Chapter: Medical Surgical Nursing: Management of Patients With Chronic Obstructive Pulmonary Disease
Chronic Obstructive Pulmonary Disease
Chronic Obstructive
Pulmonary Disease
Chronic obstructive pulmonary disease
(COPD) is a disease state characterized
by airflow limitation that is not fully reversible.This newest definition of
COPD, provided by the Global Initiative for Chronic Obstructive Lung Disease,
provides a broad description that better explains this disorder and its signs
and symptoms (National Institutes of Health [NIH], 2001). While previous definitions
have included emphysema and chronic bronchitis under the umbrella
classification of COPD, this was often confusing because most patients with
COPD present with overlapping signs and
symptoms of these
two distinct disease processes.
COPD may include diseases that cause
airflow obstruction(eg, emphysema, chronic bronchitis) or a combination of
these disorders. Other diseases such as cystic fibrosis, bronchiectasis, and
asthma were previously classified as types of chronic obstructive lung disease.
However, asthma is now considered a separate disorder and is classified as an
abnormal airway condition characterized primarily by reversible inflammation.
COPD can coexist with asthma. Both of these diseases have the same major
symptoms; however, symptoms are generally more variable in asthma than in COPD.
COPD is the fifth leading cause of death
in the United States for all ages and both genders; fifth for men and fourth
for women(National Center for Health Statistics [NCHS], 2000). In 1998,more
than 12,000 persons died of COPD. This represents a rise in the mortality rate
for this disorder at a time when death ratesfrom other serious illnesses, such
as heart disease and cerebral vascular disease, were declining. Approximately
16 million people in the United States have some form of COPD; it is
responsible for over 13.4 million office visits per year and is the third most
frequent justification for home care services (NCHS, 2000; National Heart, Lung
and Blood Institute [NHLBI], 1998). People with COPD commonly become
symptomatic during the middle adult years, and the incidence of COPD increases
with age. Although certain aspects of lung function normally decrease with age
(eg, vital capacity and forced expiratory volume in 1 second [FEV1]), COPD
accentuates and accelerates these physiologic changes.
Pathophysiology
In COPD, the airflow limitation is both
progressive and associated with an abnormal inflammatory response of the lungs
to noxious particles or gases. The inflammatory response occurs throughout the
airways, parenchyma, and pulmonary vasculature (NIH,2001). Because of the
chronic inflammation and the body’s attempts to repair it, narrowing occurs in
the small peripheral airways. Over time, this injury-and-repair process causes
scar tissue formation and narrowing of the airway lumen. Airflow obstruction
may also be due to parenchymal destruction as seen with emphysema, a disease of
the alveoli or gas exchange units.In addition to inflammation, processes
relating to imbalances of proteinases and antiproteinases in the lung may be
responsible for airflow limitation. When activated by chronic inflammation,
proteinases and other substances may be released, damaging the parenchyma of
the lung. The parenchymal changes may also be consequences of inflammation,
environmental, or genetic factors(eg, alpha1 antitrypsin deficiency).Early in
the course of COPD, the inflammatory response causes pulmonary vasculature
changes that are characterized by thickening of the vessel wall. These changes
may occur as a result of exposure to cigarette smoke or use of tobacco products
or as a result of the release of inflammatory mediators (NIH, 2001).
Chronic Bronchitis
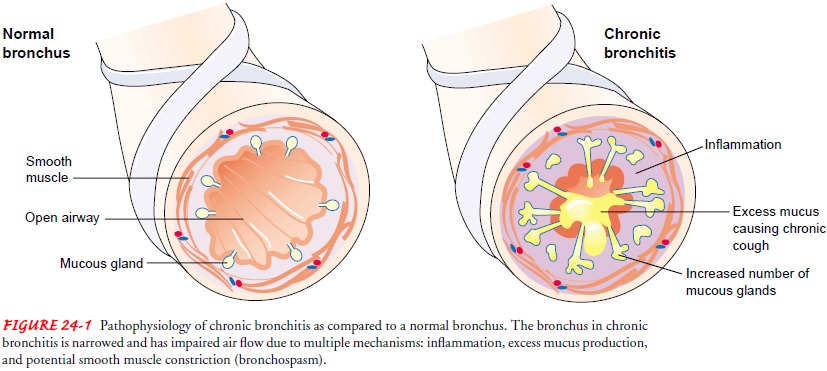
Chronic bronchitis, a disease of the
airways, is defined as the presence of cough and sputum production for at least
3 months in each of 2 consecutive years. In many cases, smoke or other
environmental pollutants irritate the airways, resulting in hypersecretionof
mucus and inflammation. This constant irritation causes the mucus-secreting
glands and goblet cells to increase in number, ciliary function is reduced, and
more mucus is produced. The bronchial walls become thickened, the bronchial
lumen is nar-rowed, and mucus may plug the airway (Fig. 24-1). Alveoli
adja-cent to the bronchioles may become damaged and fibrosed, resulting in
altered function of the alveolar macrophages. This is significant because the
macrophages play an important role in de-stroying foreign particles, including
bacteria. As a result, the pa-tient becomes more susceptible to respiratory infection.
A wide range of viral, bacterial, and mycoplasmal infections can produce acute
episodes of bronchitis. Exacerbations of chronic bronchitis are most likely to
occur during the winter.
Emphysema
In
emphysema, impaired gas exchange
(oxygen, carbon dioxide) results from destruction of the walls of overdistended
alveoli. “Emphysema” is a pathological term that describes an abnormal
distention of the air spaces beyond the terminal bronchioles, with destruction
of the walls of the alveoli. It is the end stage of a process that has
progressed slowly for many years. As the walls of the alveoli are destroyed (a
process accelerated by recurrent in-fections), the alveolar surface area in
direct contact with the pul-monary capillaries continually decreases, causing
an increase in dead space (lung area where no gas exchange can occur) and
im-paired oxygen diffusion, which leads to hypoxemia. In the later stages of
the disease, carbon dioxide elimination is impaired, resulting in increased
carbon dioxide tension in arterial blood (hypercapnia) and causing respiratory
acidosis. As the alveolar walls continue to break down, the pulmonary capillary
bed is re-duced. Consequently, pulmonary blood flow is increased, forcing the
right ventricle to maintain a higher blood pressure in the pul-monary artery.
Hypoxemia may futher increase pulmonary artery pressure. Thus, right-sided
heart failure (cor pulmonale) is one of the complications of emphysema.
Congestion, dependent edema, distended neck veins, or pain in the region of the
liver suggests the development of cardiac failure.
There are two main types of emphysema, based on the changes taking place in the lung: panlobular (panacinar) and centrilobular (centroacinar) (Fig. 24-2). Both types may occur in the same patient.
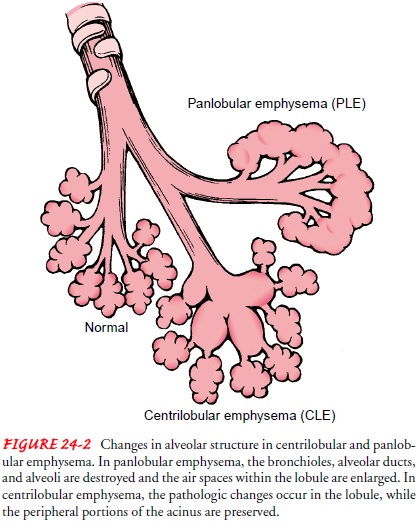
In the panlobular (panacinar) type, there is destruction of the respiratory
bronchiole, alveolar duct, and alveoli. All air spaces within the lobule are
essentially enlarged, but there is little in-flammatory disease. The patient
with this type of emphysema typically has a hyperinflated (hyperexpanded) chest
(barrel chest on physical examination), marked dyspnea on exertion, and weight
loss. To move air into and out of the lungs, negative pres-sure is required
during inspiration, and an adequate level of pos-itive pressure must be
attained and maintained during expiration. The resting position is one of
inflation. Instead of being an in-voluntary passive act, expiration becomes
active and requires muscular effort. The patient becomes increasingly short of
breath, the chest becomes rigid, and the ribs are fixed at their joints.
In
the centrilobular (centroacinar) form, pathologic changes take place mainly in
the center of the secondary lobule, preserv-ing the peripheral portions of the
acinus. Frequently, there is a derangement of ventilation–perfusion ratios,
producing chronic hypoxemia, hypercapnia (increased CO2
in the arterial blood), polycythemia, and
episodes of right-sided heart failure. Thisleads to central cyanosis,
peripheral edema, and respiratory fail-ure. The patient may receive diuretic
therapy for edema.
Risk Factors
Risk
factors for COPD include environmental exposures and host factors (Chart 24-1).
The most important risk factor for COPD is cigarette smoking. Pipe, cigar, and
other types of to-bacco smoking are also risk factors. In addition, passive
smok-ing contributes to respiratory symptoms and COPD (NIH, 2001). Smoking
depresses the activity of scavenger cells and af-fects the respiratory tract’s
ciliary cleansing mechanism, which keeps breathing passages free of inhaled
irritants, bacteria, and other foreign matter. When smoking damages this
cleansing mechanism, airflow is obstructed and air becomes trapped be-hind the
obstruction. The alveoli greatly distend, diminishing lung capacity. Smoking
also irritates the goblet cells and mucus glands, causing an increased
accumulation of mucus, which in turn produces more irritation, infection, and
damage to the lung. In addition, carbon monoxide (a byproduct of smoking)
com-bines with hemoglobin to form carboxyhemoglobin. Hemoglo-bin that is bound
by carboxyhemoglobin cannot carry oxygen efficiently.
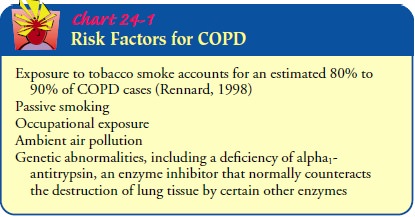
Smoking
is not the only risk factor for COPD. Other factors include prolonged and
intense exposure to occupational dusts and chemicals, indoor air pollution, and
outdoor air pollution, which adds to the total burden of inhaled particles on
the lung (NIH, 2001).
A
host risk factor for COPD is a deficiency of alpha1
anti-trypsin, an enzyme inhibitor that protects the lung parenchyma from
injury. This deficiency predisposes young patients to rapid development of
lobular emphysema even in the absence of smok-ing. Alpha1antitrypsin deficiency
is one of the most common genetically linked lethal diseases among Caucasians
and affects approximately one in every 3,000 Americans or approximately 80,000
to 100,000 cases (George, San Pedro & Stoller, 2000). The genetically
susceptible person is sensitive to environmental factors (smoking, air
pollution, infectious agents, allergens) and in time develops chronic
obstructive symptoms. Carriers of this genetic defect must be identified so
that they can modify envi-ronmental risk factors to delay or prevent overt
symptoms of disease. Genetic counseling should also be offered. Alpha-protease
inhibitor replacement therapy, which slows the progression of the disease, is
available for patients with this genetic defect and for those with severe
disease. This intermittent infusion therapy is costly and is required on an
ongoing basis.
Clinical Manifestations
COPD
is characterized by three primary symptoms: cough, spu-tum production, and
dyspnea on exertion (NIH, 2001). These symptoms often worsen over time. Chronic
cough and sputum production often precede the development of airflow limitation
by many years. However, not all individuals with cough and spu-tum production
will develop COPD. Dyspnea may be severe and often interferes with the
patient’s activities. Weight loss is com-mon because dyspnea interferes with
eating, and the work of breathing is energy-depleting. Often the patient cannot
partici-pate in even mild exercise because of dyspnea; as COPD pro-gresses,
dyspnea occurs even at rest. As the work of breathing increases over time, the
accessory muscles are recruited in an ef-fort to breathe. The patient with COPD
is at risk for respiratory insufficiency and respiratory infections, which in
turn increase the risk for acute and chronic respiratory failure.
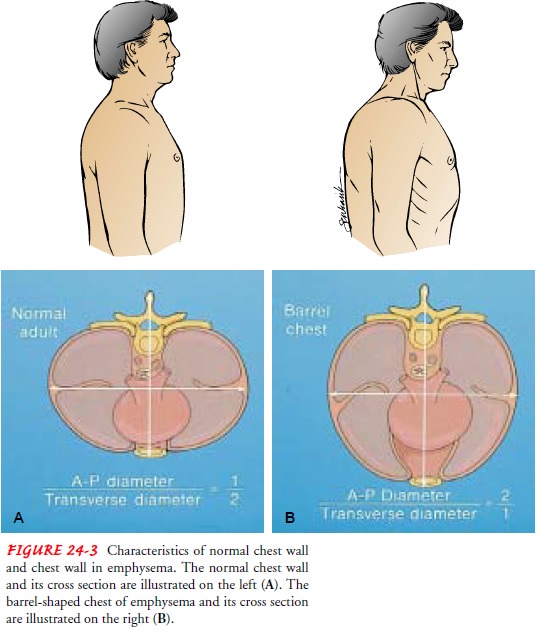
In
COPD patients with a primary emphysematous compo-nent, chronic hyperinflation
leads to the “barrel chest” thorax con-figuration. This results from fixation
of the ribs in the inspiratory position (due to hyperinflation) and from loss
of lung elasticity (Fig. 24-3). Retraction of the supraclavicular fossae occurs
on in-spiration, causing the shoulders to heave upward (Fig. 24-4). In advanced
emphysema, the abdominal muscles also contract on inspiration.

Assessment and Diagnostic Findings
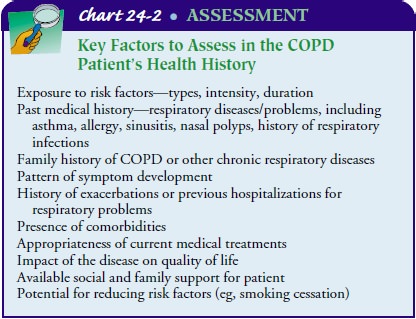
The
nurse should obtain a thorough health history for a patient with known or
potential COPD. Chart 24-2 lists the key factors to assess. Pulmonary function
studies are used to help confirm the diagnosis of COPD, determine disease
severity, and follow dis-ease progression. Spirometry
is used to evaluate airflow obstruc-tion, which is determined by the ratio of
FEV1 (volume of air that the patient can
forcibly exhale in 1 second) to forced vital capac-ity (FVC). Spirometric
results are expressed as an absolute vol-ume and as percent-predicted using
appropriate normal values for gender, age, and height. With obstruction, the
patient either has difficulty exhaling or cannot forcibly exhale air from the
lungs, reducing the FEV1.
Obstructive lung disease is defined as a FEV1/FVC
ratio of less than 70%.
In
addition, bronchodilator reversibility testing may be per-formed to rule out
the diagnosis of asthma and to guide initial treatment. With this type of
testing, spirometry is first obtained, then the patient is given an inhaled
bronchodilator per a proto-col, and finally spirometry is repeated. The patient
demonstrates a degree of reversibility if the pulmonary function values improve
after administration of the bronchodilator.
Arterial
blood gas measurements may also be obtained to as-sess baseline oxygenation and
gas exchange. In addition, a chest x-ray may be obtained to exclude alternative
diagnoses. Lastly, alpha1
antitrypsin deficiency screening may be performed for pa-tients under age 45 or
for those with a strong family history of COPD.
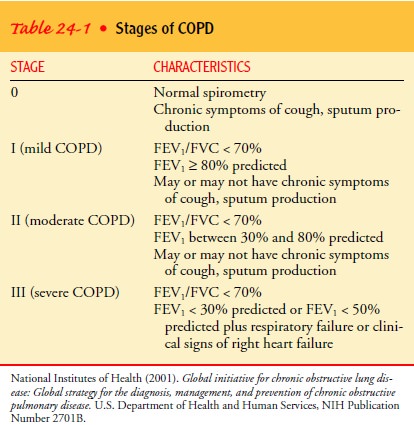
The severity of COPD is classified into four stages (Table 24-1) (National Institutes of Health, 2001). Factors that determine the clinical course and survival of patients with COPD include history of cigarette smoking, passive smoking exposure, age, rate of decline of FEV1, hypoxemia, pulmonary artery pressure, resting heart rate, weight loss, and reversibility of airflow obstruction (George, San Pedro & Stoller, 2000).
In diagnosing COPD, several differential diagnoses must be ruled out. The primary differential diagnosis is asthma. Key characteristics of asthma include onset often early in life, variation in daily symptoms and day-to-day occurrence or timing of symp-toms, family history of asthma, and a largely reversible airflow ob-struction. It may be difficult to differentiate between a patient with COPD and one with chronic asthma. A key part of differ-entiation is the patient history, as well as the patient’s respon siveness to bronchodilators. Other diseases that must be considered in the differential diagnosis include heart failure, bronchiectasis, and tuberculosis (NIH, 2001).
Complications
Respiratory insufficiency and failure are major life-threatening complications of COPD. The acuity of the onset and the sever-ity of respiratory failure depend on the patient’s baseline pul-monary function, pulse oximetry or arterial blood gas values, comorbid conditions, and the severity of other complications of COPD. Respiratory insufficiency and failure may be chronic (with severe COPD) or acute (with severe bronchospasm or pneumonia in the patient with severe COPD). Acute respiratory insufficiency and failure may necessitate ventilatory support until other acute complications, such as infection, can be treated.
Related Topics