Chapter: Paediatrics: Neurology
Paediatrics: Neuromuscular disorders
Neuromuscular disorders
See also the floppy infant. In
children with neuromuscular problems, first think about the anatomical site
that is affected (Fig. 14.7).
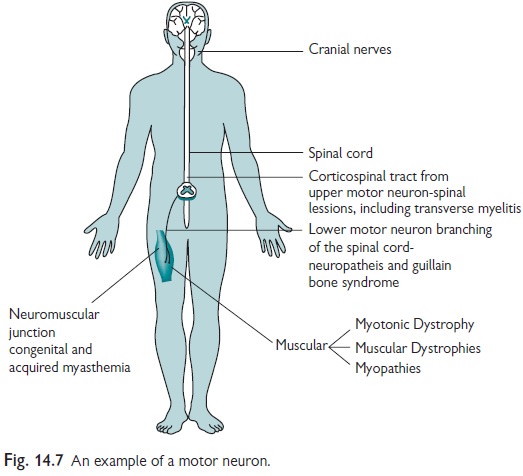
┬Ę Brain.
┬Ę Spine.
┬Ę Anterior horn cell.
┬Ę Peripheral nerve.
┬Ę Neuromuscular junction.
┬Ę Muscle.
Cerebral insult
Any brain insult may make a child
unreactive and move less. In these child-ren there may be obvious signs of
cerebral dysfunction such as enceph-alopathy. Facial movement and peripheral
power are good if the child is able to follow commands. However, they may have
low tone in the trunk, with relatively better tone at limb extremities. Good
examples are Down or Prader-Willi syndromes. Reflexes should be present. If
there is damage to the upper motor neuron then there will be spasticity with
increased tone and brisk reflexes, e.g. cerebral palsy.
Spinal cord lesions
Spinal tumours and transverse
myelitis should produce a rough level, beneath which there will be upper motor
neuron signs or a sensory level or both. Spinal cord tumours are normally
associated with a number of signs including constipation and urinary symptoms.
There are particular signs which should always be investigated.
When to worry about a spinal cord lesion
┬Ę Neurological signs, particularly
when objective, e.g. hypereflexia and paresis, at a level beneath C1
┬Ę Back pain with no other signs in
children under 11yrs
┬Ę Change in urinary function or
bowel habit with back pain in older children
Transverse myelitis
Quick onset (i.e. in days and
sometimes hours) of weakness, and/or anaes-thesia, and/or urinary dysfunction,
and/or bowel disturbance, often within a week of a minor viral infection. It
may be associated with back pain. Although later on there will be upper motor
neuron signs, where there is an acute presentation, there may be reduced
reflexes and power for the first days. However, where the weakness continues
there will be a gradual increase in the reflexes and tone. Urgent imaging of
the cord by spinal MRI with gadolinium required to exclude cord compression, and in
many cases will confirm appearances of myelitis.
Management
┬ĘImmediate
admission for monitoring of
respiratory status. Review for urinary and GI disturbance. Feeding/swallowing assessment.
┬ĘEarly introduction of
physiotherapy and occupational therapy to avoid joint contracture.
┬ĘControl of pain.
Methylprednisolone:
IV treatment (30mg/kg, given over
a period of at least 30min for 3
days) normally used initially, if no response consider other immune-modulatory
therapy.
Anterior horn cell disorders
Disorder here produces flaccid, areflexic limb, normally sparing the face.
Polio
┬Ę Now rare. May still be seen
following vaccination, or in immigrants.
┬Ę Long-term, the limb becomes
flaccid and wasted.
Spinal muscular atrophies
Confirmation of these conditions
includes fibrillation on EMG and homozygous deletion of survival motor neuron
(SMN) gene.
┬Ę Type
0 (neonatal form): very
severe, often with arthrogryposis.
┬Ę Type
1 (WerdnigŌĆōHoffman): severe
with onset in the first months of
life. Typically, there are ŌĆśbright eyesŌĆÖ, severe hypotonia, ŌĆśfrog-like
postureŌĆÖ, areflexia, and weakness that is present more in the legs than arms.
Normally fatal by 2yrs of age.
┬Ę Type
2: onset in the first years of life
with low tone, peripheral weakness,
absent reflexes, and scoliosis.
┬Ę Type
3: adolescent onset with progressive
weakness and gait disturbance, loss
of reflexes, and low tone.
These disorders will have similar
DNA results, so do not make a prognosis on the basis of the DNA result. They
are very complicated, and will need to be reviewed by specialists, with
reference to:
┬Ę An accurate prognosis based on
clinical assessment.
┬Ę Advice on appropriate therapies
e.g. invasive ventilation for type 1.
Multidisciplinary support for
occupational, physio and speech therapies, as well as dietary, respiratory,
neurological, psychological and social support.
Related Topics