Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Rheumatic Disorders
Nursing Process: The Patient With a Rheumatic Disease
NURSING PROCESS:THE PATIENT WITHA RHEUMATIC DISEASE
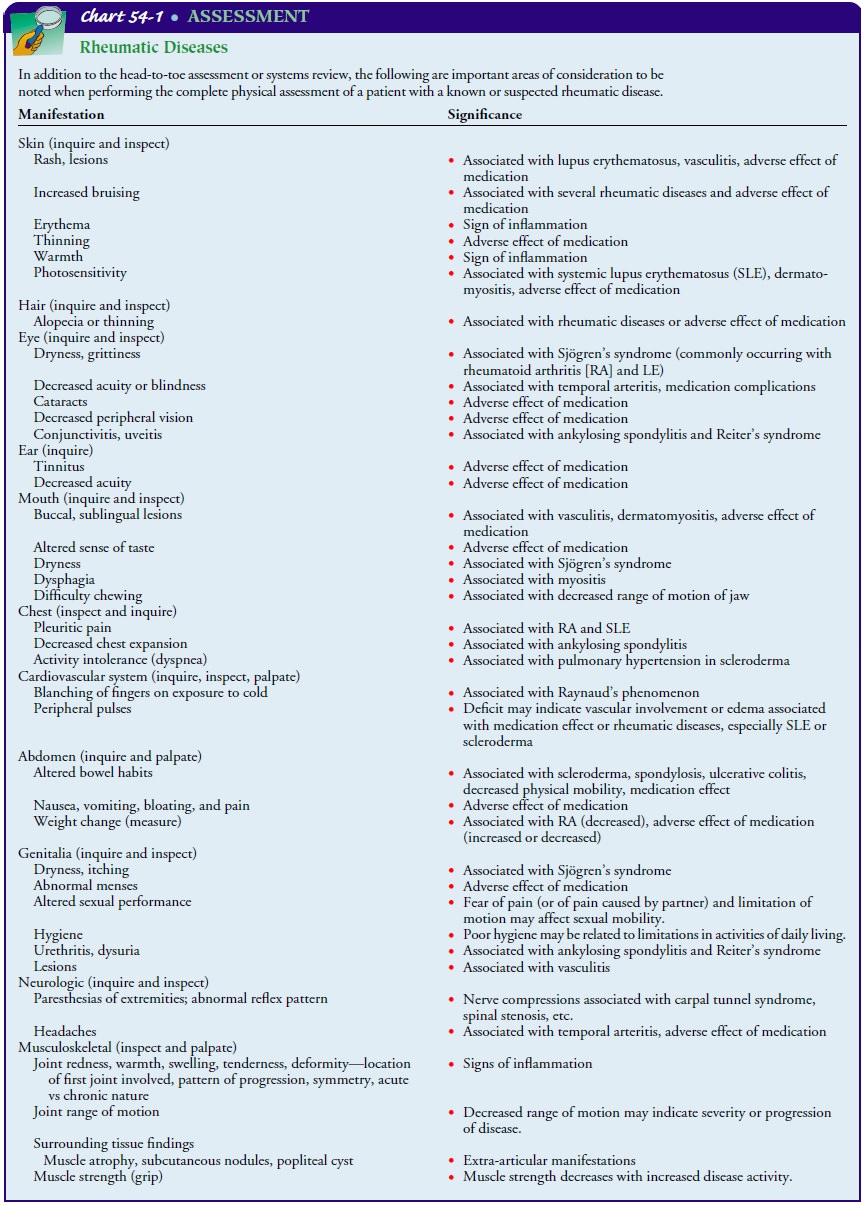
Assessment
The
depth and focus of the nursing assessment depend on several factors: the health
care setting (clinic or office, home, extended care facility, or hospital), the
role of the nurse (home care nurse; nurse practitioner; hospital, clinic, or
office nurse), and the needs of the patient. The nurse is often the first of
the health care team members to come in contact with the patient. This enables the
nurse to assess the patient’s perceptions of the disorder and situ-ation,
actions taken to relieve symptoms, plans for treatment, and expectations. The
nurse’s assessment may lead to identifying is-sues and concerns that can be
addressed by nursing interventions and, through collaboration with other team
members, to achieving the expected patient outcomes.
The health history and physical assessment focus on
current and past symptoms, such as fatigue, weakness, pain, stiffness, fever,
or anorexia, and the effects of these symptoms on the pa-tient’s lifestyle and
self-image. Because the rheumatic diseases affect many body systems, the
history and physical assessment include a review and examination of all
systems, with particular attention given to those areas most commonly affected,
includ-ing the musculoskeletal system (see Chart 54-1).
The patient’s psychological and mental status and social sup-port systems are also assessed, as is his or her ability to participate in daily activities, comply with the treatment regimen, and man-age self-care. The information obtained can give insight into the patient’s understanding of the medication regimen and may re-veal misuse of medications, noncompliance, or use of potentially harmful unproven remedies. Additional areas assessed include the patient’s understanding, motivation, knowledge, coping abilities, past experiences, preconceptions, and fears. The effects of the dis-ease on the patient’s self-concept and coping abilities are also as-sessed. The patient’s perception of the condition and its impact influences the decisions, choices, and actions associated with treat-ment recommendations.
Diagnosis
NURSING DIAGNOSES
Although
many nursing diagnoses are appropriate for the patient with a rheumatic
disease, a few of the most common include the following:
·
Acute and chronic pain related
to inflammation and in-creased disease activity, tissue damage, fatigue, or
lowered tolerance level
·
Fatigue related to increased
disease activity, pain, inadequate sleep/rest, deconditioning, inadequate
nutrition, emotional stress/depression
·
Disturbed sleep pattern
related to pain, depression, and medications
·
Impaired physical mobility
related to decreased range of motion, muscle weakness, pain on movement,
limited endurance, lack of or improper use of ambulatory devices
·
Self-care deficits related to
contractures, fatigue, or loss of motion
·
Disturbed body image related
to physical and psychological changes and dependency imposed by chronic illness
·
Ineffective coping related to
actual or perceived lifestyle or role changes
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on assessment data, potential complications may include the following:
Adverse
effects of medications
Planning and Goals
The
major goals for the patient may include relief of pain and dis-comfort, relief
of fatigue, increased mobility, maintenance of self-care, improved body image,
effective coping, and absence of complications.
Nursing Interventions
An
understanding of the underlying disease process (ie, degener-ation or
inflammation, including degeneration resulting from inflammation or vice versa)
guides the nurse’s critical thinking processes. In addition, knowledge about
whether the condition is localized or more widely systemic influences the scope
of the nursing activity.
Some rheumatic diseases (eg, OA) are more localized
alterations in which control of symptoms such as pain or stiffness is possible.
Others (eg, gout) have a known cause and specific treatment to control the
symptoms. The diseases that usually present the great-est challenge are those
with systemic manifestations, such as the dif-fuse connective tissue diseases.
The Plan of Nursing Care details the nursing interventions to be considered for
each nursing diagnosis.
RELIEVING PAIN AND DISCOMFORT
Medications are used on a short-term basis to
relieve acute pain. Because the pain may be persistent, nonopioid analgesics
such as acetaminophen are often used. After administering medications, the
nurse needs to reassess pain levels at intervals. With persistent pain,
assessment findings should be compared with baseline mea-surements and
evaluations. Additional measures include explor-ing coping skills and strategies
that have worked in the past.
The
patient needs to understand the importance of taking medications, such as
NSAIDs and disease-modifying agents, ex-actly as prescribed to achieve maximum
benefits. These benefits include relief of pain and anti-inflammatory action as
the disease is brought under control. Because disease control and pain relief
are delayed, the patient may mistakenly believe the medication is ineffective
or may think of the medication as merely “pain pills,” taking them only
sporadically and failing to achieve control over the disease activity.
Alternately, the patient may not understand the need to continue the medication
for its anti-inflammatory actions once pain control has been achieved.
A
weight reduction program may be recommended to relieve stress on painful
joints. Heat applications are also helpful in re-lieving pain, stiffness, and
muscle spasm. Superficial heat may be applied in the form of warm tub baths or
showers and warm moist compresses. Paraffin baths (dips), which offer
concentrated heat, are helpful to patients with wrist and small-joint
involve-ment. Maximum benefit is achieved within 20 minutes of appli-cation.
More frequent use for shorter lengths of time is most beneficial. Therapeutic
exercises can be carried out more com-fortably and effectively after heat has
been applied.
In some patients, however, heat may actually
increase pain, mus-cle spasm, and synovial fluid volume. If the inflammatory
process is acute, cold applications in the form of moist packs or an ice bag
may be tried. Both heat and cold are analgesic to nerve pain receptors and can
relax muscle spasms. Safe use of heat and cold must be eval-uated and taught,
particularly to patients with impaired sensation.
The
use of braces, splints, and assistive devices for ambulation, such as canes,
crutches, and walkers, eases pain by limiting move-ment or stress from weight
bearing on painful joints. Acutely in-flamed joints can be rested by applying
splints to limit motion. Splints also support the joint to relieve spasm. Canes
and crutches can relieve stress from inflamed and painful weight-bearing joints
while promoting safe ambulation. Cervical collars may be used to support the
weight of the head and limit cervical motion. A metatarsal bar or special pads
may be put into shoes if foot pain or deformity is present.
Other
strategies for decreasing pain include muscle relaxation techniques, imagery,
self-hypnosis, and distraction.
DECREASING FATIGUE
Fatigue
related to rheumatic disease can be both acute (brief and relieved by rest or
sleep) and chronic. Chronic fatigue, related to the disease process, is
persistent, cumulative, and not eliminated by rest but is influenced by
biologic, psychological, social, and personal factors.
Disease-related
factors that may influence the amount and severity of fatigue include
persistent pain, sleep disturbance, im-paired physical activity, and disease
duration. Pain increases fa-tigue by requiring additional physical and
emotional energy to deal with it. It may also cause the patient to expend more
energy to do tasks in a way that causes less pain. Pain may also interfere with
sleep, thereby increasing the fatigue level (Aaronson et al., 1999; Wolfe &
Skevington, 2000).
Efforts
are aimed at modifying and reducing the fatigue. En-ergy may be regained by
using rest periods. The patient’s needs determine the type and amount of rest
needed. Naps or night-time sleep can provide systemic rest. Splints can provide
articu-lar rest by limiting motion and stress on the joints. Relaxation
techniques can provide emotional rest. Inactivity may lead to de-conditioning
and fatigue, so measures to build endurance should be instituted. Conditioning
exercise, such as walking, swimming, or biking, requires gradual progression of
activity and monitor-ing of disease activity.
Psychosocial
factors with an effect on fatigue include depres-sion, learned helplessness,
and perceived social support (Belza, 2001; Parker et al., 2001). These factors
affect the patient’s per-ception and evaluation of the fatigue. Improvement of
functional status can improve mood. The patient is taught strategies to
con-serve energy, such as planning and grouping activities to mini-mize the
number of times the patient needs to climb the stairs each day and sitting down
to prepare meals.
PROMOTING RESTORATIVE SLEEP
Restful
sleep is important in helping the patient to cope with pain, minimize physical
fatigue, and deal with the changes ne-cessitated by a chronic disease. In
patients with acute disease, sleep time is frequently reduced and fragmented by
prolonged awakenings. Stiffness, depression, and medications may also
compromise the quality of sleep and increase daytime fatigue. A sleep-inducing
routine, medication, and comfort measures may help improve the quality of sleep.
INCREASING MOBILITY
Proper
body positioning is essential to minimize stress on in-flamed joints and
prevent deformities that limit mobility. All joints should be supported in a
position of optimal function. When in bed, the patient should lie flat on a
firm mattress, with feet positioned against a footboard and with only one
pillow under the head because of the risk of dorsal kyphosis. A pillow should
not be placed under the knees because this promotes flex-ion contracture. The
patient should lie prone several times daily to prevent hip flexion
contracture.
Active range-of-motion exercises are encouraged
because they prevent joint stiffness. If the patient cannot actively exercise
the joints, passive range of motion should be performed.
Measures to reinforce proper body posture and increase mo-bility include walking erect and using chairs with straight backs. When seated, the patient should rest the feet flat on the floor and the shoulders and hips against the back of the chair.
Care
must be taken so that splinting for comfort does not re-strict mobility later.
The knee is splinted at full extension and the wrist at slight dorsiflexion.
Because of the predominant strength of flexor muscles, the joints should not be
permitted to “freeze” in positions of flexion. This can be prevented by
regularly re-moving the splint and exercising the joint through a range of
motion. Splint modification may be needed when changes occur in joint
structure.
Additionally, assistive devices may be necessary
for mobility. They should be properly fitted and the patient should be
in-structed in their correct and safe use. A cane, long enough to allow for
only a slight bend of the elbow, should be held in the hand opposite the
affected side. Forearm-trough style crutches (platform crutches) may be needed
to protect the upper extrem-ities if the disease also involves the hands and
wrists. This is es-pecially important for the patient undergoing rehabilitation
after lower extremity joint reconstructive surgery. Assistive devices can mean
the difference between dependence and independence in mobility; however, they
may also alter the patient’s body image, which can become a barrier to
compliance with treatment.
FACILITATING SELF-CARE
Adaptive equipment may increase the patient’s
independence. When introducing adaptive equipment, however, the nurse should be
sensitive to the patient’s feelings by demonstrating ac-ceptance and positive
attitudes about using these devices. The nurse needs to keep in mind that a
patient’s deformity does not necessarily equate with the severity of
limitations or disability. For example, swollen hands may be more limiting than
deformed hands. The nurse in the hospital or in the extended care facility can
help preserve the patient’s independence in these settings by making available
adaptive equipment for eating, toileting, bathing, and dressing. In the home,
the nurse can encourage use of these devices. Again, by relieving pain,
stiffness, and fatigue, the nurse may increase the patient’s ability to perform
self-care (Luck, 2001).
IMPROVING BODY IMAGE AND COPING
All
aspects of the patient’s life, including perception of self, work role, social
life, sexual function, and financial status, may be altered because of the
unpredictability and uncertainty of the course of a rheumatic disease. Body
image changes may cause so-cial isolation and depression. The nurse and the
family need to empathize with the patient’s emotional reactions to the disease.
Communication should be encouraged so that the patient and family verbalize
feelings, perceptions, and fears related to the dis-ease. The nurse helps the
patient and family identify areas in which they have some control over disease
symptoms and treat-ment. The nurse also encourages commitment to the treatment
program, which is a key to positive outcomes, as well as use of effective
coping strategies.
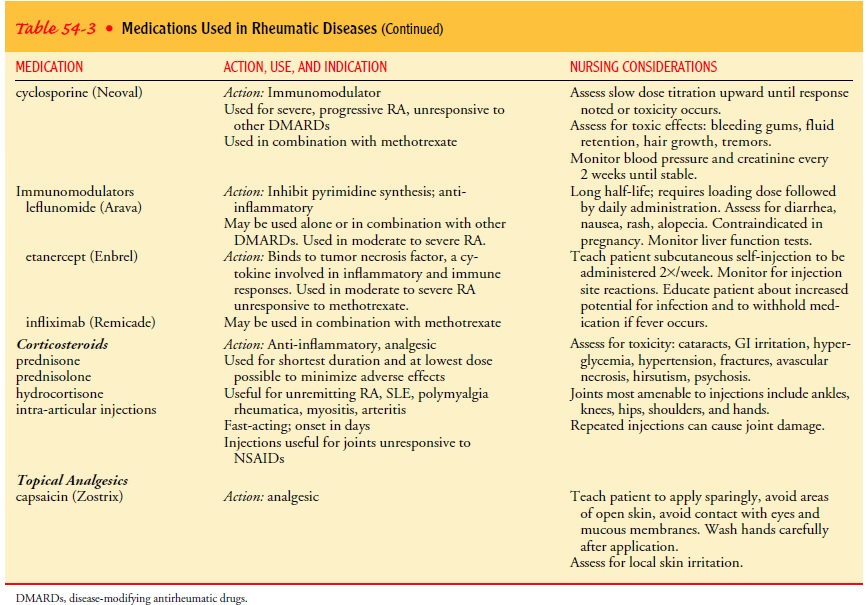
MONITORING AND MANAGINGPOTENTIAL COMPLICATIONS
Medications used for treating rheumatic diseases
have the potential for serious and adverse effects. Thus, an important aspect
of care is avoiding medication-induced complications. The physician bases the
prescribed medication regimen on clinical findings and past medical history,
then monitors for side effects with periodic clin-ical assessments and
laboratory testing. The nurse has a major role in working with the physician
and pharmacist to help the patient recognize and deal with side effects from medications.
These side effects may include gastrointestinal bleeding or irritation, bone
marrow suppression, kidney or liver toxicity, infection, mouth sores, rashes,
and changes in vision. Other signs and symptoms include bruising, breathing
problems, dizziness, jaundice, dark urine, black or bloody stools, diarrhea,
nausea and vomiting, and headaches. Systemic and local infections, which can
often be masked by high doses of corticosteroids, need close monitoring (see
Table 54-3 for more information about administration considerations).
Patient instruction also includes teaching correct
techniques of self-administration of medications, methods of reducing side
effects, and measures to ensure regular monitoring. The nurse can be available
for consultation between physician visits. If side effects occur, the
medication may need to be stopped or the dose reduced. The patient may
experience an increase in symp-toms while the complication is being resolved or
a new med-ication is being initiated. In such cases, the nurse’s counseling
regarding symptom management may relieve potential anxiety and distress.
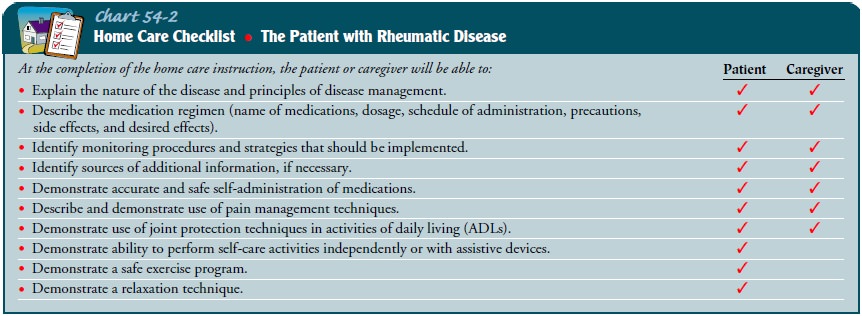
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Patient teaching is an essential aspect of nursing
care of the pa-tient with rheumatic disease to enable the patient to maintain
as much independence as possible, to take medications accurately and safely,
and to use adaptive devices correctly. Patient teaching focuses on the disorder
itself, the possible changes related to the disorder, the therapeutic regimen
prescribed to treat it, the side effects of medications, strategies to maintain
independence and function, and patient safety in the home (Chart 54-2).
The
patient and family are encouraged to verbalize their con-cerns and ask
questions. Pain, fatigue, and depression can inter-fere with the patient’s
ability to learn and should be addressed before initiating teaching. Various
educational strategies may then be used, depending on the patient’s previous
knowledge base, interest level, degree of comfort, social or cultural
influ-ences, and readiness to learn. The nurse instructs the patient about
basic disease management and necessary adaptations in lifestyle. Because
suppression of inflammation and autoimmune responses requires the use of anti-inflammatory,
disease-modifying antirheumatic and immunosuppressive agents, the patient is
taught about prescribed medications, including type, dosage, ra-tionale, side
effects, self-administration, and required monitoring procedures. If
hospitalized, the patient is encouraged to practice new self-management skills
with support from caregivers and sig-nificant others. The nurse then reinforces
disease management skills during each patient contact. Barriers to compliance
are as-sessed and measures are taken to promote adherence to medica-tions and
the treatment program.
Continuing Care
Depending on the severity of the disorder and the patient’s re-sources and supports, referral for home care may or may not be warranted. However, the patient who is elderly or frail, has a rheumatic disorder that limits function significantly, and lives alone may need a referral for home care.
The impact of rheumatic disease on everyday life is
not always evident when the patient is seen in the hospital or an ambulatory
care setting. The increased frequency with which nurses see pa-tients in the
home provides opportunities for recognizing prob-lems and implementing
interventions aimed at improving the quality of life of patients with rheumatic
disorders. The patient encountered in the home setting often has a rheumatic
disease that is secondary to the primary reason for the visit. In such cases,
the problems caused by the rheumatic disease may interfere with the treatment
of the primary condition. For example, the patient who is recovering from
coronary artery surgery may have been in-structed to exercise but is unable or
only partially able to do so because of the rheumatic disease. Conversely,
treatment of the primary condition may cause or increase problems related to
the rheumatic disease. For example, the cardiac patient who has been instructed
to walk long distances every day may find that doing so increases the symptoms
of OA in the knees.
During
home visits, the nurse has the opportunity to assess the home environment and
its adequacy for patient safety and man-agement of the disorder. Compliance
with the treatment program can be more easily monitored in the home setting,
where physi-cal and social barriers to adherence are more readily identified.
For example, the patient with diabetes who requires insulin may be unable to
fill the syringe accurately or administer the insulin because of impaired joint
mobility. Appropriate adaptive equip-ment needed for increased independence is
often identified more readily when the nurse sees how the patient functions in
the home. Any barriers to compliance can be identified and appro-priate
referrals made.
For
patients at risk for impaired skin integrity, the home care nurse can closely
monitor skin status and also instruct, provide, or supervise the patient and
family in preventive skin care mea-sures. The nurse also assesses the patient’s
need for assistance in the home and supervises home health aides, who may meet
many of the needs of the patient with a rheumatic disease. Referrals to
physical and occupational therapists may be made as problems are identified and
limitations increase. A home care nurse can visit the home to make sure the
patient can function as indepen-dently as possible despite mobility problems
and can safely man-age treatments and pharmacotherapy.
Because many of the medications to suppress
inflammation are injectable, the nurse may administer the medication to the
pa-tient or teach self-injection procedure. These frequent contacts allow the
nurse to reinforce other disease management techniques.
The nurse also assesses the patient’s physical and
psychologi-cal status, adequacy of symptom management, and adherence to the
management plan. Previous teaching is reinforced with em-phasis on side effects
of medications and changes in physical sta-tus indicating disease progression
and the need to contact the health care provider for reevaluation; otherwise,
patients may wait until their next appointment. The importance of follow-up appointments
is emphasized to the patient and family.
Patients
with chronic disorders often neglect general health issues if they are focused
on their chronic disorder; therefore, the patient and family should be reminded
about the impor-tance of participating in other health promotion activities and
health screening (eg, immunizations, cholesterol screening, bone density
testing, gynecologic examinations, mammography, colonoscopy).
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Experiences
relief of pain or improved comfort level
a) Identifies
factors that cause or increase pain
b) Identifies
realistic goals for pain relief
c) Uses
pain management strategies safely and effectively
d) Reports
decreased pain and increased comfort level
2) Experiences
reduction in level of fatigue
a) Identifies
factors that contribute to fatigue
b) Verbalizes
the relationship of fatigue to disease activity
c) Schedules
periodic rest periods and identifies and uses other measures to prevent or
modify fatigue
d) Reports
decreased level of fatigue
e) Practices
energy conservation strategies
3) Improves
sleep patterns
a) Reports
fewer night-time awakenings
b) Adheres
to sleep-inducing routine
c) Reports
feeling rested upon awakening
4) Increases
or maintains level of mobility
a) Identifies
factors that impede mobility
b) Participates
in activities and exercises that promote or maintain mobility
c) Uses
assistive devices appropriately and safely
d) Demonstrates
normal or acceptable body alignment and posture
5) Maintains
self-care activities
a) Participates
in self-care activities within capabilities
b) Uses
adaptive equipment and alternative methods to in-crease participation in
self-care activities
c) Maintains
self-care at highest possible level
6) Experiences
improved body image and coping
a) Verbalizes
concerns about the impact of rheumatic dis-ease on appearance and function
b) Sets
and achieves meaningful goals
c) States
acceptance of self-worth
d) Adapts
to body image changes caused by disease
e) Identifies
and uses effective coping strategies
7) Experiences
absence of complications
a) Takes
medications as prescribed
b) States
potential side effects of medications and names reportable side effects
c) Verbalizes
understanding of rationale for monitoring
d) Complies
with recommendations for monitoring
e) Identifies
strategies to reduce risks of side effects
Related Topics