Chapter: Paediatrics: Neurology
Paediatrics: Cerebral palsy
Cerebral palsy
┬Ę Definition:
a chronic disorder of movement
and/or posture that presents early
(i.e. before the age of 2yrs) and continues throughout life.
┬Ę Causation:
CP is caused by static injury to
the developing brain.
┬Ę Associations:
children with CP are at increased
risk of impairments including vision,
hearing, speech, learning, epilepsy, nutrition, and psychiatric.
┬Ę Clinical
forms: most children will
have a mixed disorder, but some can have pure
components of spasticitiy, choreoathatosis, or very rarely ataxia.
Spastic CP
This is the commonest label and
children can be hemiplegic, diplegic, or quadriplegic. Monoplegic cerebral
palsy is extremely rare, and normal-ly a misdiagnosis as the clinician has not
examined the arm effectively. Spasticity is a stretch-related response
characterized by a velocity-depen-dent, increased resistance to passive
stretch. It is caused by disruption to the spinal reflex arc by the upper motor
neuron. It will affect all the skeletal muscles and causes the following:
┬Ę Increased tone and reflexes.
┬Ę Clasp knife phenomenon on rapidly
stretching tendons often described as a ŌĆścatchŌĆÖ.
┬Ę Leg:
ankle plantar flexion, and either
valgus or varus deformity of foot.
┬Ę Hip:
flexion, limited adduction, and
often internal rotation.
┬Ę Wrist:
flexed and pronated.
┬Ę Elbow:
flexed.
┬Ę Shoulder:
adducted.
┬Ę Bulbar muscles may be spastic
giving dysphagia and dribbling.
Choreoathetosis
Condition presents as a 4-limb
disorder with greatly increased tone while awake and less so during the early
stages of sleep. These patients do not have the stretch-related response and
increased reflexes of pure spastic CP. However, there may be combinations of
these features in mixed CP. As the child matures they will often develop fixed
reduction in joint range of movement and then the signs will be more difficult
to distinguish from those of spastic CP. They almost always have bulbar
problems.
Ataxic cerebral palsy
This form of CP is extremely rare
and poorly understood. It is also known as the disequilibrium syndrome.
Children have a congenital ataxia giving them a striking loss of balance in the
early years (i.e. disequilibrium). They often have a mild diplegia and are
thought to be aetiologically distinct from the other types of CP, where hypoxia
and ischaemia are thought to be causal factors. It may be that congenital
ataxia is a better than applying cerebral palsyŌĆösee Investigation of CP.
Investigation of CP
┬Ę CP is a descriptive term of
disability and not the cause.
The key factor is a static
neurological insult.
┬ĘMay well be given in the history.
Beware associations being used to explain CP; factors such as prematurity may
lead to complications, but the child needs a comprehensive assessment to
exclude other disordersŌĆöesp. progressive ones. All children need investigation.
┬ĘHistory:
the cause may be evident from a
good history, in particular for prematurity
and periods of hypoxic ischaemia.
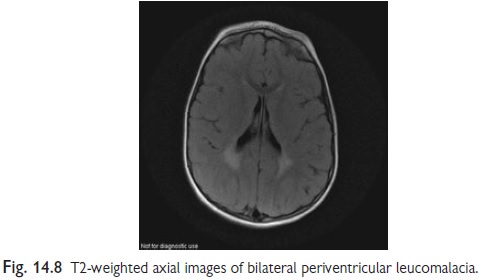
Imaging:
MRI scan of the brain, with
particular reference to the pyramidal tracts
in children with spasticity and the basal ganglia in others (Fig. 14.8). If
there is a problem in the history, e.g. hypoxic ischaemic encephalopathy, then
there should be signs of this on the imaging. Where imaging does not confirm a
static insult, seek expert opinion.
Management of CP
┬ĘComplex
multidisciplinary input.:
the primary therapists are the childŌĆÖs carers
as they will provide at least 90% of the therapy to the child. In the early
years, experts in speech, physiotherapy, and occupational therapy will support
this treatment.
┬ĘPosture
and movement: optimize
function by improving symmetry, joint ranges,
muscle length and power. Treatments and support include stretching exercises,
orthoses (e.g. ankle foot orthosis), wheelchair for mobility, sleeping and
standing systems, and botulinum toxin (Botox) to the gastrocnemius. Surgery is
used as a last resort.
┬ĘCommunication:
with speech therapy and aids.
┬ĘIndependence with a tailored
educational program, aids under supervision from occupational therapy.
┬ĘCognition
and learning support: with
a tailored educational programme.
┬ĘGeneral
medical: watch for
seizures, constipation, malnutrition, and
behavioural or psychiatric disturbance.
Note:
Dopamine-responsive dystonia will
very rarely present with an unexplained
diplegia and normal MRI. All these children will need a trial of co-careldopa
with a gradually increasing dose of up to 10mg/kg/day of the dopa component
over 3mths. If there is not a significant improve-ment then the child is
unlikely to be dopa-sensitive.
Related Topics