Chapter: Paediatrics: Paediatric Surgery
Paediatrics: Idiopathic hypertrophic pyloric stenosis
Idiopathic hypertrophic pyloric stenosis
The incidence of idiopathic
hypertrophic pyloric stenosis (IHPS) is 73/1000 live births. Boys are affected
more frequently than girls and IHPS is more common in Whites than in
dark-skinned races. The pylorus enlarges as a result of hypertrophy of the
circular muscle to produce the typical ŌĆśtumourŌĆÖ. The cause remains unknown.
Familial occurrence is well docu-mented, particularly in girls.
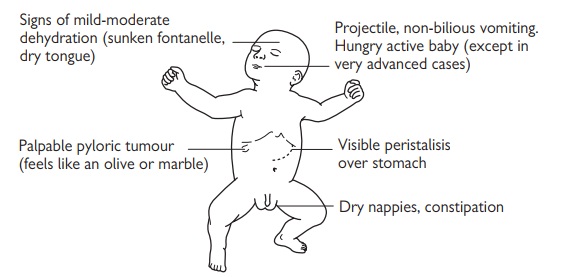
Clinical features (Fig. 23.6)
ŌĆó
Vomiting: projectile, starting in the third
or fourth week of life. The vomitus
is always non-bilious, but it may contain altered blood (ŌĆścoffee groundŌĆÖ) or fresh
blood from oesophagitis. Vomiting occurs within an hour of feeding and the baby
is immediately hungry. Vomiting may not be projectile in babies who present
early (first or second week); they are often misdiagnosed as suffering from
GOR.
ŌĆó
Constipation is common due to reduced fluid
intake.
ŌĆó
Dehydration, malnutrition, and jaundice are
late signs.
ŌĆó
IHPS
is rare beyond 12wks of age.
Diagnosis
ŌĆó
Test feed: the baby is allowed to feed from
the breast or bottle whilst the
examiner palpates the babyŌĆÖs abdomen. This is best conducted with the baby
resting on the motherŌĆÖs lap, cradled on her left arm. The examiner sits
opposite the mother, on the babyŌĆÖs left. Visible waves of gastric peristalsis
may be seen passing across the upper abdomen. The pyloric tumour is usually
easiest to feel either early in the feed or after the baby has vomited. 60ŌĆō90%
tumours are palpable. The thickened pylorus is palpable as a firm,
ŌĆśolive-shapedŌĆÖ mass, just above and to the right of the umbilicus during a
ŌĆśtest feedŌĆÖ.
ŌĆó
US: if a tumour cannot be felt, US
will usually confirm or exclude the diagnosis.
ŌĆó
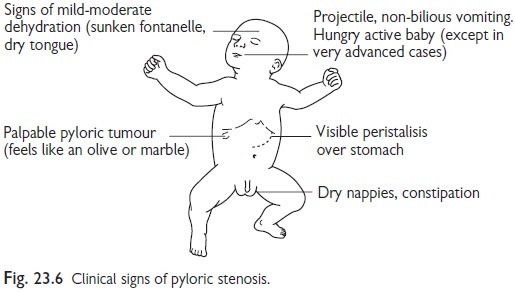
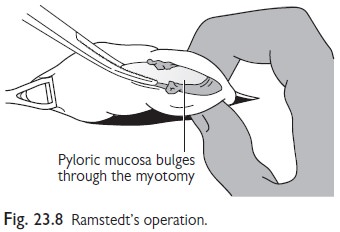
Biochemistry: the biochemical abnormality of
IHPS is a hypochloraemic, hypokalaemic
metabolic alkalosis (Fig. 23.7). Assess degree of alkalosis at presentation and
monitor correction prior to surgery.
Pre-operative management
ŌĆó
Rehydrate and correct the
alkalosis before surgery.
ŌĆó
IV fluids should be started. 0.45% Saline
with 5% dextrose and 20mmol/L
potassium chloride at 120mL/kg/day.
ŌĆó
Feeds: withhold. The stomach should be
emptied with a NGT.
ŌĆó
Electrolytes and capillary blood
pH: should be checked regularly until they return to normal (usually 24ŌĆō48h).
ŌĆó
Blood glucose: should be monitored.
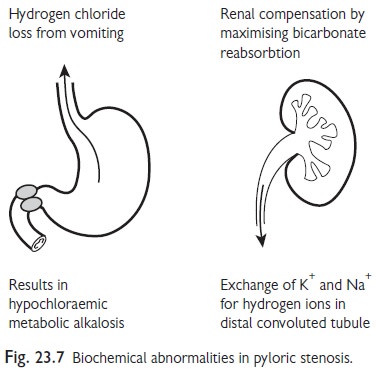
Surgery
ŌĆó
RamstedtŌĆÖs pyloromyotomy: the treatment of choice (Fig.
23.8). This involves splitting the
thickened pyloric muscle. Complications include
perforation of the mucosa, which is not serious provided it is recognized and
repaired, and wound infection.
ŌĆó
Oral feeds are usually withheld overnight.
Transient post-operative vomiting is
common but invariably settles within 36h. There are no long-term sequelae.
Related Topics