Chapter: Medicine and surgery: Gastrointestinal system
Large bowel carcinoma - Gastrointestinal oncology
Large bowel carcinoma
Definition
Large bowel malignant adenocarcinoma.
Incidence
Lifetime incidence of 1 in 25. Second most common cause of cancer death.
Age
Average 60–65 years.
Sex
Rectal cancer M > F; colonic cancer F > M.
Geography
Rare in Africa and Asia (thought to be environmental).
Aetiology
Most colorectal cancers arise from adenomatous polyps with a median transition of 20 years. Ulcerative colitis is associated with an increased incidence.
Genetic predisposing conditions include familial adenomatous polyposis, hereditary non-polyposis colon cancer. There is an overall increased incidence in first-degree relatives.
Dietary factors such as a high animal fat and low fibre intake.
Pathophysiology
Colonic cancer occurs in the sigmoid colon and rectum (50%), caecum and ascending colon (30%) and transverse and descedending colon (20%). Carcinomas may be polypoidal, ulcerating or stenosing. The tumour spreads by direct infiltration into the bowel wall and circumferential spread. Subsequent invasion of the blood and lymphatics results in distant metastasis most frequently to the liver.
Clinical features
Presentation is dependant on the site of the lesion, but in general a combination of altered bowel habit and bleeding with or without pain is reported. Up to a third of patients present with obstruction, or perforation. Caecal or ascending colonic cancers often present later with iron deficiency anaemia. Examination may reveal a mass (on abdominal palpation or rectal examination), ascites and hepatomegaly.
Macroscopy/microscopy
Raised red lesions with a rolled edge and central ulceration. Adenocarcinomas are composed of glandular tissue made up of pleomorphic neoplastic epithelial cells.
Investigations
Endoscopic examination of the large bowel with biopsy is diagnostic.
Barium enema or CT pneumocolon may also detect tumours.
LFTs, liver ultrasound scan and chest X-rays are used to look for metastatic spread.
Pre-symptomatic disease may be identified by surveillance colonoscopy in at risk patients.
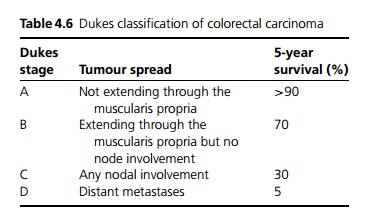
In a recent study the use of faecal occult blood testing as screening has a positive predictive value was 11% for cancer and 35% for adenoma. 48% of all detected cancers were Dukes stage A (see Table 4.6).
Management
Primary resection is the treatment of choice in fit patients (see also page 148).
· Tumours of the right and transverse colon require right hemicolectomy and ileocolic anastomosis.
· Tumours of the descending colon are treated with left hemicolectomy.
· Tumours of the sigmoid colon are treated with a sigmoid colectomy.
In all the procedures the associated mesentery and regional lymph nodes are removed en bloc.
Most rectal tumours are treated by anterior resection. In very low rectal lesions an abdominoperineal (AP) resection with formation of a permanent colostomy in the left iliac fossa may be required.
Resections may be curative or palliative, if resection is not possible a bypass procedure may be carried out. Adjuvant chemotherapy based on 5-fluorouracil (5-FU) is performed in patients with Dukes stage C (see below) but has not been shown to be beneficial in Stage A or B disease, or in elderly patients who have a higher incidence of complications. Patients with limited hepatic metastases may benefit from resection of the metastases.
Rectal carcinomas are just as likely to recur locally as metastasise distantly, so treatment is best with local radiotherapy and adjuvant chemotherapy.
Prognosis
The overall 5-year survival rate is 40% but this depends on Dukes staging (see Table 4.6).
Related Topics