Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Rheumatic Disorders
Degenerative Joint Disease (Osteoarthritis)
Degenerative Joint Disease
(Osteoarthritis)
OA,
also known as degenerative joint disease or osteoarthrosis (even though
inflammation may be present), is the most common and frequently disabling of
the joint disorders. OA is both over-diagnosed and trivialized; it is frequently
overtreated or under-treated. The functional impact of OA on quality of life,
especially for elderly patients, is often ignored.
OA has been classified as primary (idiopathic),
with no prior event or disease related to the OA, and secondary, resulting from
previous joint injury or inflammatory disease. The distinction be-tween primary
and secondary OA is not always clear.
Increasing
age directly relates to the degenerative process in the joint, as the ability
of the articular cartilage to resist micro-fracture with repetitive low loads
diminishes. OA often begins in the third decade of life and peaks between the
fifth and sixth decades. By age 75 years, 85% of the population has either
x-ray or clinical evidence of OA, but only 15% to 25% of these people
experience significant symptoms (Ruddy et al., 2001).
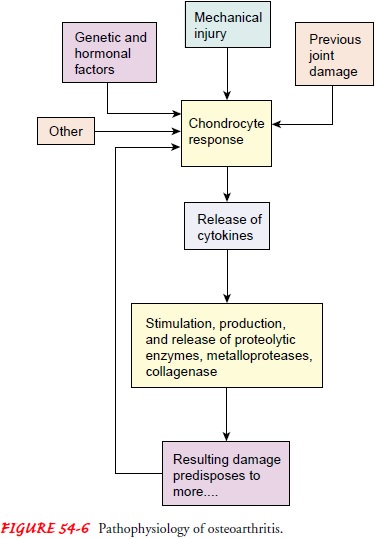
Pathophysiology
OA may be thought of as the end result of many
factors combin-ing in a generalized predisposition to the disease. OA affects
the articular cartilage, subchondral bone (the bony plate that sup-ports the
articular cartilage), and synovium. A combination of cartilage degradation,
bone stiffening, and reactive inflammation of the synovium occurs. The basic
degenerative process in the joint exemplified in OA is presented in Figure 54-6.
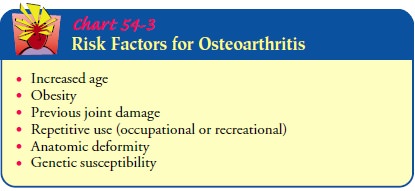
Under-standing of OA has been greatly expanded beyond what previ-ously was
thought of as simply “wear and tear” related to aging. Risk factors for OA are
summarized in Chart 54-3.
Congenital and developmental disorders of the hip are well known for predisposing a person to OA of the hip. These include congenital subluxation–dislocation of the hip, acetabular dysplasia, Legg-Calvé-Perthes disease, and slipped capital femoral epiphysis.
Obesity
is now a well-recognized risk factor for the develop-ment of OA (USDHHS, 2001).
Being overweight or obese also increases the pain and discomfort associated
with the disease (Altman et al., 2000; Coggon et al., 2001).
Clinical Manifestations
The primary clinical manifestations of OA are pain, stiffness, and functional impairment. The pain is due to an inflamed synovium, stretching of the joint capsule or ligaments, irritation of nerve endings in the periosteum over osteophytes, trabecular micro-fracture, intraosseous hypertension, bursitis, tendinitis, and mus-cle spasm. Stiffness, which is most commonly experienced in the morning or after awakening, usually lasts less than 30 minutes and decreases with movement. Functional impairment is due to pain on movement and limited motion caused by structural changes in the joints.
Although
OA occurs most often in weight-bearing joints (hips, knees, cervical and lumbar
spine), the proximal and distal finger joints are also often involved.
Characteristic bony nodes may be present; on inspection and palpation, these
are usually painless, unless inflammation is present.
Assessment and Diagnostic Findings
Diagnosis of OA is complicated because only 30% to
50% of patients with changes seen on x-rays report symptoms. Physical
assessment of the musculoskeletal system reveals tender and en-larged joints.
Inflammation, when present, is not the destructive type seen in the connective
tissue diseases such as RA. OA is char-acterized by a progressive loss of the
joint cartilage, which appears on x-ray as a narrowing of joint space. In
addition, reactive changes occur at the joint margins and on the subchondral
bone in the form of osteophytes (or spurs) as the cartilage attempts to
regenerate. Neither the presence of osteophytes nor joint space narrowing alone
is specific for OA; however, when combined, these are sensitive and specific
findings. In early or mild OA, there is only a weak correlation between joint
pain and synovitis. Blood tests are not useful in the diagnosis of OA.
Medical Management
Although
no treatment halts the degenerative process, certain preventive measures can
slow the progress if undertaken early enough. These include weight reduction,
prevention of injuries, perinatal screening for congenital hip disease, and
ergonomic modifications.
Conservative treatment measures include the use of
heat, weight reduction, joint rest and avoidance of joint overuse, orthotic
devices to support inflamed joints (splints, braces), isometric and postural
exercises, and aerobic exercise. Occupational and physi-cal therapy can help
the patient adopt self-management strategies.
PHARMACOLOGIC THERAPY
Pharmacologic management of OA is directed toward
symptom management and pain control. Medications are used in conjunc-tion with
nonpharmacologic strategies, which are the mainstay of OA management (Altman et
al., 2000). In most patients with OA, the initial analgesic therapy is
acetaminophen. Some patients respond to the nonselective NSAIDs, and patients
who are at in-creased risk for gastrointestinal complications, especially
gastro-intestinal bleeding, have been managed effectively with COX-2 inhibitors
(Altman et al., 2000; Beehrle & Evans, 1999; Bom-bardier et al., 2000;
Pasero & McCaffery, 2001; Ruddy et al., 2001). Selection of medication is
based on the patient’s needs, the stage of disease, and the risk for side
effects. Other medications that may be considered are the opioids and
intra-articular cortico-steroids. Topical analgesics such as capsaicin and
methylsalicylate are also recommended (Altman et al., 2000; Ruddy et al.,
2001).
Newer therapeutic approaches include glucosamine
and chon-droitin, which are thought to improve tissue function and retard
breakdown of cartilage (Altman et al., 2000; McAlindon et al., 2000). Viscosupplementation,
the intra-articular injection of hyal-uronic acid, is thought to improve
cartilage function and retard degradation; it may also have some
anti-inflammatory effects (Huskisson & Donnelly, 1999; Watterson &
Esdaile, 2000; Wright et al., 2000). Glucosamine and chondroitin and viscosupplementation,
although approved by the FDA, are still under-going intensive investigation for
safety and efficacy (Brandt et al., 2000).
SURGICAL MANAGEMENT
In moderate to severe OA, when pain is severe or
because of loss of function, surgical intervention may be used. Procedures most
commonly used are osteotomy (to alter the force distribution in the joint) and
arthroplasty. In arthroplasty, diseased joint com-ponents are replaced with
artificial products.
Other procedures include viscosupplementation (the
recon-stitution of synovial fluid viscosity). Hyaluronic acid (Hyalgan,
Synvisc), a glycosaminoglycan that acts as a lubricant and shock-absorbing
fluid in the joint, may be used in this procedure. Hyaluronic acid stimulates
the production of synoviocytes, pos-sibly providing better and more prolonged
pain control. A series of three to five weekly intra-articular injections are
given. Pain relief may last for 6 months (Kellick et al., 1998).
Tidal
irrigation (lavage) of the knee involves the introduction and then removal of a
large volume of saline into the joint through cannulas. In some cases it
provides pain relief for up to 6 months (Klippel, 2001; Lozada & Altman,
2001).
Nursing Management
The nursing management of the patient with OA
includes both pharmacologic and nonpharmacologic approaches. The
non-pharmacologic interventions are used first and continued with the addition
of pharmacologic agents. Pain management and op-timizing functional ability are
major goals of nursing intervention. Patients’ understanding of their disease
process and symptom pattern is critical to a plan of care. Because patients
with OA are older, they may have other health problems. Commonly they are
overweight, and they may have a sedentary lifestyle. Weight loss and an
increase in aerobic activity such as walking, with special attention to
quadriceps strengthening, are important approaches to pain management (Altman
et al., 2000; Bautch et al., 1997; Ettinger et al., 1997). A referral for
physical therapy or to an ex-ercise program for individuals with similar
problems may be very helpful. Canes or other assistive devices for ambulation
should be considered. Exercises such as walking should be begun in mod-eration
and increased gradually. Patients should plan their daily exercise for a time
when the pain is least severe or should plan to use an analgesic, if
appropriate, before exercising. Adequate pain management is important for the
success of an exercise program.
Related Topics