Chapter: 11th Microbiology : Chapter 12 : Medical Microbiology
Skin and Wound Infections
Skin and Wound Infections
The skin, which covers and protects the body, is the body’s
first line of defense against pathogens. As a physical barrier, it is almost
impossible for the pathogens to penetrate it. However, microorganisms can enter
through skin breaks that are not readily apparent, and the larval forms of a
few parasites can penetrate the intact skin. The skin has up to seven layers
(Figure 12.5) of ectodermal tissue and guards the underlying tissues viz;
muscles, bones, ligaments and internal organs. Nearly all human skin is covered
with hair follicles. Because it interfaces with the environment, skin plays an
important role in protecting the body against pathogens and excessive water
loss. Its other functions are insulation, temperature regulation, sensation,
synthesis of vitamin D, and the protection of vitamin B folates. Severely
damaged skin will try to heal by forming scar tissue. This is often discolored
and depigmented.
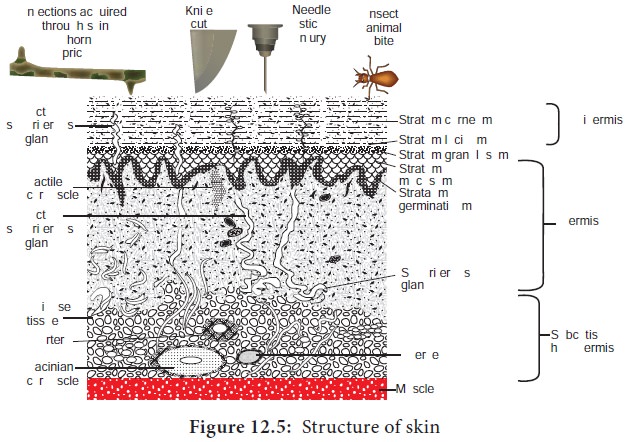
Structure of Skin
Skin is composed of three primary layers: the epidermis, the
dermis and the hypodermis.
Epidermis
It forms the water proof, protective wrap over the body’s
surface. It also serves as a barrier to infection. It is made up of stratified
squamous epithelium with an underlying basal lamina. The outermost layer of the
epidermis, the stratum corneum, consists of dead cells that contain a
waterproofing protein called keratin. The epidermis contains no blood vessels
and cells in the deepest layers are nourished exclusively by diffused oxygen
from the surrounding air. The main types of cells present in epidermis are
Merkel cells, keratinocytes with melanocytes and Langerhan cells.
Dermis
The dermis is the layer of skin beneath the epidermis that
consists of epithelial tissue and cushions the body from stress and strain. The
dermis is tightly connected to the epidermis by a basement membrane. It also
harbors many nerve endings that provide the sense of touch and heat. It
contains the hair follicles, sweat glands, sebaceous glands, apocrine glands,
lymphatic vessels and blood vessels. The blood vessels in the dermis provide
nourishment and waste removal from its own cells as well as from the Stratum
basale of the epidermis.
Hypodermis
Subcutaneous tissue (also hypodermis
and subcutis) is not part of the
skin, and lies below the dermis of
the cutis. Its purpose is to attach the skin to underlying bone and muscle as
well as supplying it with blood vessels and nerves. It consists of loose
connective tissue, adipose tissue and elastin. The main cells are fibroblasts,
macrophages and adipocytes (subcutaneous tissue contains 50% of body fat). Fat
serves as padding and insulation for the body.
The hair follicles, sweat gland ducts, and oil gland ducts in
the dermis provide passageways through which the microorganisms can enter the
skin and penetrate deeper tissues. Perspiration provides moisture and some
nutrients for microbial growth. However, it contains salt, which inhibits many
microorganisms; the enzyme lysozyme, which is capable of breaking down the cell
walls of certain bacteria and antimicrobial peptides. Sebum, secreted by oil
glands, is a mixture of lipids (unsaturated fatty acids), proteins, and salts
that prevents skin and hair from drying out. Although the fatty acids inhibit
the growth of certain pathogens, sebum, like perspiration, is also nutritive
for many microorganisms
Normal Microbiota of the Skin
The skin’s normal microbiota contains relatively large numbers
of Gram positive bacteria, such as Staphylococci
and Micrococci. Bacteria in the skin
tends to be grouped into small
clumps. Vigorous washing can reduce their numbers but will not eliminate them.
Microorganisms remaining in hair follicles and sweat glands after washing will
soon reestablish the normal populations. Areas of the body with high moisture,
such as armpits and between the legs, have higher populations of
microorganisms. They metabolize secretions from the sweat glands and are the
main contributors to body odour.
Also part of the skin’s normal microbiota are Gram positive
pleomorphic rods called diphtheroids. Some diphtheroids, such as Propionibacterium acnes, are typically anaerobic
and inhabit hair follicles. These bacteria produce propionic acid, which helps
maintain the low pH of skin, generally between 3 and 5
Wound Infection
Wound can be defined as any interruption of continuity of
external or internal surfaces caused by violence
Wounds may occur following: surgery, trauma or injections
Wound infections may occur mainly after surgical procedures
Wound sepsis is the result of cross infection from human sources
and from other outside sources.
Bacteria associated with wound infections
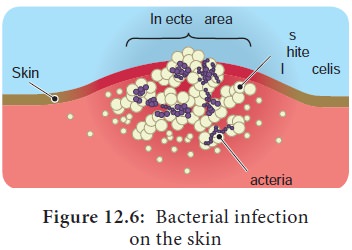
Many bacteria are associated with wound infection (Figure 12.6).
The normal flora may also cause infection. The most common normal flora of the
skin are: Staphylococci, and various Streptococci, Sarcina sp, anaerobic Diphtheroids, Gram negative rods and others.
Factors determining the ecology of the skin bacteria
The main factors that determine the ecology of skin bacteria:
·
Climate: Temperature and humidity
·
The effect of free fatty acids
·
Maintenance of the flora by products of skin secretions and
other bacterial inhibitors.
Defence against infection
·
Intact skin: Normal uninterrupted skin provides protection
against invasion by bacteria.
·
Lysozyme in sweat: The enzyme lysozyme provides protection
against Gram positive bacteria by lysing the cell wall.
·
IgA antibodies in the sweat and secretions provide first line of
defense against infection.
·
Inhibitors like unsaturated fatty acids provide protection
against bacteria.
·
Bacteriocins produced by the normal flora prevent the
establishment of other bacteria.
Factors responsible for wound infections
a) Host factors
The following factors help the organisms to survive and produce the infections:
·
Extremes of age: Very old and very young people are susceptible
to infection.
·
Diabetes mellitus: Hormonal imbal-ance increases susceptibility.
·
Steroid therapy: Immune responses are affected.
·
Obesity: Increases susceptibility.
·
Malnutrition: General health status affected.
·
Immunocompromisedindividual: Immune system will not function
properly.
·
Presence of remote infection at the time of surgery.
b) Exogenous Factors
·
Use
of unsterile
instruments:
They carry pathogens.
·
Surgeons hands / from health workers: May carry pathogens.
·
Air / Hospital environments: Unclean environment harbur
pathogens.
c) Endogenous Factors
·
Wound contamination from the patient source: From the normal
flora.
·
Wound penetrating through structures containing normal flora.
·
Surgical procedures involving mucous membranes harbouring normal
flora.
·
Patients carrying pathogens in their nose, throat, axilla.
Etiological agents
Etiological agents like Pseudomonas
aeruginosa, Staphylococcus aureus,
Proteus, member of enterobacteriaceae
anaerobic organisms, anaerobic cocci and bacteroides cause infections.
Post operative infections
Gasgangrene organisms like Clostridium
perfringens, Staphylococcus aureus and
Clostridium tetani may cause post
operative infections.
Route of entry
Wounds may occur following surgery, trauma or injections. Wound
infections may occur mainly after surgical procedures. Wound sepsis is the
result of cross infection from human sources and from other outside sources.
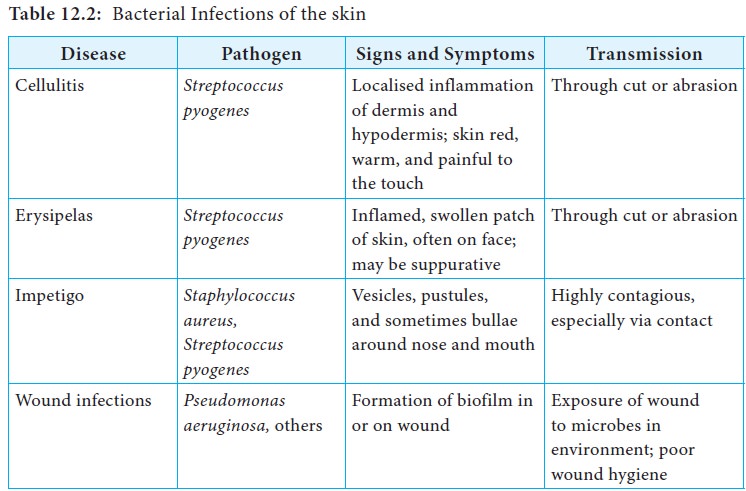
Infections of skin are listed in Table 12.2.
Mechanisms of damage
1. Organisms enter through the skin, multiply there and produce
the disease in the skin.
For example, impetigo, abscess and cellulitis (Figure 12.7) are
caused by Staphylococcus aureus and Streptococcus pyogenes.

As soon as the organisms enter the skin they multiply and
produce various toxins that kill the cells and produce cellulitis. Further
damage leads to necrosis and ulcer formation (Figure 12.8).

2. Organisms multiply in the skin and produce disease in internal organs. For example some Group A Streptococci multiply in the skin and produce disease known as Acute Glomerulonephritis causing damage to the kidneys. Some times Corynebacterium diphtheriae may multiply in the skin and affect the heart due to the toxin
3. Sometimes organism may multiply in the skin and produce the
toxin which affect the Central Nervous System (CNS) and the effects seen. In
the case of Clostridium tetani
infection, convulsions and paralysis occur due to the production of a powerful
toxin.
Related Topics