Chapter: Medical Surgical Nursing: Management of Patients With Chronic Obstructive Pulmonary Disease
Nursing Process: The Patient With COPD
NURSING PROCESS: THE PATIENT WITH COPD
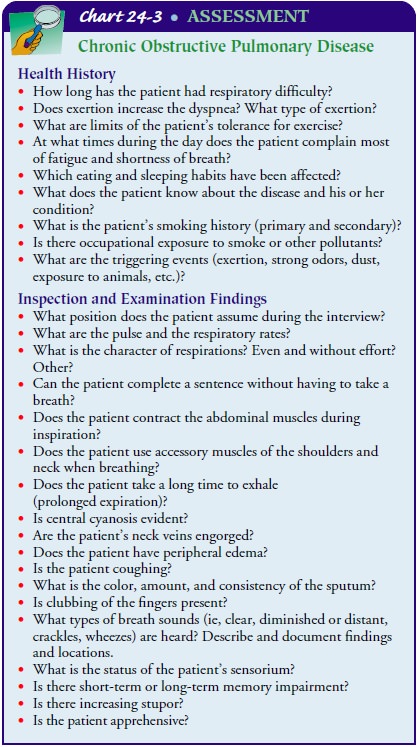
Assessment
Assessment
involves obtaining information about current symp-toms as well as previous
disease manifestations. Chart 24-3 lists sample questions that may be used to
obtain a clear history of the disease process. In addition to the history, the
nurse also reviews the results of available diagnostic tests.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the patient’s major nursing diag-noses may include the
following:
·
Impaired gas exchange and airway
clearance due to chronic inhalation of toxins
·
Impaired gas exchange related to
ventilation–perfusion inequality
·
Ineffective airway clearance related
to bronchoconstriction, increased mucus production, ineffective cough,
broncho-pulmonary infection, and other complications
·
Ineffective breathing pattern
related to shortness of breath, mucus, bronchoconstriction, and airway
irritants
·
Activity intolerance due to fatigue,
ineffective breathing patterns, and hypoxemia
·
Deficient knowledge of self-care
strategies to be performed at home.
·
Ineffective coping related to
reduced socialization, anxiety, depression, lower activity level, and the
inability to work
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on the assessment data, potential complications that may develop include:
•
Respiratory insufficiency or failure
•
Atelectasis
•
Pulmonary infection
•
Pneumonia
•
Pneumothorax
•
Pulmonary hypertension
Planning and Goals
The
major goals for the patient may include smoking cessation, improved gas
exchange, airway clearance, improved breathing pattern, improved activity
tolerance, maximal self-management, improved coping ability, adherence to the
therapeutic program and home care, and absence of complications.
Nursing Interventions
PROMOTING SMOKING CESSATION
Because
smoking has such a detrimental effect on the lungs, the nurse must discuss
smoking cessation strategies with patients. Although patients may believe that
it is too late to reverse the dam-age from years of smoking and that smoking
cessation is futile, they should be informed that continuing to smoke impairs
the mechanisms that clear the airways and keep them free of irritants. The
nurse should educate the patient regarding the hazards of smoking and cessation
strategies and provide resources regarding smoking cessation, counseling, and
formalized programs available in the community.
IMPROVING GAS EXCHANGE
Bronchospasm,
which occurs in many pulmonary diseases, re-duces the caliber of the small
bronchi and may cause dyspnea, static secretions, and infection. Bronchospasm
can sometimes be detected when wheezing or diminished breath sounds are heard
on auscultation with a stethoscope. Increased mucus production, along with
decreased mucociliary action, contributes to further reduction in the caliber
of the bronchi and results in decreased airflow and decreased gas exchange.
This is further aggravated by the loss of lung elasticity that occurs with COPD
(NIH, 2001).
These
changes in the airway require that the nurse monitor the patient for dyspnea
and hypoxemia. If bronchodilators or corti-costeroids are prescribed, the nurse
must administer the medica-tions properly and be alert for potential side
effects. The relief of bronchospasm is confirmed by measuring improvement in
expi-ratory flow rates and volumes (the force of expiration, how long it takes
to exhale, and the amount of air exhaled) and assessing whether the patient has
less dyspnea.
ACHIEVING AIRWAY CLEARANCE
Diminishing
the quantity and viscosity of sputum can clear the airway and improve pulmonary
ventilation and gas exchange. All pulmonary irritants should be eliminated or
reduced, particularly cigarette smoking, which is the most persistent source of
pul-monary irritation. The nurse instructs the patient in directed or
controlled coughing, which is more effective and reduces the fatigue associated
with undirected forceful coughing. Directed coughing consists of a slow, maximal
inspiration followed by breath-holding for several seconds and then two or
three coughs. “Huff” coughing may also be effective. The technique consists of
one or two forced exhalations (“huffs”) from low to medium lung volumes with
the glottis open.
Chest
physiotherapy with postural drainage, intermittent positive-pressure breathing,
increased fluid intake, and bland aerosol mists (with normal saline solution or
water) may be use-ful for some patients with COPD. The use of these measures
must be based on the patient’s response and tolerance.
IMPROVING BREATHING PATTERNS
Ineffective
breathing patterns and shortness of breath are due to the ineffective
respiratory mechanics of the chest wall and lung re-sulting from air trapping, ineffective diaphragmatic
movement, airway obstruction, the metabolic cost of breathing, and stress.
In-spiratory muscle training and breathing retraining may help to im-prove
breathing patterns. Training in diaphragmatic breathing reduces the respiratory
rate, increases alveolar ventilation, and sometimes helps expel as much air as
possible during expiration. Pursed-lip breathing helps to slow expiration,
prevents collapse of small airways, and helps the patient to control the rate
and depth of respiration. It also promotes relaxation, which enables the
pa-tient to gain control of dyspnea and reduce feelings of panic.
IMPROVING ACTIVITY TOLERANCE
Patients
with COPD experience progressive activity and exercise intolerance. Education
is focused on rehabilitative therapies to promote independence in executing
activities of daily living. These may include pacing activities throughout the
day or using supportive devices to decrease energy expenditure. The nurse
evaluates the patient’s activity tolerance and limitations and teaching strategies
to promote independent activities of daily liv-ing. Also, the patient may be a
candidate for exercise training to strengthen the muscles of the upper and
lower extremities and improve exercise tolerance and endurance. Other health
care pro-fessionals (rehabilitation therapy, occupational therapy, physical
therapy) may be consulted as additional resources.
ENHANCING SELF-CARE STRATEGIES
In
addition to a pulmonary rehabilitation program, the nurse helps the patient
manage self-care by emphasizing the importance of setting realistic goals,
avoiding temperature extremes, and modifying lifestyle (particularly stopping
smoking) as applicable.
Setting Realistic Goals
A
major area of teaching is the importance of setting and accept-ing realistic
short-term and long-range goals. If the patient is se-verely disabled, the
objectives of treatment are to preserve current pulmonary function and relieve
symptoms as much as possible. If the disease is mild, the objectives are to
increase exercise toler-ance and prevent further loss of pulmonary function. It
is im-portant to plan and share the goals and expectations of treatment with
the patient. The patient and those providing care need pa-tience to achieve
these goals.
Avoiding Temperature Extremes
The
nurse instructs the patient to avoid extremes of heat and cold. Heat increases
the body temperature, thereby raising oxy-gen requirements; cold tends to
promote bronchospasm. Air pol-lutants such as fumes, smoke, dust, and even
talcum, lint, and aerosol sprays may initiate bronchospasm. High altitudes
aggra-vate hypoxemia.
Modifying Lifestyle
Patients
with COPD should adopt a lifestyle of moderate activ-ity, ideally in a climate
with minimal shifts in temperature and humidity. As much as possible, the
patient should avoid emo-tional disturbances and stressful situations that
might trigger a coughing episode. The medication regimen for patients with COPD
can be quite complex; patients receiving aerosol medica-tions by an MDI may be
particularly challenged. It is crucial to review this material and to have the
patient perform a return demonstration before discharge, during follow-up
visits to the caregiver’s office or clinic, and during home visits (Chart
24-4).
Smoking
cessation goes hand in hand with lifestyle changes, and reinforcement of the
patient’s efforts is a key nursing activ-ity. Smoking cessation is the single
most important therapeutic intervention for patients with COPD. There are many
strategies, including prevention, cessation with or without oral or topical
patch medications, and behavior modification techniques.
ENHANCING INDIVIDUAL COPING STRATEGIES
COPD
and its progression promote a cycle of physical, social, and psychological
consequences, all which are interrelated. Pa-tients experience depression,
altered mood states, social isolation, and altered functional status. The nurse
is key to identifying this cycle and promoting interventions for improved
physical func-tioning, psychological and emotional stability, and social
sup-port. Following the initial assessment of the patient, the nurse may
provide referrals to health care professionals in these specific areas.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
The
nurse caring for the patient with COPD must assess for var-ious complications,
such as life-threatening respiratory insuffi-ciency and failure and respiratory
infection and atelectasis, which may increase the patient’s risk for
respiratory failure. The nurse also monitors for cognitive changes (personality
and behavioral changes, memory impairment), increasing dyspnea, tachypnea, and
tachycardia, which may indicate increasing hypoxemia and impending respiratory
failure.
The
nurse monitors pulse oximetry values to assess the pa-tient’s need for oxygen
and administers supplemental oxygen as prescribed. The nurse also instructs the
patient about signs and symptoms of respiratory infection that may worsen
hypoxemia and reports changes in the patient’s physical and cognitive status to
the physician. Other activities require assisting with the man-agement of
developing complications, with possible intubation and mechanical ventilation.
Bronchopulmonary infections must be controlled to diminish inflammatory edema and to permit recovery of normal ciliary ac-tion. Minor respiratory infections that are of no consequence to the person with normal lungs can be life-threatening to the person with COPD. The cough associated with bronchial infection intro-duces a vicious cycle with further trauma and damage to the lungs, progression of symptoms, increased bronchospasm, and increased susceptibility to bronchial infection. Infection compromises lung function and is a common cause of respiratory failure in patients with COPD.
In
COPD, infection may be accompanied by subtle changes. The nurse instructs the
patient to report any signs of infection, such as a fever or change in sputum
color, character, consistency, or amount. Any worsening of symptoms (increased
tightness of the chest, increased dyspnea and fatigue) also suggests infection
and must be reported. Viral infections are hazardous to these patients because
they are often followed by infections caused by bacterial organisms, such as Streptococcus pneumoniae and Haemophilusinfluenzae.
The
nurse should encourage patients with COPD to be im-munized against influenza
and S. pneumoniae because these
pa-tients are prone to respiratory infection. It is important to caution
patients to avoid going outdoors if the pollen count is high or if there is
significant air pollution because of the risk of bronchospasm. The patient also
should avoid exposure to high out-door temperatures with high humidity.
Pneumothorax
is a potential complication of COPD. Patients with severe emphysematous changes
can develop large bullae, which may rupture and cause a pneumothorax. The
development of a pneumothorax may be spontaneous or related to an activity such
as severe coughing or large intrathoracic pressure changes. If the patient
develops a rapid onset of shortness of breath, the nurse should quickly
evaluate the patient for a potential pneumothorax by assessing the symmetry of
chest movement, differences in breath sounds, and pulse oximetry. A
pneumothorax is a life-threatening event in the patient with COPD who has
minimal pulmonary reserve.
Over
time, pulmonary hypertension may occur as a result of chronic hypoxemia. The
pulmonary arteries respond to hypox-emia by constriction, thus leading to
pulmonary hypertension.The complication may be prevented by maintaining
adequate oxygenation through an adequate hemoglobin level, improved
ventilation/perfusion of the lungs, or continuous administration of
supplemental oxygen (if needed).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Teaching
is essential throughout the course of COPD and should be part of the nursing
care given to every patient with COPD. Pa-tients’ and family members’ knowledge
and comfort level with their knowledge should be assessed and considered when
provid-ing instructions about self-management strategies. In addition to the
aspects of patient education previously described, patients and family members
must become familiar with the medications that are prescribed and knowledgeable
about potential side ef-fects. Patients and family members need to learn the
early signs and symptoms of infection and other complications so that they seek
appropriate health care promptly.
Continuing Care
Referral
for home care is important to enable the nurse to assess the patient’s home
environment and physical and psychological status, to evaluate the patient’s
adherence to the prescribed regi-men, and to assess the patient’s ability to
cope with changes in lifestyle and physical status. The nurse assesses the
patient’s and family’s understanding of the complications and side effects of
medications. The home care visit provides an opportunity to re-inforce the
information and activities learned in the inpatient or outpatient pulmonary
rehabilitation program and to have the pa-tient and family demonstrate correct
administration of medications and oxygen, if indicated, and performance of
exercises. If the pa-tient does not have access to a formal pulmonary
rehabilitation program, it is important for the nurse to provide the education
and breathing retraining necessary to optimize the patient’s func-tional
status.
The
nurse may direct patients to community resources such as pulmonary
rehabilitation programs and smoking cessation programs to help improve their
ability to cope with their chronic condition and the therapeutic regimen and to
give them a sense of worth, hope, and well-being. In addition, the nurse
reminds the patient and family about the importance of participating in general
health promotion activities and health screening.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1.
Demonstrates knowledge of hazards of
smoking
a.
Verbalizes willingness/interest to
quit smoking
b.
Verbalizes information about
smoking, risks of contin-uing, benefits of quitting, and techniques to optimize
cessation efforts
2.
Demonstrates improved gas exchange
a.
Shows no signs of restlessness,
confusion, or agitation
b.
Has stable pulse oximetry or
arterial blood gas values (but not necessarily normal values due to chronic
changes in the gas exchange ability of the lungs)
3.
Achieves maximal airway clearance
a.
Stops smoking
b.
Avoids noxious substances and
extremes of temperature
c.
Maintains adequate hydration
d.
If indicated, performs postural
drainage correctly
e.
Knows signs of early infection and
is aware of how and when to report them if they occur
f.
Performs controlled coughing without
experiencing excessive fatigue
4.
Improves breathing pattern
a.
Practices and uses pursed-lip and
diaphragmatic breath-ing
b.
Shows signs of decreased respiratory
effort (decreased respiratory rate, less dyspnea)
5.
Demonstrates knowledge of strategies
to improve activity tolerance and maintain maximum level of self-care
a.
Performs self-care activities within
tolerance range
b.
Paces self to avoid fatigue and
dyspnea
c.
Uses controlled breathing while
performing activities
d.
Uses devices to assist with activity
tolerance and de-crease energy expenditure
6.
Demonstrates knowledge of self-care
strategies
a.
Participates in determining the
therapeutic program
b.
Understands the rationale for
activities and medications
c.
Follows the medication plan
d.
Uses bronchodilators and oxygen
therapy as prescribed
e.
Stops smoking
f.
Maintains acceptable activity level
7.
Uses effective coping mechanisms for
dealing with conse-quences of disease
a.
Uses self-care strategies to lessen
stress associated with disease
b.
Verbalizes resources available to
deal with psychological burden of disease
c.
Participates in pulmonary
rehabilitation, if appropriate
8.
Uses community resources and
home-based care
a.
Verbalizes knowledge of community
resources (eg, smoking cessation, hospital/community-based support groups)
b.
Participates in pulmonary
rehabilitation, if appropriate
9.
Avoids or reduces complications
a.
Has no evidence of respiratory
failure or insufficiency
b.
Maintains adequate pulse oximetry
and arterial blood gas values
c.
Shows no signs or symptoms of
infection, pneumotho-rax, or pulmonary hypertension
For
more information, see Plan of Nursing Care: Care of the Patient With COPD.
Related Topics