Chapter: Clinical Cases in Anesthesia : Spinal Anesthesia
Outline the advantages and disadvantages of catheter (continuous) spinal anesthesia
Outline the advantages and disadvantages of catheter (continuous)
spinal anesthesia.
In one form or another, catheter spinal
anesthesia tech-niques have provided excellent anesthesia for approximately 100
years. They offer all the benefits of single-injection spinal anesthesia plus
limitless duration of action. Continuous spinal anesthesia lapsed into disuse
with the advent of continuous epidural anesthesia, which offered relief from
the high incidence of PDPH. The relatively recent development of smaller
catheters designed for use in the subarachnoid space has led to renewed
interest in catheter spinal anesthesia. It may be selected over
single-injection spinal anesthesia for basically two reasons. Catheter spinal
anesthesia offers the option for slow incremental dosing intended to minimize
hemodynamic changes. It also extends the duration of anesthesia for operations
expected to outlast the course of single-dose methods.
Advances in technology and pharmacology have
brought us to the present state of the art. In the past, catheter spinal
anesthesia was performed with large-bore needles and catheters designed for
epidural use. Presently there are catheters ranging in size from 24- to
32-gauge. These catheters are intended for insertion through 20- to 27-gauge
needles in an attempt to reduce the incidence of PDPH. Establishment of
continuous spinal anesthesia is usually simple. A needle is placed in the
subarachnoid space, and the difference from skin to the space is estimated by
subtracting the length of the exposed needle from the needle’s total length.
The catheter is passed through the needle until its tip resides at the needle
bevel. This is usually a distance of 10 cm. The catheter is then advanced 3 cm
into the subarach-noid space. Inability to thread the catheter beyond the
needle bevel generally results from obstruction by one of several anatomic
structures. Combinations of needle manipulation, such as rotation and/or
advancement and/or withdrawal, generally allow for passage into the space. If
these maneuvers fail, the procedure is repeated at another interspace.
With the catheter properly inserted into the
subarach-noid space, slowly withdraw the needle over the catheter with one hand
as the other hand applies slight pressure in the opposite direction. Recall the
distance from the skin to the space and add 3 cm, this being the length of the
catheter which should be inserted into the patient’s back. Gently aspirate CSF
through the catheter to confirm proper placement.
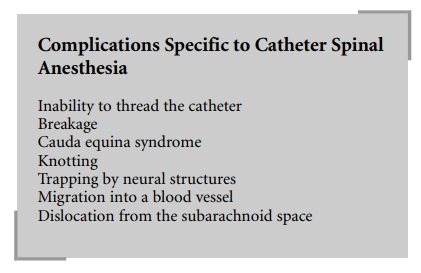
The recognized complications of continuous
spinal anesthesia include all those attributed to single-injection methods plus
those summarized below.
One of the most frequent and frustrating
complications of catheter techniques is the inability to pass a catheter into
the proper location. The incidence of inability to thread spinal catheters
approximates 8%. The potential causes of this problem are numerous and poorly
defined for any individual patient.
Experience with epidural catheters has shown
occasional breakage during insertion and removal. Spinal catheter breakage
during attempted insertion generally occurs when catheters are withdrawn
through the needle. An entire catheter segment may be sheared off by this
maneuver. Even a partial cut in the catheter could reduce its tensile strength,
predisposing to breakage during removal in the postoperative period. Inability
to pass a catheter must result in simultaneous removal of both needle and
catheter from the back. The procedure is then repeated at the same interspace
or another one.
Catheter breakage during removal from the back
is generally heralded by catheter elongation. Stretching can be considered a
warning sign of imminent danger. Break strengths of one presently available
24-gauge spinal catheter and a commonly used 20-gauge epidural catheter are
3.55 lb (1.6 kg) and 6.35 lb (2.9 kg), respectively. This is a very narrow
range, placing most catheters at risk of snapping during removal. Consequently,
removal must take place with the vertebrae flexed to the same degree as they
were during insertion. This maneuver attempts to realign the various ligaments,
minimizing their grip on the catheter.
Catheter breakage is a difficult problem to
deal with. If breakage occurs close to the skin, then superficial dissection
under local anesthesia may allow for isolation of the catheter. It can be
grasped with a clamp and gently removed. If the catheter is severed in deep
tissues, it may be left in situ. The risk of infection is small, because it is
placed under strictly sterile conditions. General anesthesia and laminectomy to
retrieve the catheter may place the patient at higher risk for associated
complications than leaving it in place. A moral and ethical obligation exists
to inform the patient of this compli-cation in the rare event of its occurrence.
Another theoretical problem is a small segment
of catheter floating freely within the subarachnoid space, which could migrate
cephalad and produce significant complica-tions. This situation may present a
more compelling reason for surgical removal than a catheter which is held
firmly by ligaments.
Another unusual but noteworthy complication of
catheter spinal anesthesia is cauda equina syndrome. In 1991, Rigler et al.
reported 4 cases of cauda equina syndrome occurring after catheter spinal
anesthesia. Evidence of sub-arachnoid block was achieved in all cases, and
additional doses were administered to raise the level of analgesia. The total
initial dose of local anesthetic was generally greater than that administered
in a single bolus dose through a spinal needle. The authors speculate that
pooling of large doses of local anesthetic resulted in neurotoxicity.
Later in 1991, Lambert and Hurley described a
model that demonstrated hyperbaric and isobaric lidocaine loculation in the
sacral and lower lumbar regions. In the event of inadequate local anesthetic
spread following injec-tion of 2% isobaric lidocaine (40 mg) they suggest the
addition of 1–2 mL of hypobaric 0.375% bupivacaine.
Hypobaric 0.375% bupivacaine is readily
prepared by dilu-tion of 0.75% plain bupivacaine with an equal volume of
distilled water. This technique should allow spread of local anesthetic into
the upper lumbar area while limiting local anesthetic exposure to only 40 mg of
lidocaine and 7.5 mg of bupivacaine. Such low doses of anesthetic would be
expected to place patients at low risk for cauda equina syndrome. This
combination of isobaric and hypobaric solutions is logical, based on observed
subarachnoid spread of these solutions.
Catheters can curl on themselves and tighten into
knots when withdrawn. Such occurrence could prevent with-drawal
postoperatively, because the knot would be too large to fit through the dural
hole. A worse circumstance could occur if a nerve were entrapped by the knot.
In this case, one would expect radicular pain during attempted catheter
removal. Catheter curling is most likely to happen if excessive lengths are
inserted into the subarachnoid space. To prevent this, never advance more than
3 cm of catheter beyond the needle tip.
Migration into a blood vessel is generally of
little conse-quence. The usual doses of local anesthetic delivered for spinal
anesthesia (approximately 50 mg of lidocaine) are less than those purposefully
administered intravenously for the treatment of premature ventricular contractions
(approximately 100 mg of lidocaine).
Dislocation from the subarachnoid space will
result in epidural placement. The small doses of local anesthetic generally
employed for spinal anesthesia will yield minimal or no blockade following
administration into the epidural space. It is theoretically possible, although
highly unlikely, that a catheter intended for the subarachnoid space could
lodge in the subdural space. The subsequent delivery of local anesthetic would
then cause either segmental anesthesia or massive sympathetic, sensory, and
motor blockade, depend-ing on the dose administered into the subdural space.
A century of spinal anesthesia has witnessed
advances in pharmacology and technology culminating in the use of small
catheters for placement in the subarachnoid space. Although spinal anesthesia,
like general anesthesia, is fraught with potential problems, its judicious
application has benefited innumerable patients. Continuous spinal anesthesia
represents a double-edged sword. It offers advantages over general anesthesia
and catheter epidural anesthesia but is associated with its own potential
compli-cations. With knowledge of these potential problems and careful
application of the procedure, catheter spinal anesthesia remains a safe and desirable
technique.
Related Topics