of blood, the “container” must be smaller in order for the blood to exert a pressure against its walls. This is what normal vasoconstric-tion does: It makes the container (the vessels) smaller than the volume of blood so that the blood will exert pressure even when the left ventricle is relaxed.
If more vasoconstriction occurs, blood pressure will increase (the container has become even smaller). This is what happens in a stress situation, when greater vasoconstriction is brought about by sympathetic impulses. If vasodilation occurs, blood pressure will decrease (the container is larger). After eating a large meal, for example, there is extensive vasodilation in the digestive tract to supply more oxygenated blood for digestive activi-ties. To keep blood pressure within the normal range, vasoconstriction must, and does, occur else-where in the body. This is why strenuous exercise should be avoided right after eating; there is not enough blood to completely supply oxygen to exer-cising muscles and an active digestive tract at the same time.
4. Elasticity of the large arteries—when the left ventricle contracts, the blood that enters the large arteries stretches their walls. The arterial walls are elastic and absorb some of the force. When the left ventricle relaxes, the arterial walls recoil or snap back, which helps keep diastolic pressure within the normal range. Normal elasticity, therefore, lowers systolic pressure, raises diastolic pressure, and maintains a normal pulse pressure. (Pulse pres-sure is the difference between systolic and diastolic pressure. The usual ratio of systolic to diastolic to pulse pressure is approximately 3:2:1. For example, with a blood pressure of 120/80 mmHg, the pulse pressure is 40, and the ratio is 120:80:40, or 3:2:1.)
5. Viscosity of the blood—normal blood viscosity depends upon the presence of red blood cells and plasma proteins, especially albumin. Having too many red blood cells is rare but does occur in the disorder called polycythemia vera and in people who are heavy smokers. This will increase blood viscosity and blood pressure.
A decreased number of red blood cells, as is seen with severe anemia, or decreased albumin, as may occur in liver disease or kidney disease, will decrease blood viscosity and blood pressure. In these situations, other mechanisms such as vaso-constriction will maintain blood pressure as close to normal as is possible.
6. Loss of blood—a small loss of blood, as when donating a pint of blood, will cause a temporary drop in blood pressure followed by rapid compen-sation in the form of a more rapid heart rate and greater vasoconstriction. After a severe hemor-rhage, however, these compensating mechanisms may not be sufficient to maintain normal blood pressure and blood flow to the brain. Although a person may survive loss of 50% of the body’s total blood, the possibility of brain damage increases as more blood is lost and not rapidly replaced.
7. Hormones—several hormones have effects on blood pressure. You may recall, but we will summarize them here and in Fig. 13–10. The adrenal medulla secretes norepi-nephrine and epinephrine in stress situations. Norepinephrine stimulates vasoconstriction, which raises blood pressure. Epinephrine also causes vaso-constriction, and increases heart rate and force of contraction, both of which increase blood pressure.
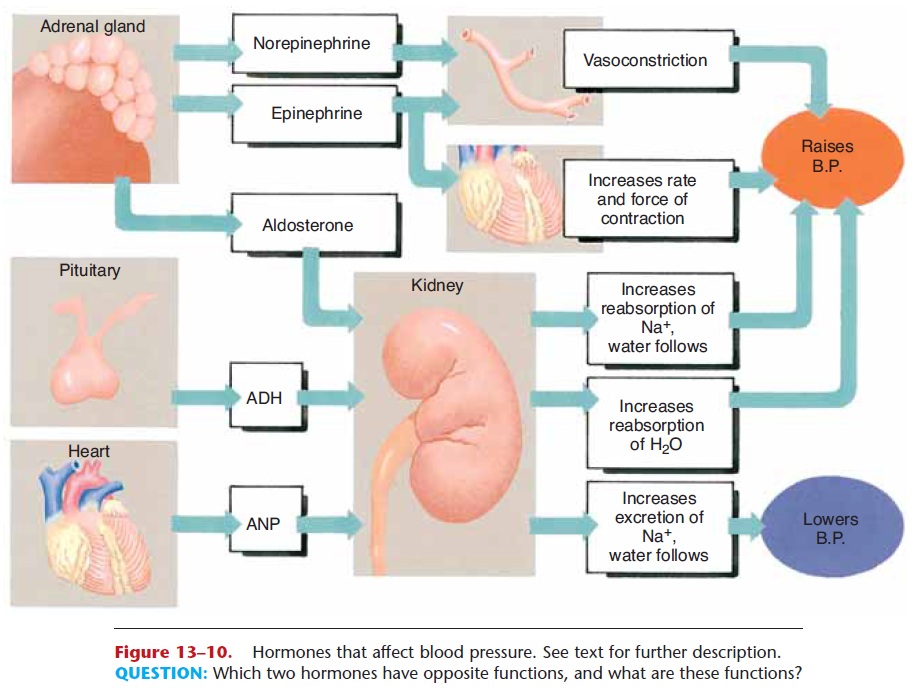
Figure 13–10. Hormones that affect blood pressure. See text for further description.
QUESTION: Which two hormones have opposite functions, and what are these functions?
Antidiuretic hormone (ADH) is secreted by the posterior pituitary gland when the water content of the body decreases. ADH increases the reabsorp-tion of water by the kidneys to prevent further loss of water in urine and a further decrease in blood pressure.
Aldosterone, a hormone from the adrenal cor-tex, has a similar effect on blood volume. When blood pressure decreases, secretion of aldosterone stimulates the reabsorption of Na+ ions by the kid-neys. Water follows sodium back to the blood, which maintains blood volume to prevent a further drop in blood pressure.
Atrial natriuretic peptide (ANP), secreted by the atria of the heart, functions in opposition to aldos-terone. ANP increases the excretion of Na+ ions and water by the kidneys, which decreases blood volume and lowers blood pressure.
DISTRIBUTION OF BLOOD FLOW
An individual’s blood volume remains relatively con-stant within the normal range appropriate to the size of the person. Active tissues, however, require more blood, that is, more oxygen, than do less active tissues. As active tissues and organs receive a greater propor-tion of the total blood flow, less active organs must receive less, or blood pressure will decrease markedly.
As mentioned previously, precapillary sphincters dilate in active tissues and constrict in less active ones. The arterioles also constrict to reduce blood flow to less active organs. This ensures that metabolically active organs will receive enough oxygen to function properly and that blood pressure for the body as a whole will be maintained within normal limits.
An example will be helpful here; let us use the body at rest and the body during exercise. Consult Fig. 13–11 as you read the following. Resting cardiac output is approximately 5000 mL per minute. Exercise cardiac output is three times that, about 15,000 mL per minute. Keep in mind that the volume of blood is the same in both cases, but that during exercise the blood is being circulated more rapidly.
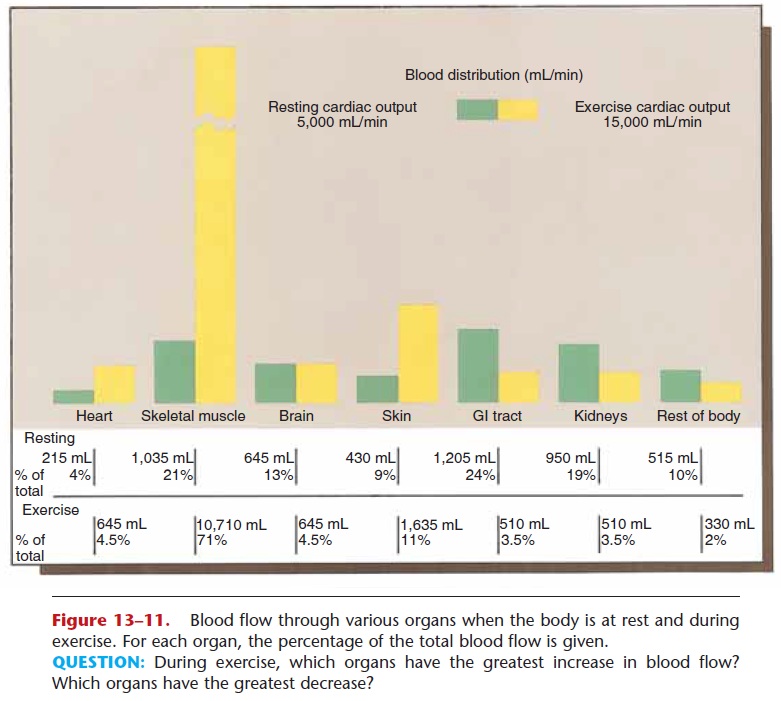
Compare the amounts of blood flowing to various organs and tissues during exercise and at rest. During exercise, the heart receives about three times as much blood as it does when the body is at rest. The very active skeletal muscles receive about ten times as much blood. The skin, as an organ of heat loss, receives about four times as much blood. Other organs, how-ever, can function adequately with less blood. Blood flow is reduced to the digestive tract, to the kidneys, and to other parts of the body such as bones.
When the exercise ceases, cardiac output will gradually return to the resting level, as will blood flow to the various organs. These changes in the distribu- tion of blood ensure sufficient oxygen for active tissues and an appropriate blood pressure for the body as a whole.
Related Topics