Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Rheumatic Disorders
Metabolic and Endocrine Diseases Associated With Rheumatic Disorders: Gout
Metabolic and Endocrine
Diseases Associated With Rheumatic
Disorders
Metabolic and endocrine diseases may be associated
with rheumatic disorders. These include biochemical abnormalities (amyloidosis
and scurvy), endocrine diseases (diabetes mellitus and acromegaly),
immunodeficiency diseases (HIV infection, AIDS), and other hereditary disorders
(hypermobility syndromes). The most common conditions, however, are the
crystal-induced arthropathies in which crystals, such as monosodium urate
(gout) or calcium pyrophosphate (calcium pyrophosphate dihydrate
disease [CPPD] or pseudogout), are deposited within joints and other tissues.
GOUT
Gout
is a heterogeneous group of conditions related to a genetic defect of purine
metabolism resulting in hyperuricemia. Over-secretion of uric acid or a renal
defect resulting in decreased excretion of uric acid, or a combination of both,
occurs. The prevalence of gout is reported to be 1.6 to 13.6 per thousand. The
incidence increases with age and body mass index. It occurs more commonly in
males than females (Ruddy et al., 2001).
In primary hyperuricemia, elevated serum urate
levels or man-ifestations of urate deposition appear to be consequences of
faulty uric acid metabolism. Primary hyperuricemia may be due to se-vere
dieting or starvation, excessive intake of foods that are high in purines
(shellfish, organ meats), or heredity. In secondary hy-peruricemia, gout is a
clinical feature secondary to any of a num-ber of genetic or acquired processes,
including conditions in which there is an increase in cell turnover (leukemia,
multiple myeloma, some types of anemias, psoriasis) and an increase in cell
breakdown. Altered renal tubular function, either as a major ac-tion or as an
unintended side effect of certain pharmacologic agents (diuretics such as
thiazides and furosemide), low-dose sal-icylates, and ethanol can contribute to
uric acid underexcretion.
Pathophysiology
Hyperuricemia (serum concentration greater than 7
mg/dL [0.4 fmol/L]) can but does not always cause monosodium urate crystal
deposition. However, as uric acid levels rise, risk increases (Ruddy et al.,
2001). Attacks of gout appear to be related to sud-den increases or decreases
of serum uric acid levels. When the urate crystals precipitate within a joint,
an inflammatory response occurs and an attack of gout begins. With repeated
attacks, accu-mulations of sodium urate crystals, called tophi, are deposited in peripheral areas of the body, such as the
great toe, the hands, and the ear. Renal urate lithiasis (kidney stones) with
chronic renal disease secondary to urate deposition may develop.
The finding of urate crystals in the synovial fluid
of asympto-matic joints suggests that factors other than crystals may be
related to the inflammatory reaction. Recovered monosodium urate crys-tals are
coated with immunoglobulins that are mainly immuno-globulin G (IgG). IgG
enhances crystal phagocytosis, thereby demonstrating immunologic activity.
Clinical Manifestations
Manifestations of the gout syndrome include acute
gouty arthritis (recurrent attacks of severe articular and periarticular
inflamma-tion), tophi (crystalline deposits accumulating in articular tissue,
osseous tissue, soft tissue, and cartilage), gouty nephropathy (renal impairment),
and uric acid urinary calculi. Four stages of gout can be identified:
asymptomatic hyperuricemia, acute gouty arthritis, intercritical gout, and
chronic tophaceous gout. The subsequent development of gout is directly related
to the dura-tion and magnitude of the hyperuricemia. Therefore, the com-mitment
to lifelong pharmacologic treatment of hyperuricemia is deferred until there is
an initial attack of gout.
For hyperuricemic people who are going to develop
gout, acute arthritis is the most common early clinical manifestation. The
metatarsophalangeal joint of the big toe is the most commonly affected (75% of
patients). The tarsal area, ankle, or knee may also be affected. Less commonly,
the wrists, fingers, and elbows may be affected. The acute attack may be
triggered by trauma, alcohol ingestion, dieting, medications, surgical stress,
or illness. The abrupt onset often occurs at night, awakening the patient with
se-vere pain, redness, swelling, and warmth of the affected joint. Early
attacks tend to subside spontaneously over 3 to 10 days even without treatment.
The attack is followed by a symptom-free period (the intercritical stage) until
the next attack, which may not come for months or years. With time, however,
attacks tend to occur more frequently, involve more joints, and last longer.
Tophi
are generally associated with more frequent and severe inflammatory episodes.
Higher serum concentrations of uric acid are also associated with more
extensive tophus formation. Tophi most commonly occur in the synovium,
olecranon bursa, sub-chondral bone, infrapatellar and Achilles tendons,
subcutaneous tissue on the extensor surface of the forearms, and overlying
joints. They have also been found in the aortic walls, heart valves, nasal and
ear cartilage, eyelids, cornea, and sclerae. Joint enlarge-ment may cause a
loss of joint motion. Uric acid deposits may cause renal stones and kidney
damage.
Medical Management
A definitive diagnosis of gouty arthritis is
established by polarized light microscopy of the synovial fluid of the involved
joint. Uric acid crystals are seen within the polymorphonuclear leukocytes
within the fluid. Colchicine (oral or parenteral) or an NSAID such as
indomethacin is used to relieve an acute attack of gout. Management of
hyperuricemia, tophi, joint destruction, and renal disorders is usually
initiated after the acute inflammatory process has subsided. Uricosuric agents,
such as probenecid, cor-rect hyperuricemia and dissolve deposited urate.
Allopurinol is also effective, but its use is limited because of the risk for
toxicity. When reduction of the serum urate level is indicated, the urico-suric
agents are the medications of choice. When the patient has, or is at risk for,
renal insufficiency or renal calculi (kidney stones), allopurinol is the
medication of choice. Corticosteroids may be used in resistant cases. If the
individual experiences several acute episodes or there is evidence of tophi
formation, prophylactic treatment is considered. Specific treatment is based on
serum uric acid level, 24-hour urinary uric acid excretion, and renal function
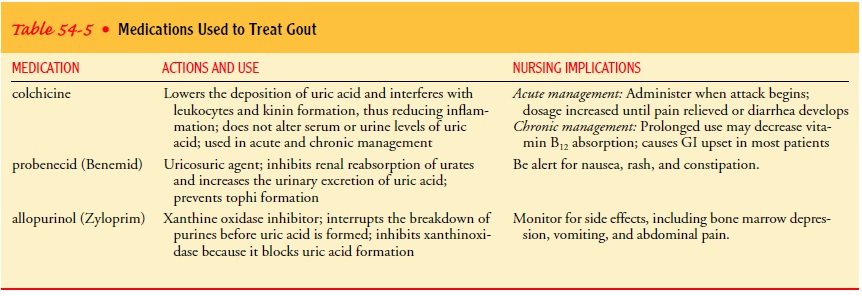
(Table 54-5).
Nursing Management
Historically, gouty arthritis was thought to be a condition of the royalty and the very rich, with the disease attributed to “high living.” This has not been shown to be entirely true. While severe dietary restriction is not necessary, patients should be encouraged to restrict consumption of foods high in purines, especially organ meats, and to limit alcohol intake. Maintenance of normal body weight should be encouraged. In an acute episode of gouty arthri-tis, pain management is essential. During the intercritical period, the patient feels well and may abandon preventive behaviors, which may result in an acute attack. Acute attacks are most effectively treated if therapy is begun early in the course.
Related Topics