Chapter: Medical Surgical Nursing: Management of Patients With Chronic Obstructive Pulmonary Disease
Chronic Obstructive Pulmonary Disease: Medical and Nursing Management
Medical Management
RISK REDUCTION
Smoking
cessation is the single most effective intervention to prevent COPD or slow its
progression (NIH, 2001). Recent sur-veys indicate that 25% of all American
adults smoke (USPHS, 2000). Nurses play a key role in promoting smoking
cessation and educating patients about ways to do so. Patients diagnosed with
COPD who continue to smoke must be encouraged and as-sisted to quit. Factors
associated with continued smoking vary among patients and may include the
strength of nicotine addic-tion, continued exposure to smoking-associated
stimuli (at work or in social settings), stress, depression, and habit.
Continued smoking is also more prevalent among those with low incomes, a low
level of education, and psychosocial problems (Pohl, 2000).
Because
there are multiple factors associated with continued smoking, successful
cessation often requires multiple strategies. The health care provider should
promote cessation by explaining the risks of smoking and personalizing the
“at-risk” message to the patient. After giving a strong warning about smoking,
the health care provider should work with the patient to set a definite “quit
date.” Referral to a smoking cessation program may be helpful. Follow-up within
3 to 5 days after the quit date to review progress and to address any problems
is associated with an increased rate of success; this should be repeated as
needed. Continued rein-forcement with telephone calls or clinic visits is
extremely bene-ficial. Relapses should be analyzed, and the patient and health
care provider should jointly identify possible solutions to prevent future backsliding.
It is important to emphasize successes rather than failures. First-line
pharmacotherapies that reliably increase long-term smoking abstinence rates are
bupropion SR (Zyban, Wellbutrin), nicotine gum, nicotine inhaler, nicotine
nasal spray, or nicotine patches. Second-line pharmacotherapies include
clonidine (Catapres) and nortriptyline (Aventyl) (USPHS, 2000).
Smoking
cessation can begin in a variety of health care settings— outpatient clinic,
pulmonary rehabilitation, community, hospital, and the patient’s home.
Regardless of the setting, the nurse has the opportunity to teach the patient
about the risks of smoking and the benefits of smoking cessation. A variety of
materials, re-sources, and programs are available to assist with this effort
(eg, Agency for Healthcare Research and Quality [formerly Agency for Healthcare
Policy and Research], United States Public Health Service, Centers for Disease
Control and Prevention, National Cancer Institute, American Lung Association,
American Cancer Society).
PHARMACOLOGIC THERAPY
Bronchodilators.
Bronchodilators
relieve bronchospasm and re-duce airway obstruction by allowing increased
oxygen distribu-tion throughout the lungs and improving alveolar ventilation.
These medications, which are central in the management of COPD (NIH, 2001), are
delivered through a metered-dose inhaler, by nebulization, or via the oral
route in pill or liquid form. Bron-chodilators are often administered regularly
throughout the day as well as on an as-needed basis. They may also be used
prophy-lactically to prevent breathlessness by having the patient use them
before an activity, such as eating or walking.
metered-dose
inhaler (MDI) is a pressurized device con-taining an aerosolized
powder of medication. A precise amount of medication is released with each
activation of the canister (Dhand, 2000). Patients need to be instructed on the
correct use of the device. A spacer (holding chamber) may also be used to
en-hance deposition of the medication in the lung and help the pa-tient coordinate
activation of the MDI with inspiration. Spacers come in several designs, but
all are attached to the MDI and have a mouthpiece on the opposite end (Fig.
24-5). Once the canister is activated, the spacer holds the aerosol in the
chamber until the patient inhales (Dhand, 2000). The patient should take a
slow, 3- to 5-second inhalation immediately following activation of the MDI
(Expert Panel Report II, 1997).
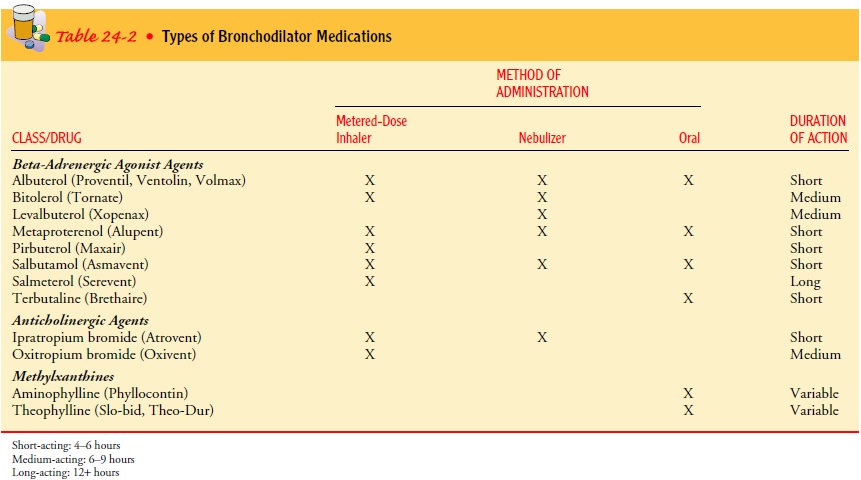
Several
classes of bronchodilators are used: beta-adrenergic agonists, anticholinergic
agents, and methylxanthines. These medications may be used in combination to
optimize the bron-chodilation effect. Some of these medications are
short-acting; others are long-acting. Long-acting bronchodilators are more
con-venient for patient use. Examples of medications in these differ-ing
classes are shown in Table 24-2. Nebulized medications (nebulization of
medication via an air compressor) may also be effective in patients who cannot
use an MDI properly or who pre-fer this method of administration.
Corticosteroids.
Inhaled
and systemic corticosteroids (oral orintravenous) may also be used in COPD but
are used more fre-quently in asthma. Although it has been shown that
cortico-steroids do not slow the decline in lung function, these medications
may improve symptoms. A short trial course of oral cortico-steroids may be
prescribed for patients with stage II or III COPD to see if pulmonary function
improves and symptoms decrease. Inhaled corticosteroids via MDI may also be
used. Examples of corticosteroids in the inhaled form are beclomethasone
(Beclovent, Vanceril), budesonide (Pulmicort), flunisolide (AeroBid),
fluti-casone (Flovent), and triamcinolone (Azmacort).
Medication regimens used to manage COPD are based on disease severity. For stage I or mild COPD, a short-acting bron chodilator may be prescribed. For stage II or moderate COPD, one or more bronchodilators may be prescribed along with in-haled corticosteroids, if symptoms are significant. For stage III or severe COPD, medication therapy includes regular treatment with one or more bronchodilators and inhaled corticosteroids (NIH, 2001).
Other Medications.
Patients
should receive a yearly influenzavaccine and the pneumococcal vaccine every 5
to 7 years as pre-ventive measures. In most healthy adults, pneumococcal
vaccine titers persist for 5 or more years (George, San Pedro & Stoller,
2000). Other pharmacologic treatments that may be used in COPD include alpha1 antitrypsin augmentation therapy, anti-biotic
agents, mucolytic agents, and antitussive agents.
MANAGEMENT OF EXACERBATION
An
exacerbation of COPD is difficult to diagnose, but signs and symptoms may
include increased dyspnea, increased sputum pro-duction and purulence,
respiratory failure, changes in mental sta-tus, or worsening blood gas
abnormalities. Primary causes for an acute exacerbation include
tracheobronchial infection and air pollution (NIH, 2001). Secondary causes are
pneumonia; pul-monary embolism; pneumothorax; rib fractures or chest trauma;
inappropriate use of sedative, opioid, or beta-blocking agents; and right- or
left-sided heart failure. First, the primary cause of the exacerbation is
identified, and then specific treatment is ad-ministered. Optimization of
bronchodilator medications is the first-line therapy and involves identifying
the best medication or combinations of medications taken on a regular schedule
for that patient. Depending on the signs and symptoms, corticosteroids,
antibiotic agents, oxygen therapy, and intensive respiratory in-terventions may
also be used. Indications for hospitalization of a patient with an acute
exacerbation of COPD include severe dys-pnea that does not respond adequately
to initial therapy, confusion or lethargy, respiratory muscle fatigue, paradoxical
chest wall movement, peripheral edema, worsening or new onset of central
cyanosis, persistent or worsening hypoxemia, and/or need for noninvasive or
invasive assisted mechanical ventilation (Celli, Snider, Heffner et al., 1995;
NIH, 2001).
OXYGEN THERAPY
Oxygen therapy can be administered as long-term continuous therapy, during exercise, or to prevent acute dyspnea. Long-term oxygen therapy has been shown to improve the patient’s quality of life and survival (NIH, 2001). For patients with an arterial oxygen pressure (PaO2) of 55 mm Hg or less on room air, maintaining a constant and adequate oxygen saturation (>90%) is associated with significantly reduced mortality and improved quality of life. Indications for oxygen supplementa-tion include a PaO2 of 55 mm Hg or less or evidence of tissue hypoxia and organ damage such as cor pulmonale, secondary polycythemia, edema from right heart failure, or impaired men-tal status. In patients with exercise-induced hypoxemia, oxygen supplementation during exercise can improve performance. Pa-tients who are hypoxemic while awake are likely to be so during sleep. Therefore, nighttime oxygen therapy is recommended as well, and the prescription for oxygen therapy is for continuous, 24-hour use. Intermittent oxygen therapy is indicated for those who desaturate only during exercise or sleep.
SURGICAL MANAGEMENT
Bullectomy.
A
bullectomy is a surgical option for select patientswith bullous emphysema.
Bullae are enlarged airspaces that do not contribute to ventilation but occupy
space in the thorax; these areas may be surgically excised. Many times these
bullae compress areas of the lung that do have adequate gas exchange.
Bullectomy may help reduce dyspnea and improve lung function. It can be done
thoracoscopically (with a video-assisted thoraco-scope) or via a limited
thoracotomy incision.
Lung Volume Reduction Surgery.
Treatment options for patientswith end-stage COPD (stage III) with
a primary emphysematous component are limited, although lung volume reduction
surgery is an option for a specific subset of patients. This subset includes
patients with homogenous disease or disease that is focused in one area and not
widespread throughout the lungs. Lung volume re-duction surgery involves the
removal of a portion of the diseased lung parenchyma. This allows the
functional tissue to expand, re-sulting in improved elastic recoil of the lung
and improved chest wall and diaphragmatic mechanics. This type of surgery does
not cure the disease, but it may decrease dyspnea, improve lung func-tion, and
improve the patient’s overall quality of life. Careful se-lection of patients
for this procedure is essential to decrease the morbidity and mortality. The
long-term outcomes of this surgery are unknown.
The
National Emphysema Treatment Trial (NETT) is a large, multicenter randomized
clinical trial that began in 1997 and is ongoing. It is attempting to answer
many questions regarding the risks and benefits of lung volume reduction
surgery in the treat-ment of severe emphysema. All patients in this trial
receive a 6-to 10-week pulmonary rehabilitation program and comprehen-sive
medical management. Following completion of pulmonary rehabilitation, patients
are randomized to continue medical man-agement or undergo lung volume reduction
surgery. The results of this trial will help to determine the role of lung
volume reduc-tion surgery for patients with severe emphysema (NIH, 2001). It is
expected that 2,500 patients will be entered into the study.
Lung Transplantation.
Lung
transplantation is a viable alterna-tive for definitive surgical treatment of
end-stage emphysema. It has been shown to improve quality of life and
functional capac-ity (NIH, 2001). Specific criteria exist for referral for lung
trans-plantation; however, organs are in short supply and many patients die
while waiting for a transplant.
PULMONARY REHABILITATION
Pulmonary
rehabilitation for patients with COPD is well estab-lished and widely accepted
as a means to alleviate symptoms and optimize functional status. In both
randomized and nonrandom-ized clinical trials, pulmonary rehabilitation has
been shown to improve exercise tolerance, reduce dyspnea, and increase
health-related quality of life (Rochester, 2000). The primary goal of
re-habilitation is to restore patients to the highest level of independent
function possible and to improve their quality of life. A suc-cessful
rehabilitation program is individualized for each patient, is
multidisciplinary, and attends to both the physiologic and emotional needs of
the patient. Most pulmonary rehabilitation programs include educational,
psychosocial, behavioral, and physical components. Breathing exercises and
retraining and ex-ercise programs are used to improve functional status, and
the pa-tient is taught methods to alleviate symptoms.
Pulmonary
rehabilitation may be used therapeutically in other diseases besides COPD,
including asthma, cystic fibrosis, lung cancer, interstitial lung disease,
thoracic surgery, and lung trans-plantation. It may be conducted in the
inpatient, outpatient, or home setting; the lengths of programs vary. Selection
of a program depends upon the patient’s physical, functional, and psychosocial
status; insurance coverage; changing health care trends; availabil-ity of
programs; and patient preference (Rochester, 2000).
Nursing Management
The
nurse plays a key role in identifying potential candidates for pulmonary
rehabilitation and in facilitating and reinforcing the material learned in the
rehabilitation program. Not all patients have access to a formal rehabilitation
program. However, the nurse can be instrumental in teaching the patient and
family as well as facilitating specific services for the patient (eg,
respiratory therapy education, physical therapy for exercise and breathing
re-training, occupational therapy for conserving energy during ac-tivities of
daily living, and nutritional counseling). In addition, numerous educational
materials are available to assist the nurse in teaching patients with COPD.
Potential resources include the American Lung Association, the American
Association of Cardio-vascular and Pulmonary Rehabilitation, the American
Thoracic Society, the American College of Chest Physicians, and the Amer-ican
Association for Respiratory Therapy.
PATIENT EDUCATION
Patient
education is a major component of pulmonary rehabili-tation and includes a
broad variety of topics. Depending on the length and setting of the program,
topics may include normal anatomy and physiology of the lung, pathophysiology
and changes with COPD, medications and home oxygen therapy, nutrition,
respiratory therapy treatments, symptom alleviation, smoking cessation,
sexuality and COPD, coping with chronic disease, communicating with the health
care team, and planning for the future (advance directives, living wills,
informed decision making about health care alternatives).
Breathing Exercises.
The
breathing pattern of most people withCOPD is shallow, rapid, and inefficient;
the more severe the dis-ease, the more inefficient the breathing pattern. With
practice, this type of upper chest breathing can be changed to diaphrag-matic
breathing, which reduces the respiratory rate, increases alveolar ventilation,
and sometimes helps expel as much air as possible during expiration. Pursed-lip
breathing helps to slow expiration, prevents collapse of small airways, and
helps the patient to control the rate and depth of res-piration. It also
promotes relaxation, enabling the patient to gain control of dyspnea and reduce
feelings of panic.
Inspiratory Muscle Training.
Once the patient masters dia-phragmatic breathing, a program of
inspiratory muscle training may be prescribed to help strengthen the muscles
used in breath-ing. This program requires that the patient breathe against
resis-tance for 10 to 15 minutes every day. As the resistance is gradually
increased, the muscles become better conditioned. Conditioning of the
respiratory muscles takes time, and the patient is instructed to continue
practicing at home (Larson, Covey, Wirtz et al., 1999; NIH, 2001).
Activity Pacing.
A
patient with COPD has decreased exercisetolerance during specific periods of
the day. This is especially true on arising in the morning, because bronchial
secretions collect in the lungs during the night while the person is lying
down. The patient may have difficulty bathing or dressing. Activities
requir-ing the arms to be supported above the level of the thorax may produce
fatigue or respiratory distress but may be tolerated bet-ter after the patient
has been up and moving around for an hour or more. Working with the nurse, the
patient can reduce these limitations by planning self-care
activities and determining the best time for bathing, dressing, and daily
activities.
Self-Care Activities.
As
gas exchange, airway clearance, and thebreathing pattern improve, the patient
is encouraged to assume increasing participation in self-care activities. The
patient is taught to coordinate diaphragmatic breathing with activities such as
walking, bathing, bending, or climbing stairs. The patient should bathe, dress,
and take short walks, resting as needed to avoid fa-tigue and excessive
dyspnea. Fluids should always be readily avail-able, and the patient should
begin to drink fluids without having to be reminded. If postural drainage is to
be done at home, the nurse instructs and supervises the patient before
discharge or in the outpatient setting.
Physical Conditioning.
Physical conditioning techniques in-clude breathing exercises and
general exercises intended to con-serve energy and increase pulmonary
ventilation. There is a close relationship between physical fitness and
respiratory fit-ness. Graded exercises and physical conditioning programs using
treadmills, stationary bicycles, and measured level walks can improve symptoms
and increase work capacity and exercise tolerance. Any physical activity that
can be done regularly is helpful. Lightweight portable oxygen systems are
available for ambulatory patients who require oxygen therapy during physi-cal
activity.
Oxygen Therapy.
Oxygen
supplied to the home comes in com-pressed gas, liquid, or concentrator systems.
Portable oxygen sys-tems allow the patient to exercise, work, and travel. To
help the patient adhere to the oxygen prescription, the nurse explains the proper
flow rate and required number of hours for oxygen use as well as the dangers of
arbitrary changes in flow rates or duration of therapy. The nurse cautions the
patient that smoking with or near oxygen is extremely dangerous. The nurse also
reassures the patient that oxygen is not “addictive” and explains the need for
regular evaluations of blood oxygenation by pulse oximetry or arterial blood
gas analysis.
Nutritional Therapy.
Nutritional
assessment and counseling areimportant aspects in the rehabilitation process
for the patient with COPD. Approximately 25% of patients with COPD are
undernourished (NIH, 2001; Ferreira, Brooks, Lacasse & Gold-stein, 2001). A
thorough assessment of caloric needs and coun-seling about meal planning and
supplementation are part of the rehabilitation process.
Coping Measures.
Any
factor that interferes with normal breath-ing quite naturally induces anxiety,
depression, and changes in behavior. Many patients find the slightest exertion
exhausting. Constant shortness of breath and fatigue may make the patient
irritable and apprehensive to the point of panic. Restricted activ-ity (and
reversal of family roles due to loss of employment), the frustration of having
to work to breathe, and the realization that the disease is prolonged and
unrelenting may cause the patient to react with anger, depression, and
demanding behavior. Sexual function may be compromised, which also diminishes
self-esteem. In addition, the nurse needs to provide education and support to
the spouse/significant other and family because the caregiver role in end-stage
COPD can be difficult.
Related Topics