Chapter: Modern Pharmacology with Clinical Applications: Antiinflammatory and Antirheumatic Drugs
Nonsteroidal Antiinflammatory Drugs
NONSTEROIDAL
ANTIINFLAMMATORY DRUGS
The nonsteroidal anti-inflammatory drugs (NSAIDs) have a variety of
clinical uses as antipyretics, analgesics, and anti-inflammatory agents. They reduce body tem-perature
in febrile states and thus are effective an-tipyretics. They are also useful as
analgesics, relieving mild to moderate pain
such as myalgia, dental pain, dysmenorrhea, and headache. Unlike the
opioid analgesics, they do not cause neurological de-pression or dependence. As
anti-inflammatory agents, NSAIDs are used to treat conditions such as muscle
strain, tendinitis, and bursitis. They are also used to treat the chronic pain
and inflammation of rheumatoid arthritis (adult onset and juvenile),
osteoarthritis, and arthritic variants such as gouty arthritis and ankylosing
spondylitis. While NSAIDs used to be the sole agent of choice for mild to
moderate rheumatoid disease, they are now frequently used in conjunction with
the disease-modifying antirheumatic drugs
(DMARDs) early in the treatment of these disorders. This is
because the NSAIDs reduce pain and
inflammation associated with rheumatoid diseases but do not delay or reverse
the dis-ease’s progress.
Mechanism of Action
The anti-inflammatory actions of the NSAIDs are most likely
explained by their inhibition of prostaglandin syn-thesis by COX-2. The COX-2 isoform is the
predomi-nant COX involved in the production of prostaglandins during
inflammatory processes. Prostaglandins of the E and F series evoke some of the
local and systemic man-ifestations of inflammation, such as vasodilation, hyper-emia,
increased vascular permeability, swelling, pain, and increased leukocyte
migration. In addition, they in-tensify the effects of inflammatory mediators,
such as histamine, bradykinin, and 5-hydroxytryptamine. All NSAIDs except the
COX-2-selective agents inhibit both COX isoforms; the degree of inhibition of
COX-1 varies from drug to drug. No one
NSAID is empirically superior for the
treatment of inflammatory diseases; in-stead, each individual’s response to and
tolerance of a drug determines its therapeutic utility.
Adverse Effects
A number of the toxicities
commonly caused by the NSAIDs result from the inhibition of prostaglandin
synthesis (Table 36.2). The ability of
NSAIDs to increase gastric acid
secretion and inhibit blood clotting can lead to GI toxicity. Mild
reactions, such as heartburn and in-digestion, may be decreased by adjusting
the dosage, us-ing antacids, or administering the drugs after meals. Occult
loss of blood from the GI tract and iron defi-ciency anemia are also possible.
More serious toxicity can result from prolonged NSAID therapy, including peptic
ulceration and rarely, GI hemorrhage.
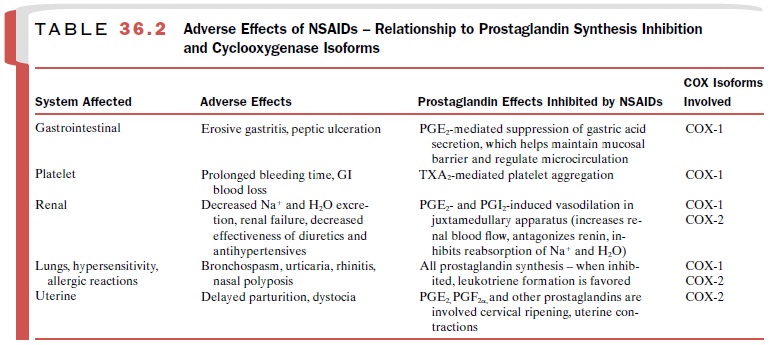
NSAIDs can impair renal function, cause fluid reten-tion, and
provoke hypersensitivity reactions, including
bronchospasm, aggravation of asthma, urticaria, nasal polyps, and rarely,
anaphylactoid reactions. These reac-tions may occur even in those who have
previously used NSAIDs without any ill effects. NSAIDs inhibit uterine
contraction and can cause premature closure of the fe-tal ductus arteriosus.
The spectrum of toxicity
produced by each NSAID is related to its inhibition of specific COX isoforms.
The earliest NSAIDs inhibit both isoforms of COX. Certain of these drugs are
more specific for COX-1, whereas oth-ers inhibit COX-1 and COX-2 with roughly
equal po-tency. More recently developed
drugs selectively inhibit COX-2 and
therefore do not elicit the GI and antiplatelet side effects common to drugs
that inhibit COX-1.
Adverse effects that are not
unequivocally related to inhibition of prostaglandin synthesis include hepatic
effects (hepatitis, hepatic necrosis, cholestatic jaundice, increased serum
aminotransferases), dermal effects (photosensitivities, Stevens-Johnson
syndrome, toxic epidermal necrolysis, onycholysis), central nervous sys-tem
(CNS) effects (headaches, dizziness, tinnitus, deaf-ness, drowsiness,
confusion, nervousness, increased sweating, aseptic meningitis), ocular effects
(toxic am-blyopia, retinal disturbances), and certain renal effects (acute
interstitial nephritis, acute papillary necrosis).
Contraindications and Drug Interactions
Co-morbid factors that increase the risk of NSAID-induced GI bleeding include history of ulcer disease, advanced age, poor health status, treatment with certain drugs (discussed later), long duration of NSAID ther-apy, smoking, and heavy alcohol use. Because of their renal effects, NSAIDs must be used with caution in patients with renal impairment, heart failure, hyperten-sion, and edema.
The use of NSAIDs is
contraindicated in persons who have had a hypersensitivity reaction to
salicylates or any other NSAID. Asthmatics are at par-ticular risk for these
reactions. NSAIDs should be used during pregnancy only if the potential benefit
justifies the risk to the fetus.
A significant number of drug
interactions are com-mon to most of the NSAIDs. The likelihood of NSAID-induced
GI toxicity is increased by concomitant treat-ment with corticosteroids (long
term), other NSAIDs, bisphosphonates, or anticoagulants. Certain NSAIDs can
also compete for protein binding sites with war-farin, compounding the risk of
GI bleeding if these drugs are coprescribed. Agents that cause
thrombocy-topenia (e.g., myelosuppressive antineoplastic drugs) can also
increase the likelihood that NSAIDs will cause bleeding. NSAIDs can decrease
the clearance of methotrexate, resulting in severe hematological and GI
toxicity. This does not appear to be a significant problem with low-dose
methotrexate used in the treatment of rheumatoid arthritis; however, higher
methotrexate doses used in the treatment of psoriasis or cancer may produce
this toxicity. NSAIDs, when used in conjunc-tion with immunosuppressive agents,
can mask fever and other signs of infection.
Because NSAIDs decrease
prostaglandin synthesis in the kidney, these drugs can increase the nephrotox- icity
of agents such as aminoglycosides, amphotericin B, cidofovir, cisplatin,
cyclosporine, foscarnet, ganci-clovir, pentamidine, and vancomycin. NSAIDs can
de-crease the renal excretion of drugs such as lithium. NSAIDs can decrease the
effectiveness of antihyper-tensive drugs such as β-blockers and diuretics. The
eld-erly and those with decreased renal function are at particular risk for
this interaction. Elevated hepatic enzymes and hepatic toxicity can occur with
some drugs.
Related Topics