Chapter: 11th Microbiology : Chapter 12 : Medical Microbiology
Microbial Infections of the Human Body
Microbial Infections of the Human
Body
Medical microbiology is the branch of microbiology which deals
with prevention, diagnosis and treatment of infectious diseases. There are four
kinds of microorganisms that cause infectious diseases. They are bacteria,
fungi, parasites and viruses. Any disease that spreads from one host to
another, either directly or indirectly is said to be a communicable disease.
Chicken pox, measles, genital herpes, typhoid fever and tuberculosis are
examples of such diseases, that are easily spread from one person to another.
A non communicable disease does not spread from one host to
another. For example, Clostridium tetani,
a soil inhabitant, produces Tetanus when it is introduced into a wound or an
abrasion. Tetanus is thus an infectious disease, but not communicable.
Infectious disease occurs when the infecting microorganism
causes damage to the host. The term infection refers to the establishment of
the microorganisms in the tissues resulting in injury or harmful effect to the
host. Infection is a pathological condition due to the growth of microorganisms
in a host. To initiate an infection, a pathogenic microbe enters the tissues of
the body by a characterization route, the portal of entry.
Routes of Infections
There are various ways in which microorganisms enters into the
host are explained below.
a. Contact
Infection may be acquired by contact which may be direct or
indirect. Sexually transmitted diseases such as syphilis and gonorrhea spread
by direct contact. Indirect contact may be through the agency of inanimate
objects such as clothing, pencils or toys which may be contaminated by a
pathogen from one person to another. Pencils shared by school children may act
as fomites in the transmission of diphtheria, and face towels in trachoma.
b. Inhalation
Respiratory infections such as influenza and tuberculosis are
transmitted by inhalation of the pathogen in droplet and droplet nuclei that
are shed by the patients during sneezing, speaking or coughing. Common cold
virus, Adenovirus is some of the virus producing respiratory infections.
c. Ingestion
Intestinal infections are generally acquired by the ingestion of
food or drinks contaminated by pathogens. Infection transmitted by ingestion
may be waterborne (cholera), food borne (typhoid) or fecal-oral route
(dysentery).
d. Inoculation
Pathogens, in some instances, may be inoculated directly into
the tissues of the host. Tetanus spores implanted in the depth of wounds,
rabies virus deposited subcutaneously by dog bites, inoculation through
unsterile syringes and surgical equipments are examples that enter through
direct inoculation.
e. Congenital
Some pathogens are able to cross the placental barrier and
infect the fetus in uterus. Bacteria like Treponema
pallidum, viruses like Rubella,
Cytomegalovirus parasite like Toxoplasma
gondi are some of the organisms that enter through placenta and cause
disease in the newborn.
Types of Infections
Infections may be classified in various ways. Initial infection
with a parasite in a host is called a primary infection. Subsequent infections
by the same parasite in the host are termed reinfections. When a new parasite
sets up an infection in a host whose resistance is lowered by a preexisting
infectious disease, this is termed secondary infection.
When in a patient already suffering from a disease, a new
infection is setup from another host or other external sources it is termed
cross infection. Cross infections occurring in hospitals are called nosocomial
infections. Iatrogenic infection refers to physician induced infections
resulting from investigative, therapeutic or other procedures.
Depending on whether the source of infection is from the host’s
own body or from external sources, infections are classified as endogenous or exogenous, respectively.
Endogenous infection
Endogenous infections are acquired from the host himself from
the normal flora of the body.
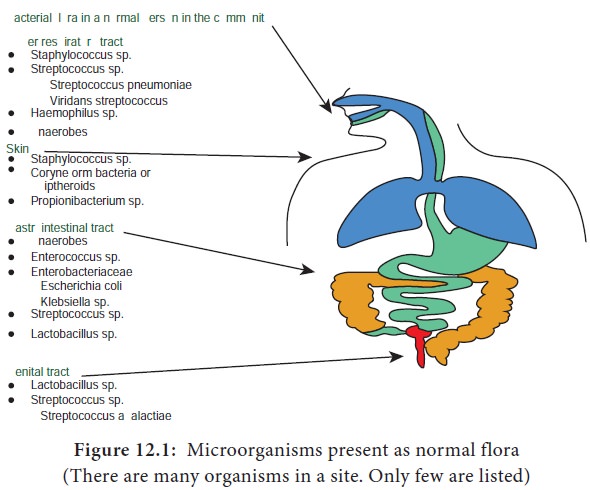
Microorganisms are present in certain areas of the body in all
human beings. They are called normal flora. The common areas are Nose, Mouth,
Teeth, Throat, Intestine, Urethra, Vagina and Skin (Figure 12.1).
1.
When the skin is breached normal flora enters the tissues.
2.
When the urethral organisms ascend, they cause urinary tract
infection
3.
When a patient is treated with antibiotics, normal flora is
eliminated and replaced by potential pathogens
4.
When the intestine is perforated, normal flora enter the
previously sterile body parts
5.
Similarly when the pH of the vagina increases potential
pathogens occupy the space.
However normal flora helps host against pathogen and benefits
the host in many ways
·
Normal flora of skin produces fatty acids which inhibit other
species
· Intestinal bacteria secrete antibacterial substances (bacteriocins, colicins) and many metabolic products that prevent other species to survive.
·
Because of their large numbers other species do not have space
in the intestine
· Acidic environment created by vaginal Lactobacilli suppresses growth of other bacteria.
Exogenous sources of infections
Human beings: The commonest source of infections in human are from other human beings. The parasite
may originate from a patient or a carrier. A patient is a person who harbours
the pathogenic microorganism and suffers from ill effect because of it. A healthy carrier is the one who harbours the pathogens but has
never suffered from the disease caused by the pathogen. A convalescent carrier is one who has recovered from the disease and
continues to harbor the pathogen in his body (Figure 12.2).
Animals: Many pathogens are
able to infect both human beings and animals. Infectious disease
transmitted from animals to human beings are called zoonoses. Zoonotic diseases
may be bacterial (Example: plague from rats) or viral (Example: rabies from
dogs).
Insects: Blood sucking insects
may transmit pathogens to human
beings. The diseases so caused are called arthopod borne diseases. Insects such
as mosquitoes, ticks, mites, flies, fleas and lice that transmit infections are
called vectors.
Transmission may be mechanical or biological. Mechanical transmission is the passive transport of the pathogens on the insects feet or other body parts. Example: Houseflies can transfer the pathogens of Typhoid fever and Bacillary dysentery (shigellosis) from feces of infected people to food. Such vectors are called mechanical vectors.
Biological transmission is an active process and is more
complex. The pathogens multiply in the body of the vectors often undergoing
part of a developmental cycle in it. Such vectors are termed biological
vectors. Example: Aedes aegypti
mosquito transmitting dengue, Anopheles
mosquito transmitting malaria.
Soil: Some pathogens are
able to survive in the soil for very
long periods. Spores of tetatus bacilli may remain viable in the soil for
several decades and serve as the source of infection.
Water: Water may act as the
source of infection due to contamination with pathogenic microorganisms.
Example: Cholera causing Vibrio cholerae.
Food: Contaminated food materials
may act as source of infection. The presence of pathogens in food
may be due to external contamination. Example: Food contaminated by Staphylococcus.
Types of Infectious Diseases
Infectious diseases may be localised or generalised.
Localised infections: An infection that is restricted to a specific location or region within the
body of the host is called localised infection.
Generalised infections: An infection that has spread to several regions or areas in the body of the
host. This involves the spread of the infecting agent from the site of entry
through tissue spaces or channels, along the lymphatics or through the
bloodstream.
Circulation of bacteria in the blood is known as Bacteremia. Septicemia is the condition
where bacteria circulate and multiply in the blood, form toxic products and
cause high fever. Pyemia is a condition where
pyogenic bacteria produce septicemia with multiple abscesses in the internal
organs such as the spleen, liver and kidney.
Occurrence of a disease
To understand the full scope of a disease, we should know about
its occurrence. Epidemiology involves in the study of the frequency and
distribution of disease and other health related factors in defined
populations. The incidence of a disease is the number of people in a population
who develop a disease during a particular time period. The prevalence of a
disease is the total number of existing cases with respect to the entire
population.
Depending on the spread of infectious disease in the community,
they may be classified into different types.
·
Endemic diseases are those which are constantly present in a
particular area. Typhoid fever is endemic in most parts of India.
·
Epidemic disease is one that spreads rapidly, involving many
persons in an area at the same time. Example: Epidemic of Dengue in 2017.
·
A pandemic is an epidemic that spreads through many areas of the
world involving very large numbers of persons within a short period. Example:
H1N1 Influenza outbreak in 2009. Ebola outbreak in 2014-2016 in West Africa was
the largest in history and first ever epidemic, affecting multiple countries.
·
If a particular disease occurs only occasionally, it is called a
sporadic disease. The most commonly occurring sporadic diseases in India are
Diphtheria and Hepatitis A and E.
Severity or duration of a disease
·
Another useful way of defining the scope of a disease is in
terms of its severity or duration.
·
An acute disease is one that
develops rapidly but lasts for a short time.
·
A chronic disease develops more
slowly, and the body’s reactions may be less severe, but the disease is likely
to be continual or recurrent for long periods.
·
A disease that is intermediate between acute and chronic is
described as a subacute disease.
Interaction between Microbes and Host
Pathogen is a microorganism which causes disease.
Pathogenecity is the ability of a pathogen to produce disease.
Virulence is the degree of pathogenecity of a microorganism.
Virulence is not generally attributable to a single property but depends on
several parameters related to the organism, the host and their interaction.
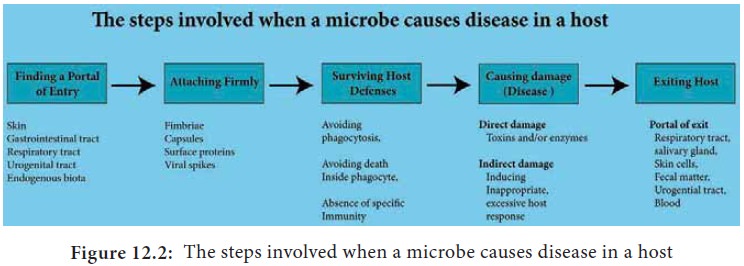
Microorganisms first enter the body, survive, multiply and
elaborate many factors and produce the disease.
Adhesion: The initial event in
the pathogenesis of many infections is the attachment of the
bacteria to body surfaces. Adhesions may occur as organized structures, such as
fimbriae and pili. Adhesions serve as virulence factors.
Capsule: It is an envelope or
slime layer surrounding the cell wall of certain microorganisms.
Capsule plays important roles in immune evasion as it inhibit’s phagocytosis,
as well as protecting the bacteria while outside the host.
Toxins: Toxins are specific
chemical products of microbes, plants and some animals that are poisonous
to other organisms. Toxigenicty is the power to produce toxins.
A toxin is named according to specific target of action: Neurotoxin acts on the nervous system. Enterotoxin acts on the intestine, Haemotoxin lyses red blood cells, and Nephrotoxins damages the kidneys.
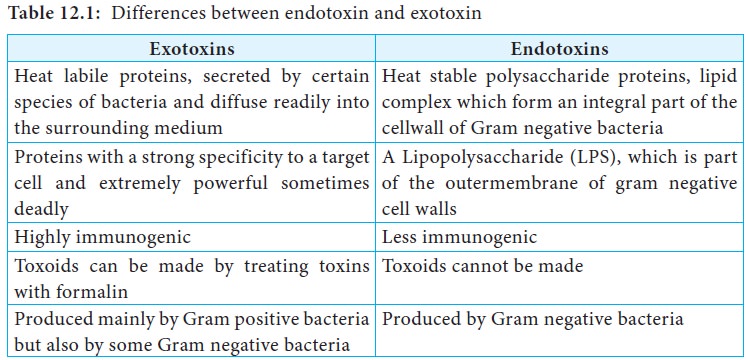
A toxin molecule secreted by a living bacterial cell into the
infected tissue is an exotoxin. A toxin that is not
actively secreted but is shed from the
outer membrane is an endotoxin. the difference
between exotoxin and endotoxin were
given in Table 12.1.
Production of enzymes
Some enzymes like proteases, DNAases and phospholipases are
produced and they help in destruction of the cell structure and to hydrolyse
host tissues.
Antigenic variation
Microorganisms evade the host immune responses by changing their
surface antigens. Antigenic drift and antigenic shift are common in influenza
viruses. The distinction between the commensal and the organism associated with
disease.
Diagnostic Cycle
Specific diagnosis is important for better patient care, use of
appropriate antibiotics and to initiate appropriate preventive measures. The
diagnostic cycle begins when the clinician takes a microbiological sample and
ends when a clinician receives the laboratory report and uses the information
to manage the condition (Figure 12.3).
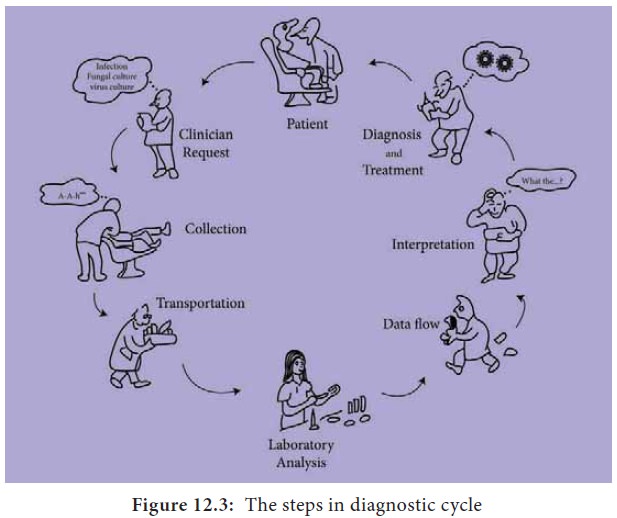
The steps in diagnostic cycle are
1.
Clinical request and provision of clinical information.
2.
Collection and transport of appropriate specimens.
3.
Laboratory analysis.
4.
Interpretation of microbiology report and use of the
information.
Specimen Collection and transport: It is important to collect
the specimen appropriately and protect it from contamination. Transport media
are used that are compatible with the organism believed to be present in the
clinical sample. Quality of patient specimens and their transport to the
laboratory is important.
Infections and samples used
Respiratory tract infections: Nasal and bronchial washings,
throat and nasal swabs, sputum.
Eye infections: Conjunctival swab or scraping.
Wound infections: Pus, skin scraping, wound swap.
Gastrointestinal infections: Stool, rec-tal swabs.
Genital infections: Vesicle fluid or swab.
Urinary tract infections: Urine.
Blood borne infections: Blood.
Nervous system infections: Cerebro-spinalfluid (CSF).
Laboratory diagnosis of infectious agents
Direct diagnosis:
It is
the demonstration of the
presence of an infectious agent, antigen or nucleic acids
Indirect diagnosis: It is the demonstration of presence of antibodies to a particular
infectious agent, cytopathic effects, haemagglutination, inclusion bodies and
neutralization.
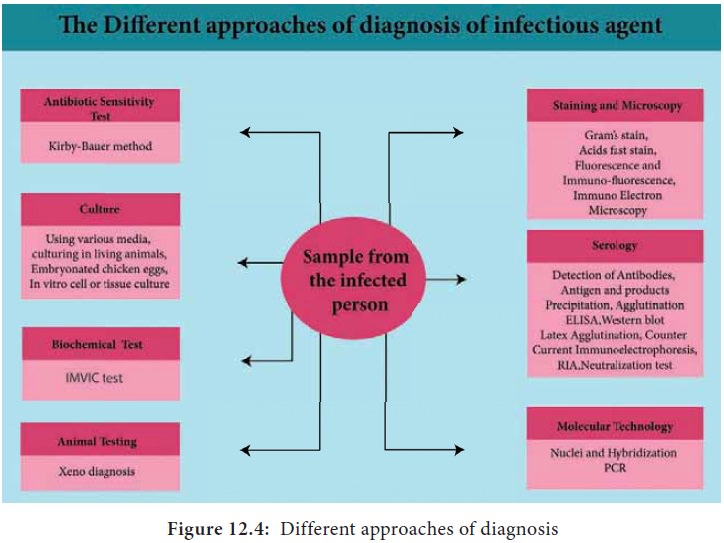
The different approaches for diagnosis or identification of
infectious agents are shown in Figure 12.4.
Related Topics