Chapter: Obstetrics and Gynecology: Fetal Growth Abnormalities:Intrauterine Growth Restriction and Macrosomia
Intrauterine Growth Restriction: Diagnosis
Diagnosis
Assessment of gestational age is
important in early preg-nancy, because dating becomes increasingly imprecise at
later gestational ages.Antenatal
recognition of IUGR depends upon the recognition of risk factors and the
clinical assessment of uterine size, fol-lowed by biometric measurements.
Physical examination is limited
in usefulness in recognizing IUGR or in making a specific diagnosis, but it is
an impor-tant screening test for abnormal fetal growth. Maternal size and
weight gain throughout pregnancy also have limited value, but access to such
information is readily available; a low maternal weight or little or no weight
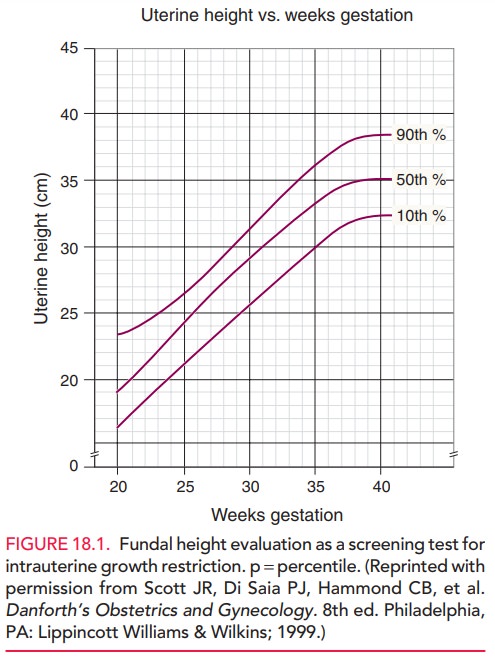
gain during pregnancy may suggest IUGR. Serial measurements of fundal height are commonly used as a
screening test forIUGR, but have high rates of false-negative and
false-positive predictive values. Between 20 and 36 weeks of ges-tation, fundal
height should increase approximately 1 cm per week, consistent with gestational
age in weeks (Fig. 18.1). A discrepancy may be related to constitutional
factors, but a significant discrepancy of more than 2 cm may indicate IUGR and
the need for an ultrasound examination. Clinical estimations of fetal weight
alone are not helpful in diagnos-ing IUGR, except when fetal size is grossly
diminished.
If IUGR
is suspected based on risk factors and clinical assessment, ultrasonography
should be performed to assess fetal size and growth. Specificfetal biometry measurementsare compared
with standardized tables that reflect normal growth at a certain gestational
age. The four standard fetal measurements include the (1) biparietal diameter,
(2) head circumference (HC), (3) abdominal circumference (AC), and (4) femur
length. Conversion of individual morphologic measurements to fetal weight using
published equations or ratios of measurements can provide useful estimations of
fetal size. An abdominal circumference within the normal range reliably
excludes growth restriction, with a false-negative rate of less than 10%. A
small abdominal circum-ference or fetal weight estimate below the 10th
percentile suggests the possibility of growth restriction, with the likelihood
increasing as the percentile rank decreases.
When IUGR
is suspected, serial measurements of fetal biometric parameters provide an
estimated growth rate. Suchserial measurements are of
considerable clinical value in confirming or excluding the diagnosis and
assessing the progression and severity of growth restriction. Given the high
incidence of genetic and structural defects associated with IUGR, a detailed
ultrasound survey for the presence of fetal structural and functional defects
may be indicated.
Following
recognition of altered fetal growth, a search for potential etiology should
ensue. Ultrasonography should in-clude a detailed anatomic
survey to evaluate for the pres-ence of structural anomalies, given the high
incidence of genetic and structural defects with IUGR. Ultrasound eval-uation
should also include an assessment of amniotic
fluidvolume. The combination of oligohydramnios (dimin-ished amniotic fluid
volume) and IUGR is associated with severe disease and increased morbidity. The
mechanism of decreased amniotic fluid is thought to be decreased placen-tal
perfusion of oxygen and nutrients with a compensatory redistribution of fetal
blood favoring the brain, adrenal gland, and heart. The consequent decrease in
fetal blood to the kidneys leads to a reduction of urine output, which is the
primary source of amniotic fluid in the second half of pregnancy.
Direct invasive studies of the
fetus are useful in selected patients with IUGR. Amniocentesis for fetal lung
matu-rity may assist delivery planning near term or when there is uncertainty
regarding gestational age and concern for growth restriction. Fetal karyotyping
and viral cultures and polymerase chain reactions can be performed on fluid
obtained by amniocentesis. Rarely, chorionic
villus sam-pling (biopsy of placenta) or direct blood sampling (per-cutaneous umbilical blood sampling)
may be necessaryfor specific studies.
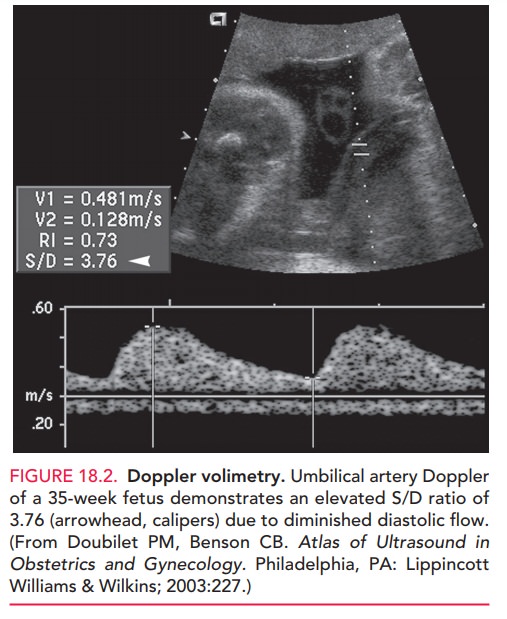
Doppler velocimetry of fetal vessels provides furtherinsight into the fetal response to altered growth, and has become part of the standard assessment of the fetus once IUGR is diagnosed. Doppler velocimetry has been shown to both reduce interventions and improve fetal outcome in pregnancies at risk for IUGR. Fetal-placental circula-tion is evaluated in the umbilical artery and is measured by a systolic/diastolic (S/D) ratio. The S/D indirectly mea-sures impedance or resistance downstream within the pla-cental vessels. As placental resistance increases, diastolic flow decreases and the S/D ratio rises. A normal S/D ratioat term is 1.8 to 2.0.
Fetuses with IUGR with absent or reversed diastolic flow have
progressively worse perinatal outcomes (Figure 18.2). The fetal middle cerebral
artery is also evaluated and reflects fetal adaptation. The patho-physiologic
response to reduced placental perfusion gen-erally spares the fetal brain,
resulting in an increase of diastolic and mean blood flow velocity in the
middle cere-bral artery. Ductus venosus may also be evaluated by Doppler
ultrasound, and the fetus with abnormal ductus flow is at very high risk of
adverse outcome.
Related Topics