Chapter: Clinical Anesthesiology: Anesthetic Equipment & Monitors : Cardiovascular Monitoring
Noninvasive Arterial Blood Pressure Monitoring Indications
Noninvasive
Arterial Blood Pressure Monitoring Indications
The use of any anesthetic, no matter how
“trivial,” is an indication for arterial blood pressure measure-ment. The
techniques and frequency of pressure determination depend on the patient’s
condition and the type of surgical procedure. An oscillometric blood pressure
measurement every 3–5 min is ade-quate in most cases.
Contraindications
Although some method of blood pressure
measure-ment is mandatory, techniques that rely on a blood pressure cuff are
best avoided in extremities with vascular abnormalities (eg, dialysis shunts)
or with intravenous lines. Rarely, it may prove impossible to monitor blood
pressure in cases (eg, burns) in which there may be no accessible site from
which the blood pressure can be safely recorded.
Techniques & Complications
A. Palpation
SBP can be determined by (1) locating a
palpable peripheral pulse, (2) inflating a blood pressure cuff proximal to the
pulse until flow is occluded, (3) releasing cuff pressure by 2 or 3 mm Hg per
heart-beat, and (4) measuring the cuff pressure at which pulsations are again
palpable. This method tends to underestimate systolic pressure, however,
because of the insensitivity of touch and the delay between flow under the cuff
and distal pulsations. Palpation does not provide a diastolic pressure or MAP.
The equip-ment required is simple and inexpensive.
B. Doppler Probe
When a Doppler probe is substituted for
the anesthesiologist’s finger, arterial blood pressure
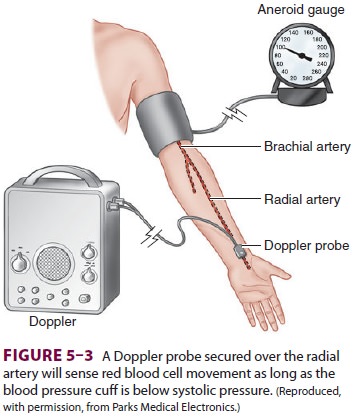
measurement becomes sensitive enough to
be useful in obese patients, pediatric patients, and patients in shock (Figure 5–3).
The Doppler effect is the shift in
the frequency of sound waves when their source moves relative to the observer.
For example, the pitch of a train’s whistle increases as a train approaches and
decreases as it departs. Similarly, the reflection of sound waves off of a
moving object causes a fre-quency shift. A Doppler probe transmits an
ultra-sonic signal that is reflected by underlying tissue. As red blood cells
move through an artery, a Doppler frequency shift will be detected by the
probe. The dif-ference between transmitted and received frequency causes the
characteristic swishing sound, which indicates blood flow. Because air reflects
ultrasound, a coupling gel (but not
corrosive electrode jelly) is applied between the probe and the skin.
Positioning the probe directly above an artery is crucial, since the beam must
pass through the vessel wall. Interference from probe movement or
electrocautery is an annoy-ing distraction. Note that only systolic pressures
can be reliably determined with the Doppler technique.
A variation of Doppler technology uses a piezo-electric crystal to detect lateral arterial wall move-ment to the intermittent opening and closing of vessels between systolic and diastolic pressure. This instrument thus detects both systolic and diastolic pressures. The Doppler effect is routinely employed by perioperative echocardiographers to discern both the directionality and velocity of both blood flow within the heart and the movement of the heart’s muscle tissue (tissue Doppler).
C. Auscultation
Inflation of a blood pressure cuff to a
pressure between systolic and diastolic pressures will par-tially collapse an
underlying artery, producing tur-bulent flow and the characteristic Korotkoff
sounds. These sounds are audible through a stethoscope placed under—or just
distal to—the distal third of the blood pressure cuff. The clinician measures
pres-sure with an aneroid or mercury manometer.
Occasionally, Korotkoff sounds cannot be
heard through part of the range from systolic to diastolic pressure. This
auscultatory gap is most common in hypertensive patients and can lead to an
inaccurate diastolic pressure measurement. Korotkoff sounds are often difficult
to auscultate during episodes of hypotension or marked periph-eral
vasoconstriction. In these situations, the sub-sonic frequencies associated
with the sounds can be detected by a microphone and amplified to indicate
systolic and diastolic pressures. Motion artifact and electrocautery
interference limit the usefulness of this method.
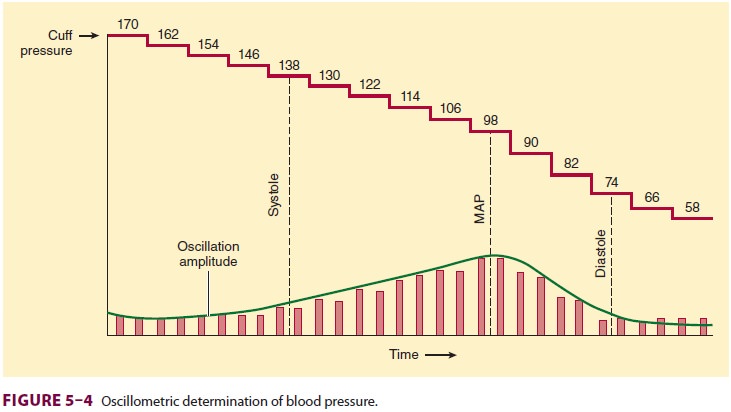
D. Oscillometry
Arterial pulsations cause oscillations
in cuff pres-sure. These oscillations are small if the cuff is inflated above
systolic pressure. When the cuff pressure decreases to systolic pressure, the
pulsa-tions are transmitted to the entire cuff, and the oscillations markedly
increase. Maximal oscilla-tion occurs at the MAP, after which oscillations
decrease. Because some oscillations are present above and below arterial blood
pressure, a mer-cury or aneroid manometer provides an inaccurate and unreliable
measurement. Automated blood pressure monitors electronically measure the
pres-sures at which the oscillation amplitudes change (Figure 5–4). A microprocessor
derives systolic, mean, and diastolic pressures using an algorithm. Machines
that require identical consecutive pulse waves for measurement confirmation may
be unre-liable during arrhythmias (eg, atrial fibrillation). Oscillometric
monitors should not be used on patients on cardiopulmonary bypass. Nonetheless,
the speed, accuracy, and versatility of oscillomet-ric devices have greatly
improved, and they have become the preferred noninvasive blood pressure
monitors in the United States and worldwide.
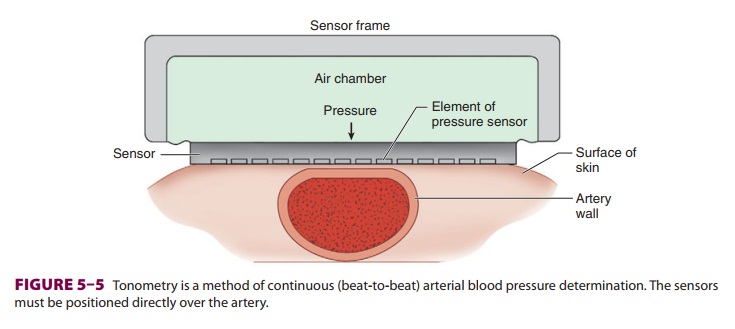
E. Arterial Tonometry
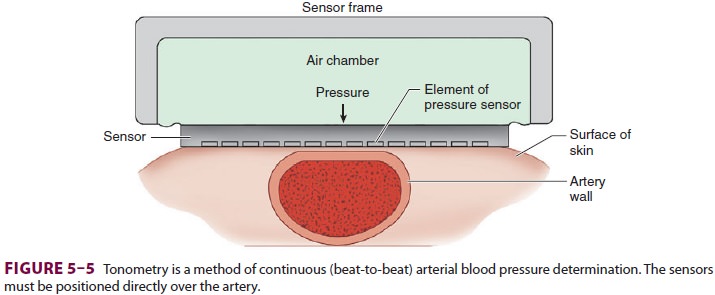
Arterial tonometry measures beat-to-beat
arterial blood pressure by sensing the pressure required to partially flatten a
superficial artery that is supported by a bony structure (eg, radial artery). A
tonometer consisting of several independent pressure trans-ducers is applied to
the skin overlying the artery (Figure 5–5). The contact stress between the
trans-ducer directly over the artery and the skin reflects intraluminal
pressure. Continuous pulse recordings produce a tracing very similar to an
invasive arterial blood pressure waveform. Limitations to this tech-nology
include sensitivity to movement artifact and the need for frequent calibration.
Clinical Considerations
Adequate oxygen delivery to vital organs must be maintained during anesthesia. Unfortunately, instruments to monitor specific organ perfusion and oxygenation are complex, expensive, and often unreliable, and, for that reason, an adequate arterial blood pressure is assumed to predict adequate organ blood flow. However, flow also depends on vascular resistance:
Even if the pressure is high, when the
resistance is also high, flow can be low. T hus, arterial blood pressure should
be viewed as an indicator—but not a measure—of organ perfusion.
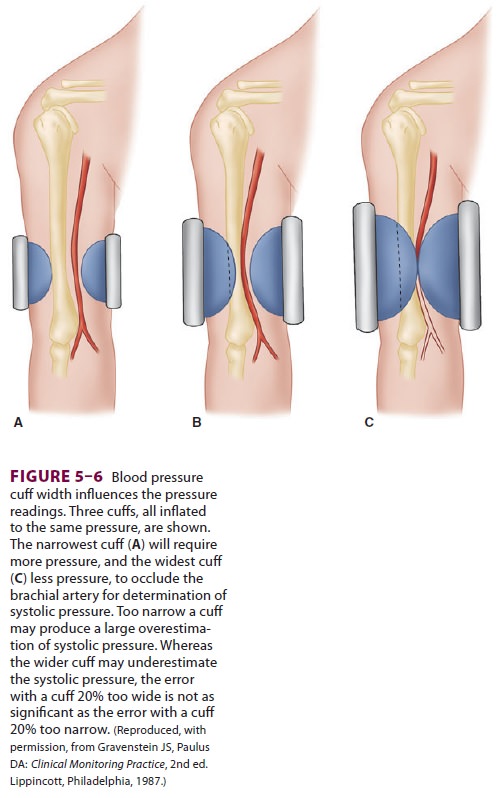
The accuracy of any method of blood
pressure measurement that involves a blood pressure cuff depends on proper cuff
size (Figure
5–6). The cuff ’s bladder should extend at least halfway around the
extremity, and the width of the cuff should be 20% to 50% greater than the
diameter of the extremity.
Automated blood pressure monitors, using
one or a combination of the methods described above, are frequently used in
anesthesiology. A self-con-tained air pump inflates the cuff at set intervals.
Incorrect or too frequent use of these automated devices has resulted in nerve
palsies and extensive extravasation of intravenously administered fluids. In
case of equipment failure, an alternative method of blood pressure determination
must be immedi-ately available.
Related Topics