Chapter: Paediatrics: Paediatric Surgery
Paediatrics: Intussusception
Intussusception
Intussusception typically affects
infants between 6 and 18mths of age. The incidence is 1/500 children. The
majority of intussusceptions occur in association with viral gastroenteritis.
ŌĆó
Enlarged
PeyerŌĆÖs patch in the ileum acts as the lead
point that then invaginates into the distal bowel.
ŌĆó
Intussusceptions
in older children and adults are more likely to be due to a pathological lead point, e.g. a polyp or
MeckelŌĆÖs diverticulum.
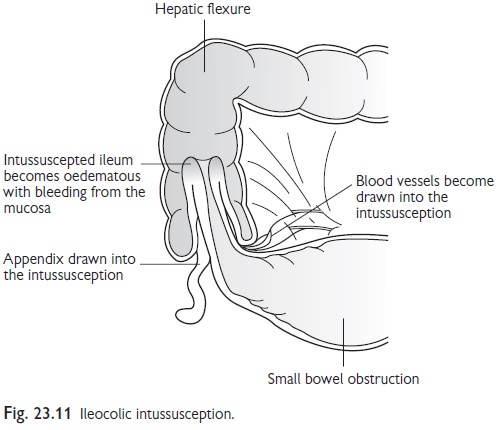
Intussusception causes a small
bowel obstruction. The intussuscepted bowel becomes engorged, which causes
rectal bleeding, and eventually gangrenous. Following this, perforation and
peritonitis will occur. The most common site for an intussusception is
ileocolic (Fig. 23.11) followed by ileo-ileal. Small bowel intussusception may
occur as a post-operative complication in infants, typically following
nephrectomy.
Presentation
The typical presentation of an
intussusception in an infant is as follows:
ŌĆó
Spasms
of colic associated with pallor, screaming, and drawing-up legs.
ŌĆó
The
child falls asleep between episodes.
ŌĆó
Later,
as the intestinal obstruction progresses, bile-stained vomiting develops and
rectal bleeding, (i.e. ŌĆśred currant jelly stoolsŌĆÖ).
ŌĆó
The
child will appear ill, listless, and dehydrated.
ŌĆó
In
late cases circulatory shock or peritonitis will be present.
Assessment
┬Ę In 30% of cases the
intussusception will be palpable as a sausage-shaped abdominal mass.
ŌĆó
Blood
may be noted on rectal examination.
ŌĆó
AXR: small bowel obstruction and
occasionally a soft tissue mass will be
visible.
ŌĆó
US: confirms the diagnosis by showing
a characteristic ŌĆśtarget signŌĆÖ.
Management
┬Ę Resuscitation:
often large volumes of IV fluid
are required to restore perfusion.
┬Ę Antibiotics.
ŌĆó
Analgesia.
ŌĆó
NGT passed if the infant is vomiting.
ŌĆó
Radiological reduction: provided that there is no evidence
of peritonitis, and facilities for immediate surgery are available, the treatment
of choice is for an expert paediatric radiologist to reduce the intussusception
pneumatically by rectal insufflation of air under fluoroscopic control. The
risks of this procedure are incomplete reduction and perforation. The latter
can be particularly dangerous as a tension pneumoperitoneum develops very
rapidly.
ŌĆó Laparotomy: if pneumatic reduction fails, or is contraindicated because of concern about a gangrenous intussusception, laparotomy is necessary. The distal bowel is gently compressed to reduce the intussusception. If this is not successful then the intussusception is resected. There is a recurrence rate about 10% whether the intussusception is treated radiologically or by surgery. Further recurrence should raise the question of a pathological lead point.
Related Topics