Chapter: Obstetrics and Gynecology: Fetal Growth Abnormalities:Intrauterine Growth Restriction and Macrosomia
Macrosomia
MACROSOMIA
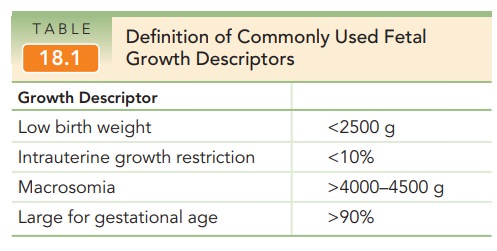
Two terms have been used to
define excessive fetal growth. Fetal
macrosomia is based on weight alone and refers to afetus with an estimated
weight of 4000–4500 g or greater. Large
for gestational age (LGA) generally implies a birthweight >90% for a
given gestational age, and is dependent on both weight and gestational age with
percentiles gener-ated from population-specific norms (see Table 18.1). By
definition, the prevalence of LGA is fixed, but not all neonates at the upper
extreme of size are pathologically large. Growth potential, growth rate, and
gestational age at onset may be important considerations.
Etiology
Macrosomia, like fetal growth
restriction, has multiple potential causes, categorized into fetal or maternal
factors (Box 18.2). Similar to fetal growth restriction, fetal factors include
the genetic composition or inherent growth poten-tial of the individual, and
genetic syndromes such as Beckwith-Wiedemann syndrome. Male fetuses are also
more commonly affected than female fetuses.
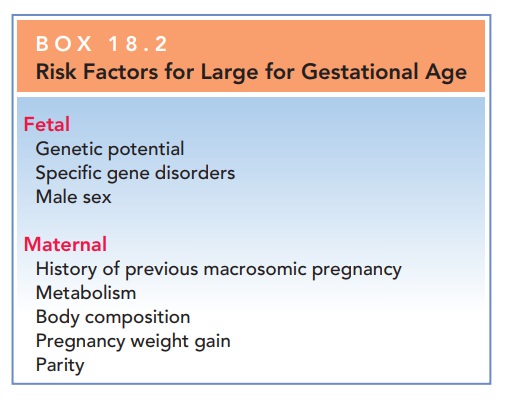
Maternal factors include a
history of macrosomia, maternal prepregnancy weight, weight gain during
preg-nancy, multiparity, male fetus, gestational age greater than 40 weeks,
ethnicity, maternal birth weight, maternal height, maternal age younger than 17
years, and a positive 50-g glu-cose screen with a negative result on the 3-hour
glucose tol-erance test.
The magnitude of glucose
intolerance during preg-nancy and specific measures of control are correlated
with fetal weight and fetal fat mass. Lipids are also associated with fetal
size, with triglycerides and free fatty acids posi-tively correlated to birth
weight, and triglycerides inde
Maternal body composition and body mass index are major determinants
of insulin sensitivity, independent of hypertension and pregestational or
gestational diabetes. Also, maternal weight gain and pregravid weight
contribute to the variance in fetal birth weight. Finally, increased parity is
associated with larger babies.
Significance
Macrosomia is associated with
both increased maternal and fetal/neonatal risks. A patient with a macrosomic
fetus has an increased risk of cesarean delivery, because of labor
abnormalities. The risk of postpartum hemorrhage and vaginal lacerations are
also elevated with macrosomia. Maternal infections associated with macrosomia
include urinary tract infection in women undergoing elective cae-sarean section
and puerperal fever in women undergoing a trial of labor. Risks to the fetus
are shoulder dystocia and fracture of the clavicle, although brachial plexus
nerve injury is rare. Macrosomic infants also have an increased risk for lower
Apgar scores.
Other neonatal risks are
partially dependent on the underlying etiology of macrosomia, such as maternal
obesity or diabetes, and may include an increased risk of hypothermia,
hyperbilirubinemia, hypoglycemia, prema-turity, and stillbirth. The
relationship between gestational age and fetal size is important. Macrosomic
preterm infants remain at risk for complications of prematurity. Size and
extent of maturity are independent. Long-term risks include overweight or
obesity in later life, again illus-trating that intrauterine growth may predict
the founda-tion of many aspects of lifelong physiologic function.
Diagnosis
Because the diagnosis of
macrosomia is based on an esti-mated fetal weight above the 90th percentile and
becomes increasingly imprecise at later gestational ages, careful dating of
pregnancy is important. The two primary meth-ods for clinical estimation of
fetal weight are Leopold maneuvers (abdominal palpation; see Fig. 9.7) and
mea-surement of the height of the uterine fundus above the maternal symphysis
pubis.
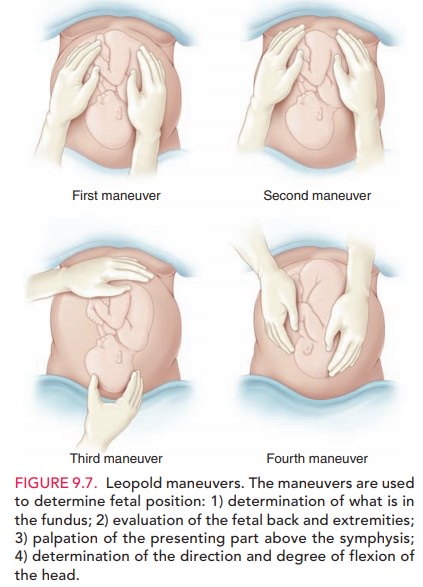
Measurement
of the symphysis–fundal height alone is a poor predictor of fetal macrosomia
and should be combined with clinical palpation of (Leopold maneuvers) to be
useful.
Clinical findings may be combined
with ultrasound to diagnose macrosomia. Ultrasound-derived estimates of fetal
weight are obtained by entering the measurements of various fetal body parts,
usually including the abdominal circumference, into one of several popular
regression equa-tions. However, most of the regression formulas currently in
use are associated with significant errors when the fetus is macrosomic. The
superiority of ultrasound-derived esti-mates of fetal weight over clinical
estimates has not been established.
The true
value of ultrasound in management of macrosomia is its ability to rule out the
diagnosis.
Differential diagnosis of an
enlarged uterus includes a large fetus, more than one fetus (multiple gestation),
extra amni-otic fluid (polyhydramnios), large placenta (molar preg-nancy), or
large uterus (uterine leiomyomata, other gynecologic tumor, or uterine
anomaly).
Management
For
mothers without diabetes, no clinical interventions designed to treat or curb
fetal growth when macrosomia is suspected havebeen reported. Current
evidence does not support earlydelivery for macrosomia alone, because induction
of labor does not decrease maternal and neonatal morbidity; it does increase
the rate of cesarean deliveries. In addition, the data do not support a
specific estimated fetal weight at which women should undergo elective cesarean
delivery.
Given the limitations of ultrasound estimations and the asso-ciation with increasing injury with increasing infant weight, the American College of Obstetricians and Gynecologists rec-ommends that a cesarean delivery should be offered for esti-mated fetal weights greater than 5000 g in women without diabetes and greater than 4500 g in women with diabetes.
Various techniques can be used to
facilitate vaginal delivery in the case of shoulder dystocia, such as
exaggerated flexion of the thighs (McRoberts maneuver), suprapubic pressure,
various rotations, episiotomy, delivery of the posterior arm, and intentional
clavicular fracture. The Zavanelli maneu-ver, cephalic replacement with
subsequent cesarean deliv-ery, has yielded mixed results. A prolonged second
stage of labor or arrest of descent in the second stage is an indica-tion for
cesarean delivery. Postpartum or neonatal manage-ment depends on gestational
age and underlying etiology.
Related Topics