Chapter: Clinical Anesthesiology: Anesthetic Equipment & Monitors : Cardiovascular Monitoring
Central Venous Catheterization
CENTRAL VENOUS CATHETERIZATION
Indications
Central venous catheterization is
indicated for monitoring central venous pressure (CVP), admin-istration of
fluid to treat hypovolemia and shock, infusion of caustic drugs and total
parenteral nutri-tion, aspiration of air emboli, insertion of transcu-taneous
pacing leads, and gaining venous access in patients with poor peripheral veins.
With special-ized catheters, central venous catheterization can be used for
continuous monitoring of central venous oxygen saturation.
Contraindications
Relative contraindications include
tumors, clots, or tricuspid valve vegetations that could be dis-lodged or
embolized during cannulation. Other contraindications relate to the cannulation
site. For example, subclavian vein cannulation is relatively contraindicated in
patients who are receiving anti-coagulants (due to the inability to provide
direct compression in the event of an accidental arterial puncture). Some
clinicians avoid central venous cannulation on the side of a previous carotid
endar-terectomy due to concerns about the possibility of unintentional carotid
artery puncture. The presence of other central catheters or pacemaker leads may
reduce the number of sites available for central line placement.
Techniques & Complications
Central venous cannulation involves
introducing a catheter into a vein so that the catheter’s tip lies with the
venous system within the thorax. Generally, the optimal location of the
catheter tip is just superior to or at the junction of the superior vena cava
and the right atrium. When the catheter tip is located within the thorax,
inspiration will increase or decrease CVP, depending on whether ventilation is
controlled or spontaneous. Measurement of CVP is made with a water column (cm H2O), or, preferably, an electronic transducer (mm
Hg). The pressure should be mea-sured during end expiration.
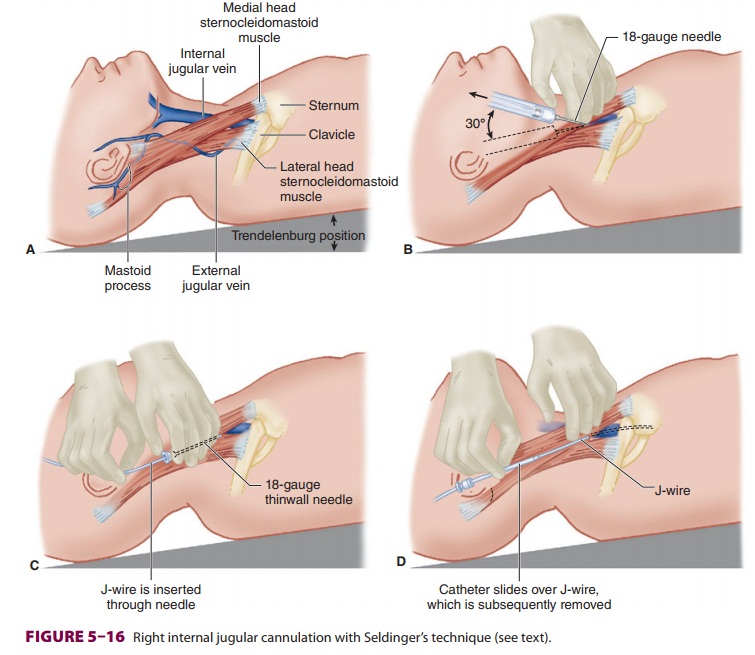
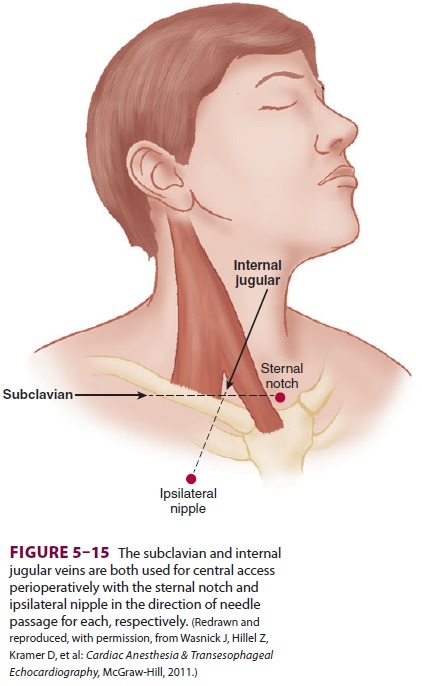
Various sites can be used for
cannulation (Figure
5–15 and Table 5–1). All cannulation sites have an
increased risk of line-related infections the longer the catheter remains in
place. Compared with other sites, the subclavian vein is associated with a
greater risk of pneumothorax during insertion, but a reduced risk of other
complications during pro-longed cannulations (eg, in critically ill patients).
The right internal jugular vein provides a combination of accessibility and
safety. Left-sided internal jugular vein catheterization has an increased risk
of pleural effusion and chylothorax. The external jugular veins can also be
used as entry sites, but due to the acute angle at which they join the great
veins of the chest, are associated with a slightly increased likelihood of
failure to gain access to the central circulation than the internal jugular
veins. Femoral veins can also be cannulated, but are associated with an
increased risk of line-related sepsis. There are at least three cannu-lation
techniques: a catheter over a needle (similar to peripheral catheterization), a
catheter through needle (requiring a large-bore needle stick), and catheter
over a guidewire (Seldinger’s technique; Figure 5–16). The overwhelming majority of
centrallines are placed using Seldinger’s technique.
The following scenario describes the
placement of an internal jugular venous line. The patient is placed in the
Trendelenburg position to decrease the risk of air embolism and to distend the
internal jug-ular (or subclavian) vein. Venous catheterization requires full
aseptic technique, including scrub, sterile gloves, gown, mask, hat,
bactericidal skin preparation (alcohol-based solutions are preferred), and
sterile drapes. The two heads of the sternoclei-domastoid muscle and the
clavicle form the three sides of a triangle (Figure 5–16A). A 25-gauge nee-dle
is used to infiltrate the apex of the triangle with local anesthetic. The
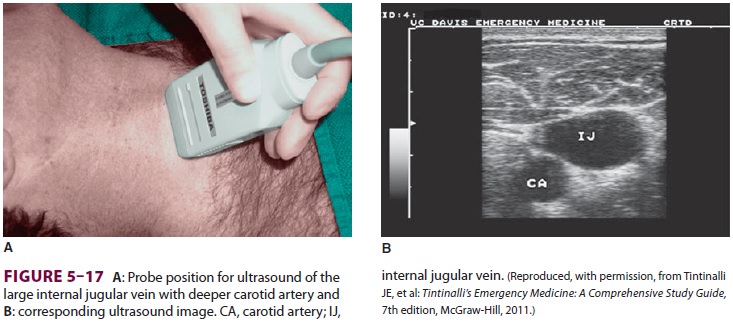
internal jugular vein can be located using ultrasound, and we strongly.
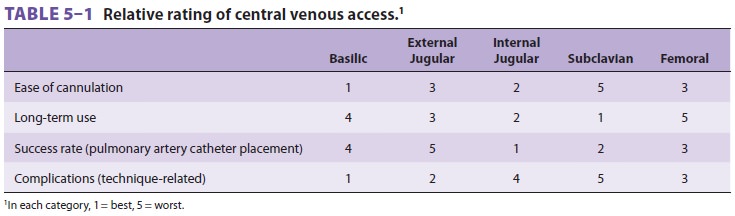
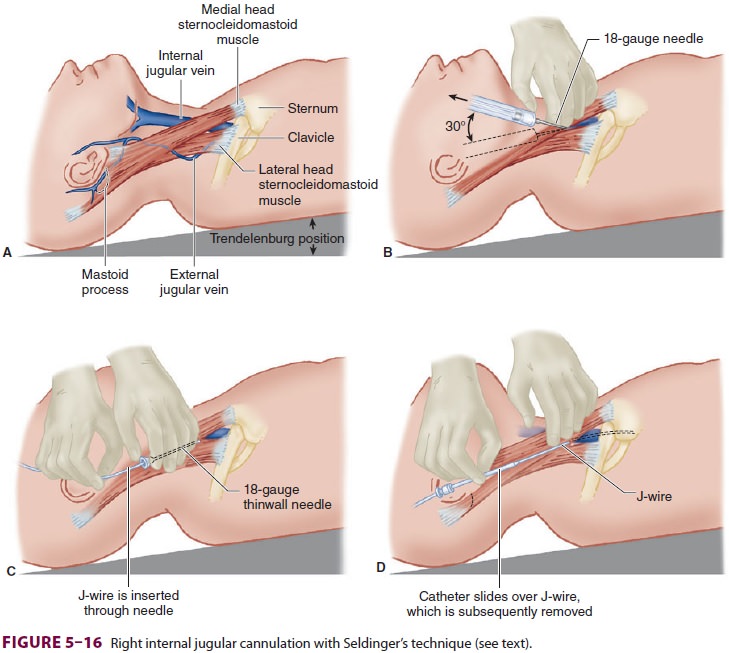
recommend that it be used whenever
possible (Figure
5–17). Alternatively, it may be located by advancing the 25-gauge
needle—or a 23-gauge nee-dle in heavier patients—along the medial border of the
lateral head of the sternocleidomastoid, toward the ipsilateral nipple, at an
angle of 30° to the skin. Aspiration of venous blood confirms the vein’s
loca-tion. It is essential that the vein (and not the artery) be cannulated.
Cannulation of the carotid artery can lead to hematoma, stroke, airway
compromise, and possibly death. An 18-gauge thin-wall needle or an 18-gauge
catheter over needle is advanced along the same path as the locator needle
(Figure 5–16B), and, with the latter apparatus, the needle is removed from the
catheter once the catheter has been advanced into the vein. When free blood
flow is achieved, a J wire with a 3-mm radius curvature is introduced after
confirmation of vein puncture (Figure 5–16C). The needle (or catheter) is
removed, and a dilator is advanced over the wire. The catheter is prepared for
insertion by flushing all ports with saline, and all distal ports are “capped”
or clamped, except the one through which the wire must pass. Next, the dilator
is removed, and the final catheter is advanced over
the wire (Figure 5–16D). The guidewire
is removed, with a thumb placed over the catheter hub to prevent aspiration of
air until the intravenous catheter tubing is connected to it. The catheter is
then secured, and a sterile dressing is applied. Correct location is confirmed
with a chest radiograph. 1 The
catheter’s tip should not be allowed to migrate
into the heart chambers. Fluid administration sets should be changed
frequently, per your medical center protocol. Th e possibility of placement of
the vein dilator or catheter into the carotid artery can be decreased by
transducing the vessel’s pressure waveform from the introducer needle (or
catheter, if a catheter over needle has been used) before passing the wire
(most simply accomplished by using a sterile intravenous extension tubing as a
manometer). Alternatively, one may compare the blood’s color or Pao2 with an arterial sample. Blood color and pulsatility
can be misleading or inconclusive, and more than one confirmation method should
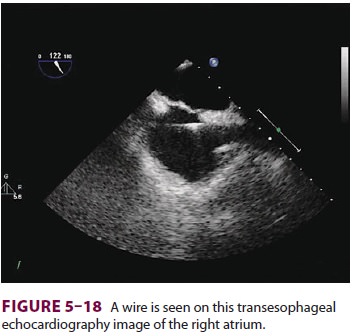
be used. In cases where transesophageal echocardiography (TEE) is used, the
guide wire can be seen in the right atrium, confirming venous entry (Figure
5–18).
The risks of central venous cannulation
include line infection, blood stream infection, air or thrombus embolism,
arrhythmias (indicating that the catheter tip is in the right atrium or
ventricle), hematoma, pneumothorax,
hemothorax, hydrothorax,
chylothorax, cardiac perforation, cardiac tamponade, trauma to nearby nerves
and arteries, and thrombosis.
Clinical Considerations
Normal cardiac function requires adequate ventricular filling by venous blood. CVP approximates right atrial pressure. Ventricular volumes are related to pressures through compliance. Highly compliant ventricles accommodate volume with minimal changes in pressure. Noncompliant systems have larger swings in pressure with less volume changes. Consequently, an individual CVP measurement will reveal only limited information about ventricu-lar volumes and filling. Although a very low CVP may indicate a volume-depleted patient, a mod-erate to high pressure reading may reflect either volume overload or poor ventricular compliance. Changes associated with volume loading coupled with other measures of hemodynamic performance (eg, blood pressure, HR, urine output) may be a bet-ter indicator of the patient’s volume responsiveness. CVP measurements should always be considered within the context of the patient’s overall clinical perspective.
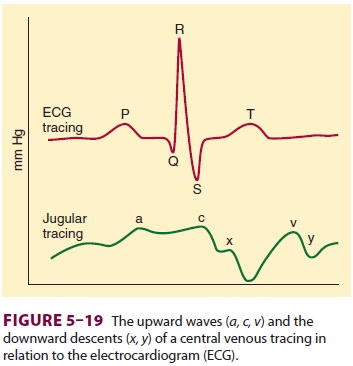
The shape of the central venous waveform
corresponds to the events of cardiac contraction (Figure 5–19): a waves from atrial contraction are absent in atrial fibrillation and are
exaggerated in junctional rhythms (“cannon” a
waves); c waves are due to tricuspid
valve elevation during early ven-tricular contraction; v waves reflect venous
return against a closed tricuspid valve; and the x and y descents are
probably caused by the downward dis-placement of the tricuspid valve during
systole and tricuspid valve opening during diastole.
Related Topics