Chapter: Medical Surgical Nursing: Management of Patients With Chronic Obstructive Pulmonary Disease
Asthma
Asthma
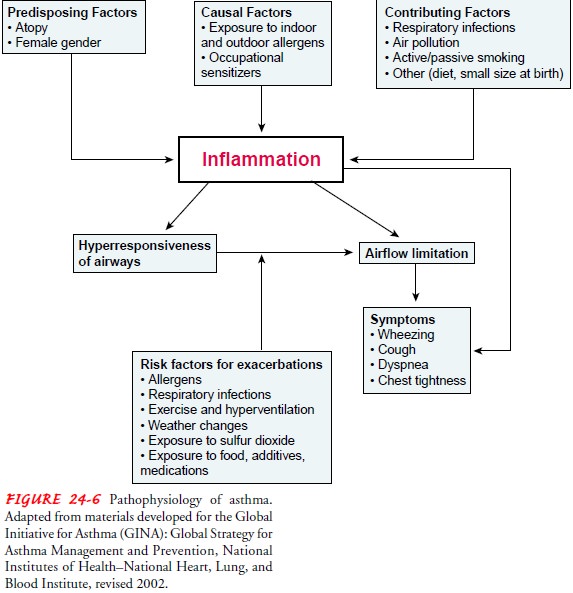
Asthma is a
chronic inflammatory disease of the airways thatcauses airway
hyperresponsiveness, mucosal edema, and mucus production. This inflammation
ultimately leads to recurrent episodes of asthma symptoms: cough, chest
tightness, wheezing, and dyspnea (Fig. 24-6). Estimates show that nearly 17
million Americans have asthma, and more than 5,000 die from this dis-ease
annually (Centers for Disease Control and Prevention [CDC], 1998; CDC, 1999;
NCHS, 2001). In 1998, asthma ac-counted for over 13.9 million outpatient visits
to physician of-fices or hospital clinics and over 2.0 million emergency room
visits (NCHS, 2001).
Asthma
differs from the other obstructive lung diseases in that it is largely
reversible, either spontaneously or with treatment. Pa-tients with asthma may
experience symptom-free periods alter-nating with acute exacerbations, which
last from minutes to hours or days. Asthma can occur at any age and is the most
com-mon chronic disease of childhood. Despite increased knowledge regarding the
pathology of asthma and the development of bet-ter medications and management
plans, the death rate from asthma continues to increase. For most patients it
is a disruptive disease, affecting school and work attendance, occupational
choices, physical activity, and general quality of life.
Allergy is the strongest predisposing factor for asthma. Chronic exposure to airway irritants or allergens also increases the risk for developing asthma. Common allergens can be seasonal (eg, grass, tree, and weed pollens) or perennial (eg, mold, dust, roaches, or animal dander). Common triggers for asthma symptoms and exacerbations in patients with asthma include airway irritants (eg, air pollutants, cold, heat, weather changes, strong odors or perfumes, smoke), exercise, stress or emotional upsets, sinusitis with postnasal drip, medications, viral respiratory tract infections, and gastroesophageal reflux. Most people who have asthma are sensitive to a variety of triggers. A patient’s asthma condition will change depending upon the environment, activities, manage-ment practices, and other factors (NHLBI, 1998).
Pathophysiology
The
underlying pathology in asthma is reversible and diffuse air-way inflammation.
The inflammation leads to obstruction from the following: swelling of the
membranes that line the airways (mucosal edema), reducing the airway diameter;
contraction of the bronchial smooth muscle that encircles the airways
(bron-chospasm), causing further narrowing; and increased mucus pro-duction,
which diminishes airway size and may entirely plug the bronchi.
The
bronchial muscles and mucus glands enlarge; thick, tena-cious sputum is
produced; and the alveoli hyperinflate. Some pa-tients may have airway
subbasement membrane fibrosis. This is called airway “remodeling” and occurs in
response to chronic in-flammation. The fibrotic changes in the airway lead to
airway nar-rowing and potentially irreversible airflow limitation (NIH, 2001;
NHLBI, 1998).
Cells
that play a key role in the inflammation of asthma are mast cells, neutrophils,
eosinophils, and lymphocytes. Mast cells, when activated, release several
chemicals called mediators. These chemicals, which include histamine,
bradykinin, prostaglandins, and leukotrienes, perpetuate the inflammatory
response, causing increased blood flow, vasoconstriction, fluid leak from the
vascu-lature, attraction of white blood cells to the area, and
broncho-constriction (NHLBI, 1998). Regulation of these chemicals is the aim of
much of the current research regarding pharmacologic therapy for asthma.
Further,
alpha- and beta2-adrenergic receptors of the
sympa-thetic nervous system are located in the bronchi. When the
alpha-adrenergic receptors are stimulated, bronchoconstriction occurs; when the
beta2-adrenergic receptors are stimulated, bronchodilation results.
The balance between alpha and beta2 receptors is con-trolled
primarily by cyclic adenosine monophosphate (cAMP). Alpha-adrenergic receptor
stimulation results in a decrease in cAMP, which leads to an increase of
chemical mediators released by the mast cells and bronchoconstriction. Beta2-receptor
stimulation results in increased levels of cAMP, which inhibits the release of
chemical mediators and causes bronchodilation (NHLBI, 1998).
Clinical Manifestations
The
three most common symptoms of asthma are cough, dysp-nea, and wheezing. In some
instances, cough may be the only symptom. Asthma attacks often occur at night
or early in the morning, possibly due to circadian variations that influence
air-way receptor thresholds.
An
asthma exacerbation may begin abruptly but most fre-quently is preceded by
increasing symptoms over the previous few days. There is cough, with or without
mucus production. At times the mucus is so tightly wedged in the narrowed
airway that the patient cannot cough it up. There may be generalized wheez-ing
(the sound of airflow through narrowed airways), first on ex-piration and then
possibly during inspiration as well. Generalized chest tightness and dyspnea
occur. Expiration requires effort and becomes prolonged. As the exacerbation progresses,
diaphoresis, tachycardia, and a widened pulse pressure may occur along with
hypoxemia and central cyanosis (a late sign of poor oxygenation). Although
life-threatening and severe hypoxemia can occur in asthma, it is relatively
uncommon. The hypoxemia is secondary to a ventilation–perfusion mismatch and
readily responds to sup-plemental oxygenation.Symptoms of exercise-induced
asthma include maximal symp-toms during exercise, absence of nocturnal
symptoms, and some-times only a description of a “choking” sensation during
exercise.
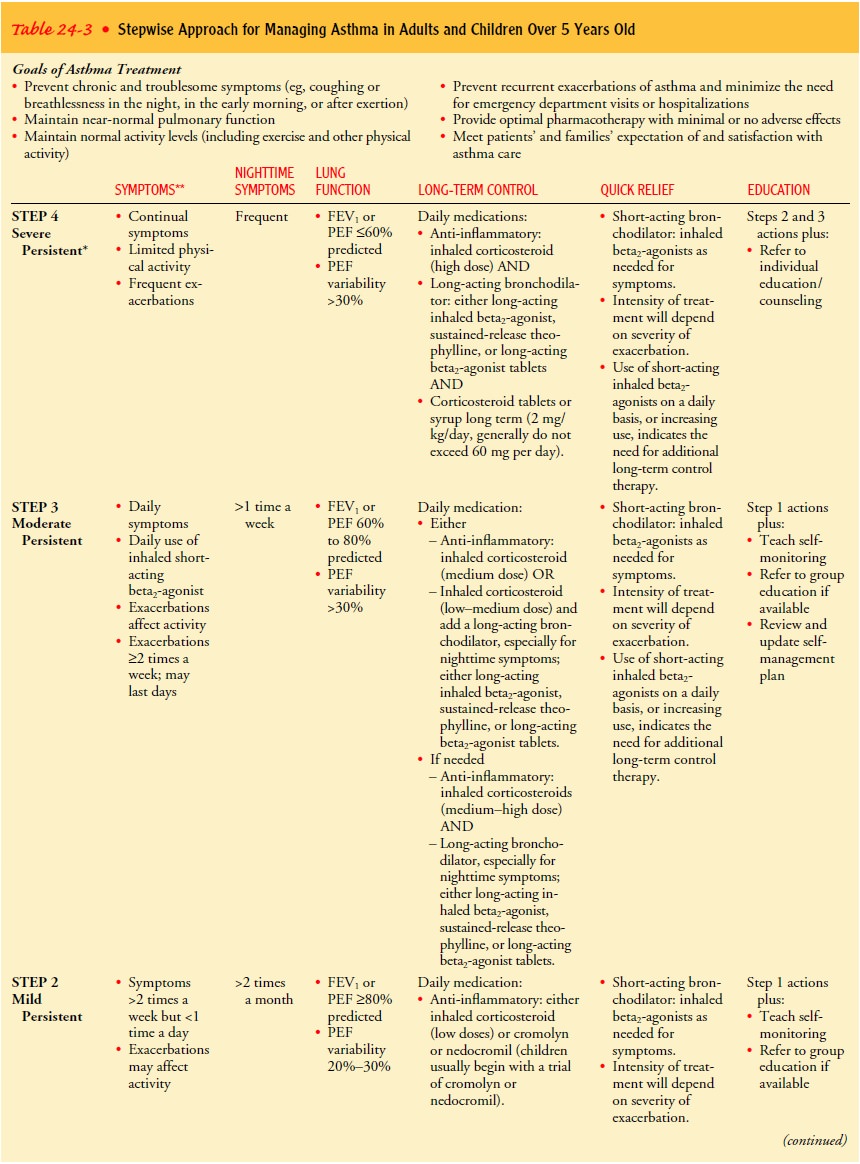
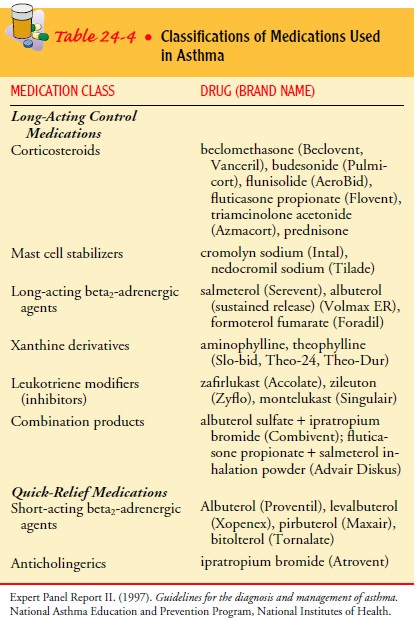
Asthma
is categorized according to symptoms and objective measures of airflow
obstruction (Table 24-3) (Expert Panel Re-port II, 1997).
Assessment and Diagnostic Findings
A
complete family, environmental, and occupational history is es-sential. To
establish the diagnosis, the clinician must determine that periodic symptoms of
airflow obstruction are present, air-flow is at least partially reversible, and
other etiologies have been excluded. A positive family history and
environmental factors, including seasonal changes, high pollen counts, mold,
climate changes (particularly cold air), and air pollution, are primarily
as-sociated with asthma. In addition, asthma is associated with a va-riety of
occupation-related chemicals and compounds, including metal salts, wood and
vegetable dust, medications (eg, aspirin, antibiotics, piperazine, cimetidine),
industrial chemicals and plas-tics, biologic enzymes (eg, laundry detergents),
animal and insect dusts, sera, and secretions. Comorbid conditions that may
ac-company asthma include gastroesophageal reflux, drug-induced asthma, and
allergic bronchopulmonary aspergillosis. Other pos-sible allergic reactions
that may accompany asthma include eczema, rashes, and temporary edema.
During
acute episodes, sputum and blood tests may disclose eosinophilia (elevated
levels of eosinophils). Serum levels of im-munoglobulin E may be elevated if
allergy is present. Arterial blood gas analysis and pulse oximetry reveal
hypoxemia during acute at-tacks. Initially, hypocapnia and respiratory
alkalosis are present. As the condition worsens and the patient becomes more
fatigued, the PaCO2 may rise.
A normal PaCO2 value may be a signal of im-pending
respiratory failure. Because CO2 is 20
times more dif-fusible than oxygen, it is rare for PaCO2
to be normal or elevated in a person who is breathing very rapidly. During an
exacerbation, the FEV1 and FVC
are markedly decreased but improve with bron-chodilator administration
(demonstrating reversibility). Pul-monary function is usually normal between
exacerbations.
The
occurrence of a severe, continuous reaction is referred to as status
asthmaticus and is considered life-threatening (see below).
Prevention
Patients
with recurrent asthma should undergo tests to identify the substances that
precipitate the symptoms. Possible causes are dust, dust mites, roaches,
certain types of cloth, pets, horses, de-tergents, soaps, certain foods, molds,
and pollens. If the attacks are seasonal, pollens can be strongly suspected.
The patient is in-structed to avoid the causative agents whenever possible.
Knowledge
is the key to quality asthma care. Although na-tional guidelines are available
for the care of the asthma patient, unfortunately health care providers may not
follow them. Failure to follow the guidelines in the following areas has been
noted: lack of treatment of patients who have symptoms more than 2 days per
week with a regular medication schedule, lack of patient-specific advice on
improving the environment and an explanation about the importance of doing so,
lack of encouragement for pa-tients to monitor their peak flow measurements
with a diary, and lack of written, up-to-date educational materials (Plaut,
2001).
A
1998 survey by a group called “Asthma in America” found that 11% of physicians
were unaware of the national asthma guidelines. Only 35% of patients with
asthma who were surveyed reported having pulmonary function testing in the past
year.
While
83% of physicians reported prescribing peak flow meter monitoring, only 62% of
patients had ever heard of a peak flow meter (Rickard & Stempel, 1999). All
health care providers caring for asthma patients need to be aware of the
national guidelines and use them (Expert Panel Report II, 1997).
Complications
Complications
of asthma may include status asthmaticus, respira-tory failure, pneumonia, and
atelectasis. Airway obstruction, particularly during acute asthmatic episodes,
often results in hy-poxemia, requiring the administration of oxygen and the
moni-toring of pulse oximetry and arterial blood gases. Fluids are administered
because people with asthma are frequently dehydrated from diaphoresis and
insensible fluid loss with hyperventilation.
Medical Management
Immediate
intervention is necessary because the continuing and progressive dyspnea leads
to increased anxiety, aggravating the situation.
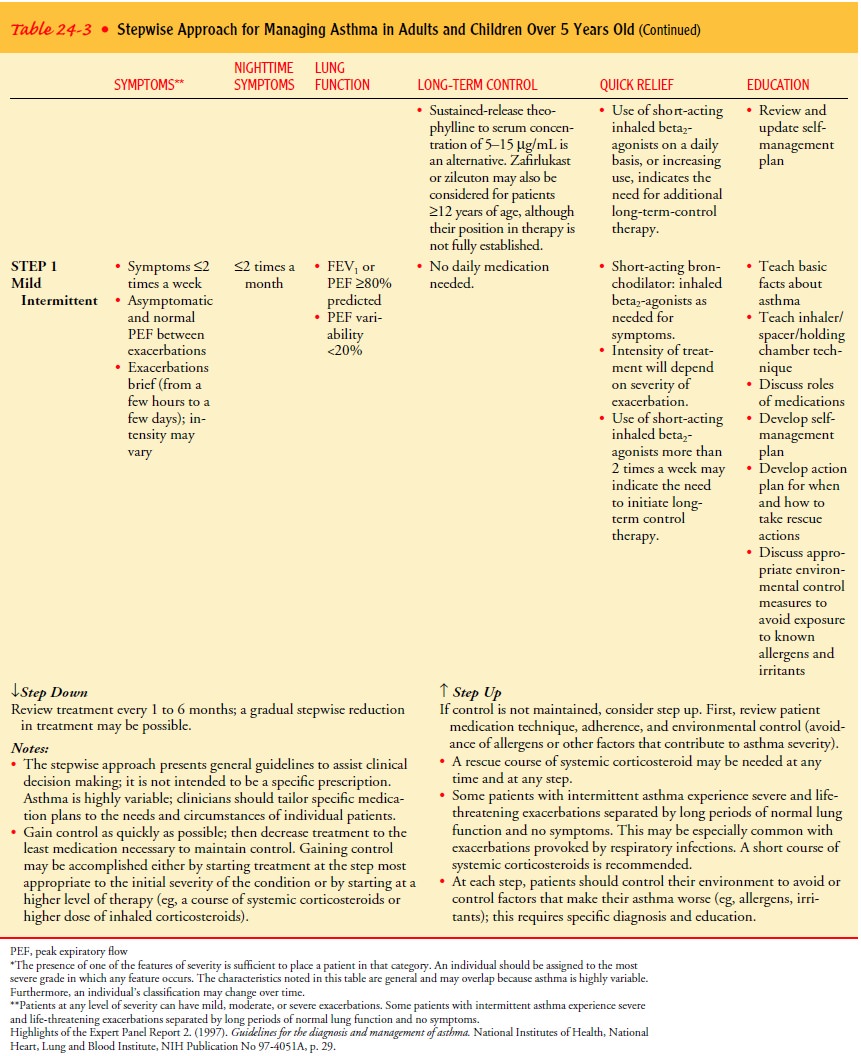
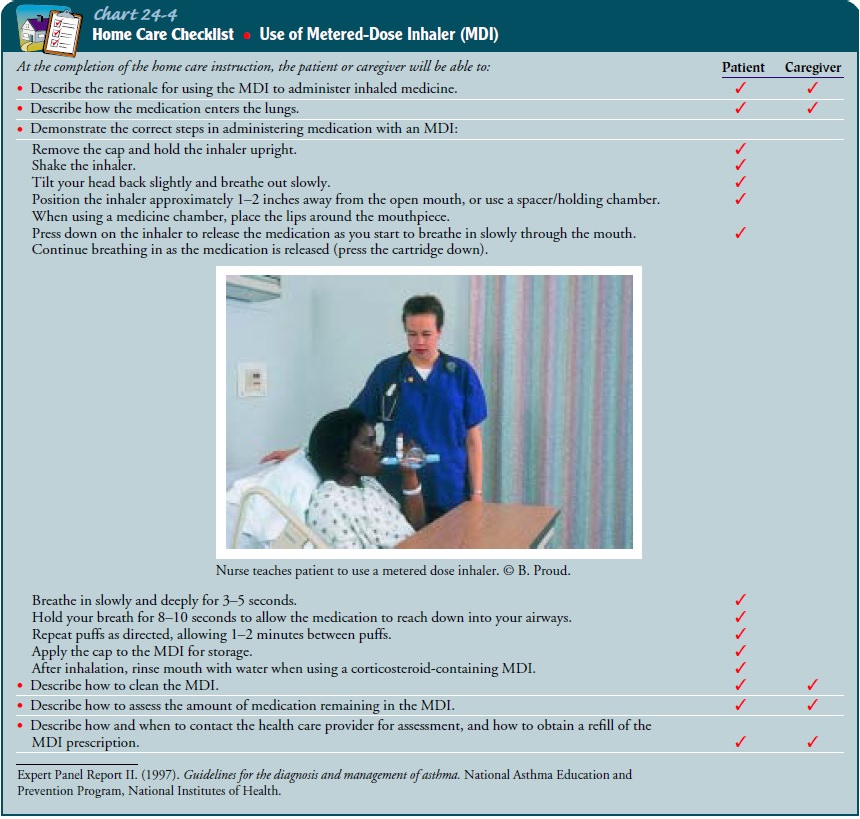
PHARMACOLOGIC THERAPY
Two
general classes of asthma medications are long-acting med-ications to achieve
and maintain control of persistent asthma and quick-relief medications for
immediate treatment of asthma symptoms and exacerbations (Table 24-4). Because
the under-lying pathology of asthma is inflammation, control of persistent
asthma is accomplished primarily with regular use of anti-inflammatory medications.
These medications have systemic side effects when used long term. The route of
choice for administra-tion of these medications is the MDI because it allows
for topical administration. Critical to the success of inhaled therapy is the
proper use of the MDI (see Chart 24-4). If the patient has diffi-culty with
this procedure, the use of a spacer device is indicated. Table 24-3 presents a
stepwise approach for managing asthma (Expert Panel Report II, 1997).
Information on use of the MDI and spacer device is given in the previous
section on COPD.
Long-Acting Control Medications.
Corticosteroids are the mostpotent and effective anti-inflammatory
medications currently available. They are broadly effective in alleviating
symptoms, im-proving airway function, and decreasing peak flow variability.
Initially, the inhaled form is used. A spacer should be used with inhaled
corticosteroids and the patient should rinse the mouth after administration to
prevent thrush, a common complication of inhaled corticosteroid use. A systemic
preparation may be used to gain rapid control of the disease; to manage severe,
persistent asthma; to treat moderate to severe exacerbations; to accelerate
recovery; and to prevent recurrence (Dhand, 2000).
Cromolyn
sodium (Intal) and nedocromil (Tilade) are mild to moderate anti-inflammatory
agents that are used more com-monly in children. They also are effective on a
prophylactic basis to prevent exercise-induced asthma or in unavoidable
exposure to known triggers. These medications are contraindicated in acute
asthma exacerbations.
Long-acting beta2-adrenergic agonists are used with anti-inflammatory medications to control asthma symptoms, partic-ularly those that occur during the night. These agents are also effective for preventing exercise-induced asthma. Long-acting beta2-adrenergic agonists are not indicated for immediate relief of symptoms.
Methylxanthines
(theophylline [Slo-bid, Theo-24, Theo-Dur]) are mild to moderate
bronchodilators usually used in addition to inhaled corticosteroids, mainly for
relief of nighttime asthma symptoms. There is some evidence that theophylline
may have a mild anti-inflammatory effect (NHLBI, 1998).
Leukotriene
modifiers (inhibitors) or antileukotrienes are a new class of medications.
Leukotrienes are potent bronchocon-strictors that also dilate blood vessels and
alter permeability. Leukotriene inhibitors act by either interfering with
leukotriene synthesis or blocking the receptors where leukotrienes exert their
action (Boushey, Fick, Lazarus & Martin, 2000). At this time, they may
provide an alternative to inhaled corticosteroids for mild persistent asthma or
may be added to a regimen of inhaled corticosteroids in more severe asthma to
attain further control.
In
addition, combination products are also available (eg, albuterol/ipratropium
[Combivent]) and offer ease of use for the patient.
Quick-Relief Medications.
Short-acting beta-adrenergic agonistsare the medications of choice
for relieving acute symptoms and preventing exercise-induced asthma. They have
a rapid onset of action. Anticholinergics (eg, ipratropium bromide [Atrovent])
may bring added benefit in severe exacerbations, but they are used more
frequently in COPD patients.
MANAGEMENT OF ASTHMA EXACERBATION
Asthma
exacerbations are best managed by early treatment and education of the patient
(Expert Panel Report II, 1997). Quick-acting beta-adrenergic medications are
first used for prompt relief of airflow obstruction. Systemic corticosteroids
may be nec-essary to decrease airway inflammation in patients who fail to
re-spond to inhaled beta-adrenergic medications. In some patients, oxygen supplementation
may be required to relieve hypoxemia associated with a moderate to severe
exacerbation (Expert Panel Report II, 1997). Also, response to treatment may be
monitored by serial measurements of lung function.
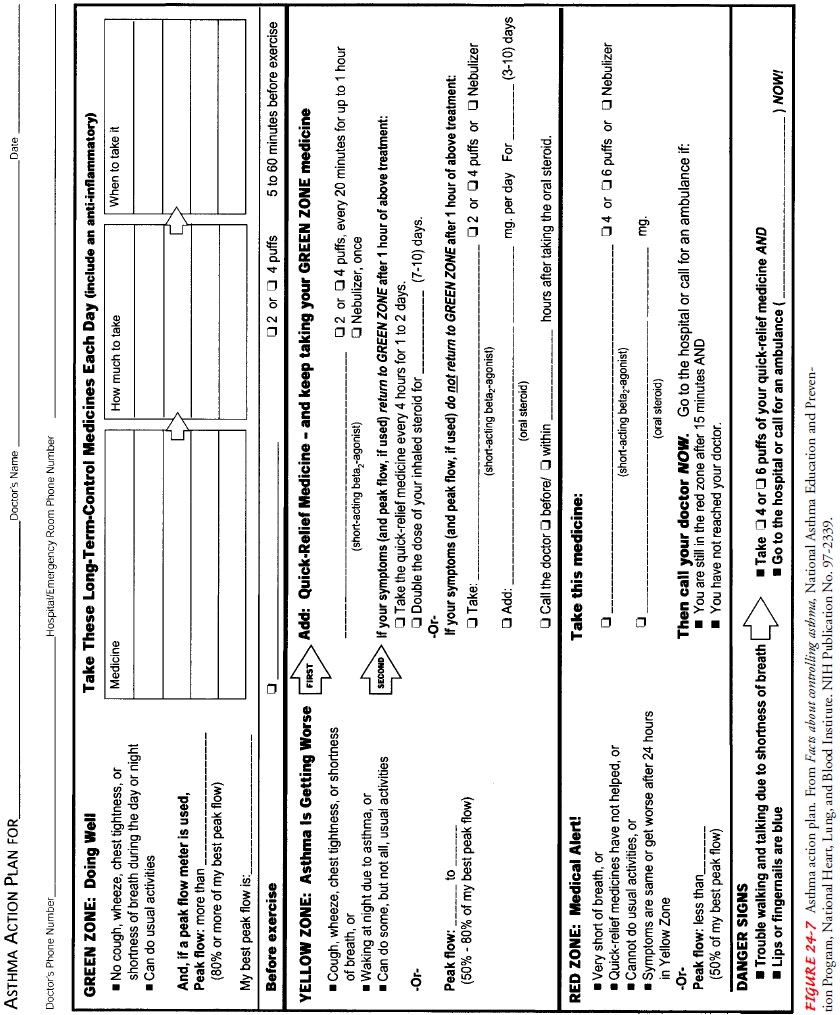
A
written action plan is the most useful tool for the patient (Fig. 24-7). This
helps to guide the patient in self-management strategies regarding an
exacerbation and also provides instruc-tions regarding recognition of early
warning signs of worsening asthma. Patient self-management and early recognition
of prob-lems lead to more efficient communication with health care providers
regarding an asthma exacerbation (Expert Panel Report II, 1997).
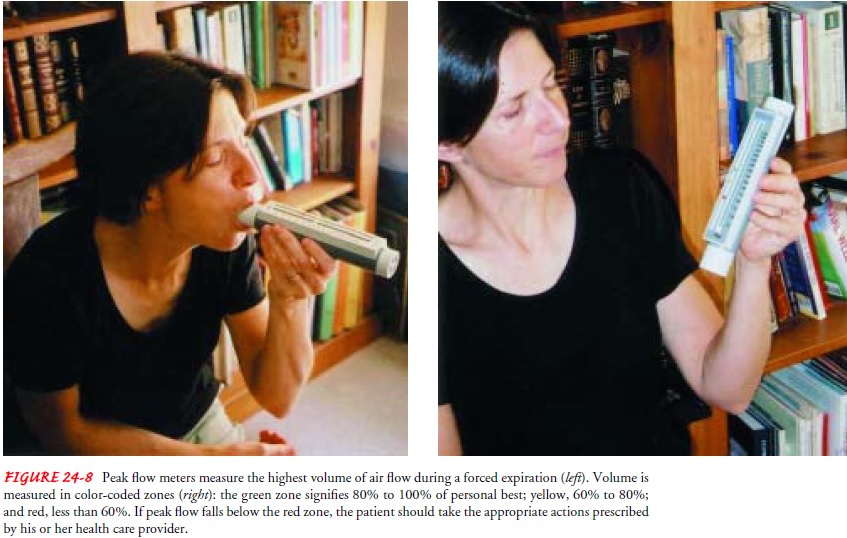
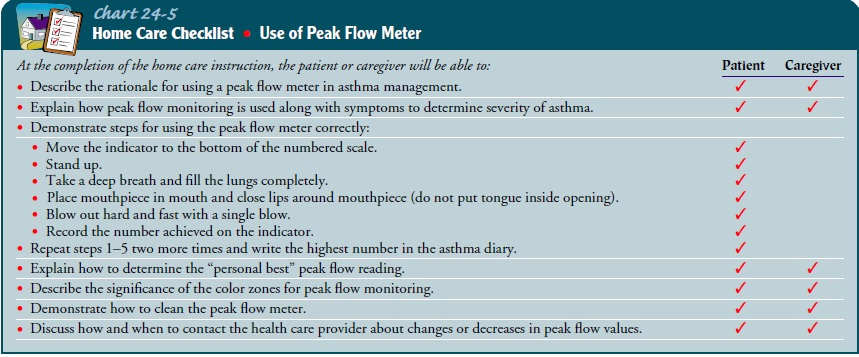
PEAK FLOW MONITORING
Peak
flow meters measure the highest airflow during a forced ex-piration (Fig. 24-8).
Daily peak flow monitoring is recommended for all patients with moderate or
severe asthma because it helps measure asthma severity and, when added to
symptom monitor-ing, indicates the current degree of asthma control. The
patient is instructed in the proper technique, particularly to give maxi-mal
effort. The “personal best” is determined after monitoring peak flows for 2 or
3 weeks after receiving optimal asthma ther-apy. The green (80% to 100% of
personal best), yellow (60% to 80%), and red (less than 60%) zones are
determined, and specific actions are delineated for each zone, enabling the
patient to mon-itor and manipulate his or her own therapy after careful
instruc-tion (Expert Panel Report II, 1997). This reinforces compliance,
independence, and self-efficacy (Reinke, 2000).
Nursing Management
The
immediate nursing care of the patient with asthma depends on the severity of
the symptoms. The patient may be treated suc-cessfully as an outpatient if
asthma symptoms are relatively mild, or he or she may require hospitalization
and intensive care for acute and severe asthma.
The
patient and family are often frightened and anxious be-cause of the patient’s
dyspnea. Thus, an important aspect of care is a calm approach. The nurse
assesses the patient’s respiratory status by monitoring the severity of
symptoms, breath sounds, peak flow, pulse oximetry, and vital signs. The nurse
obtains a history of allergic reactions to medications before administering
medications and identifies the patient’s current use of medica-tions. The nurse
administers medications as prescribed and mon-itors the patient’s responses to
those medications. Fluids may be administered if the patient is dehydrated, and
antibiotic agents may be prescribed if the patient has an underlying
respiratory in-fection. If the patient requires intubation because of acute
respi-ratory failure, the nurse assists with the intubation procedure,
continues close monitoring of the patient, and keeps the patient and family
informed about procedures.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
A major challenge is to implementbasic asthma management principles at the community level (Reinke, 2000). Key issues include education of health care providers, establishment of programs for asthma education (for patients and providers), use of outpatient follow-up care for pa-tients, and a focus on chronic management versus acute episodic care. The nurse is pivotal to achieving all of these objectives.
Patient
teaching is a critical component of care for the patient with asthma (Plaut,
2001). Multiple inhalers, different types of inhalers, antiallergy therapy,
antireflux medications, and avoid-ance measures are all integral for long-term
control. This com-plex therapy requires a patient–provider partnership to
determine the desired outcomes and to formulate a plan to achieve those
outcomes. The patient then carries out daily therapy as part of self-care management,
with input and guidance by the health care provider. Before a partnership can
be established, the patient needs to understand the following:
·
The nature of asthma as a chronic
inflammatory disease
·
The definition of inflammation and
bronchoconstriction
·
The purpose and action of each
medication
·
Triggers to avoid, and how to do so
·
Proper inhalation technique
·
How to perform peak flow monitoring
(Chart 24-5)
·
How to implement an action plan
·
When to seek assistance, and how to
do so
An assortment of excellent educational materials is available from the Expert Panel Report II (1997) and the National Heart, Lung and Blood Institute.
The nurse should obtain current edu-cational materials for
the patient based on the patient’s diagno-sis, causative factors, educational
level, and cultural factors.
Continuing Care.
The
nurse who has contact with the patient inthe hospital, clinic, school, or
office uses the opportunity to as-sess the patient’s respiratory status and
ability to manage self-care to prevent serious exacerbations. The nurse
emphasizes adherence to the prescribed therapy, preventive measures, and the
need to keep follow-up appointments with the primary health care provider. A
home visit to assess the home environment for aller-gens may be indicated for
the patient with recurrent exacerba-tions. The nurse refers the patient to
community support groups. In addition, the nurse reminds the patient and family
about the importance of health promotion strategies and recommended health
screening.
Related Topics