Chapter: Basic & Clinical Pharmacology : Antidepressant Agents
Monoamines and Other Neurotransmitters
Monoamines and Other Neurotransmitters
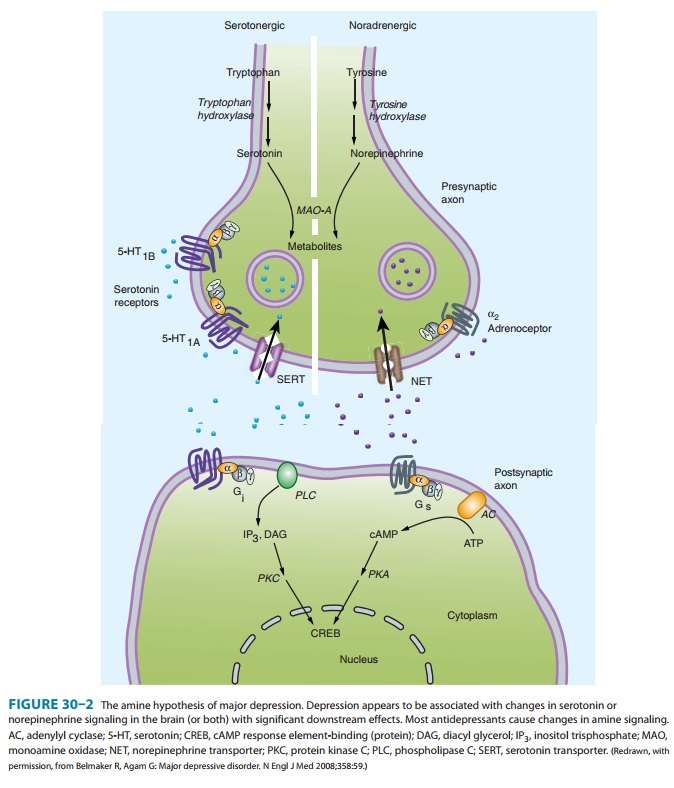
The monoamine hypothesis of depression (Figure
30–2) suggests that depression is related to a deficiency in the amount or
functionof cortical and limbic serotonin (5-HT), norepinephrine (NE), and
dopamine (DA).
Evidence to support the monoamine hypothesis
comes from several sources. It has been known for many years that reserpine
treatment, which is known to deplete monoamines, is associated with depression
in a subset of patients. Similarly, depressed patients who respond to
serotonergic antidepressants such as flu-oxetine often rapidly suffer relapse
when given diets free of tryp-tophan, a precursor of serotonin synthesis.
Patients who respond to noradrenergic antidepressants such as desipramine are
less likely to relapse on a tryptophan-free diet. Moreover, depleting
cate-cholamines in depressed patients who have previously responded to
noradrenergic agents likewise tends to be associated with relapse.
Administration of an inhibitor of norepinephrine synthe-sis is also associated
with a rapid return of depressive symptoms in patients who respond to
noradrenergic but not necessarily in patients who had responded to serotonergic
antidepressants.
Another line of evidence supporting the
monoamine hypothesis comes from genetic studies. A functional polymor-phism
exists for the promoter region of the serotonin trans-porter gene, which
regulates how much of the transporter protein is available. Subjects who are
homozygous for the s (short) allele may be more vulnerable to developing major
depression and suicidal behavior in response to stress. In addi-tion,
homozygotes for the s allele may also be less likely to respond to and tolerate
serotonergic antidepressants. Conversely, subjects with the l (long) allele
tend to be more resistant to stress and may be more likely to respond to
serotonergic anti-depressants.
Studies of depressed patients have sometimes
shown an alteration in monoamine function. For example, some studies have found
evidence of alteration in serotonin receptor numbers (5-HT1A and
5-HT2C) or norepinephrine (α2) receptors in depressed and suicidal
patients, but these findings have not been consistent. A reduction in the
primary serotonin metabolite 5-hydroxyindoleacetic acid in the cerebrospinal
fluid is associ-ated with violent and impulsive behavior, including violent
sui-cide attempts. However, this finding is not specific to major depression
and is associated more generally with violent and impulsive behavior.
Finally, perhaps the most convincing line of
evidence support-ing the monoamine hypothesis is the fact that (at the time of
this writing) all available antidepressants appear to have significant effects
on the monoamine system. All classes of antidepressants appear to enhance the
synaptic availability of 5-HT, norepineph-rine, or dopamine. Attempts to
develop antidepressants that work on other neurotransmitter systems have not
been effective to date.
The monoamine hypothesis, like the neurotrophic
hypothe-sis, is at best incomplete. Many studies have not found an alteration
in function or levels of monoamines in depressed patients. In addition, some
candidate antidepressant agents under study do not act directly on the
monoamine system. These include glutamate antagonists, melatonin agonists, and
gluco-corticoid-specific agents. Thus, monoamine function appears to be an
important but not exclusive factor in the pathophysiology of depression.
Related Topics