Chapter: Microbiology and Immunology: Bacteriology: Neisseria
Laboratory diagnosis of Neisseria gonorrhoeae infection
Laboratory Diagnosis
Laboratory diagnosis of gonococcal infection depends on dem-onstration of N. gonorrhoeae at the site of infection.
◗ Specimens
The genital (urethral discharge, cervical discharge, etc.), rectal, and pharyngeal specimens are collected for the isolation and identification of gonococci.
· In acute gonococcal infection, urethral discharge in malesand cervical discharge in females are the specimens of choice. High vaginal swab in females is not satisfactory.
When collecting specimens, such as endocervical discharge in women, the cervix is first cleaned of the exudate; a swab is then placed into the external os and rotated for several seconds.
In males, discharge present at the meatus is collected for examination. The meatus is first cleaned with gauze soaked in saline. The urethral discharge is then col-lected with the help of a platinum loop. If no discharge is present at the meatus, urethral specimens are collected by inserting and rotating a small swab 2–3 cm into the ure-thra. A calcium alginate or Rayon swab on a metal shaft is usually used for this purpose.
· In chronic infection, since urethral discharge is less, theexudate after prostatic massage or morning drop of secretion and urine are also examined for the cocci. Rectal specimens are frequently useful for demonstration of gonococci in asymptomatic women and in homosexual and bisexual men.
· Samples are collected from all possible mucosal sites, such as pharynx, urethra, cervix, and rectum, and from blood and synovial fluid in patients with possible DGI.
After collection, the specimens are transported and pro-cessed immediately in the laboratory. If delay is unavoidable, specimens are collected and transported to the laboratory in a transport medium, such as Stuart’s transport medium.
◗ Microscopy
Gram stain of urethral exudates: The presence of four ormore polymorphonuclear (PMN) leukocytes per oil-immersion field in Gram-stained urethral exudate smear is diagnostic of urethritis:
· Demonstration of typical Gram-negative intracellular diplococci is characteristic of N. gonorrhoeae (Fig. 26-3, Color Photo 22).
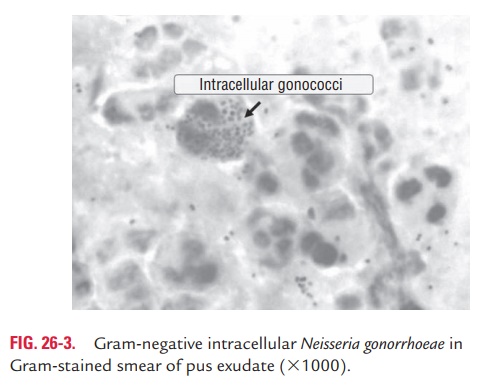
· Gram stain helps in the presumptive diagnosis of the gonococcal infection.
· It is more than 90% sensitive and 98% specific for the diagno-sis of gonococcal infection in symptomatic males. However, in asymptomatic males, the sensitivity of the Gram stain is only 60% or less.
In women, presence of more than 10 PMN per high-power field on an endocervical smear is suggestive of cervicitis. Gram stain of endocervical smears is less sensitive (50–60%) and 82–90% specific in both symptomatic and asymptomatic women.
Gram stain is not a sensitive method for detection of gono-cocci in patients with anorectal gonorrhea, pharyngitis, and
Specificity is also less because commensal Neisseria species in the oropharynx and gastrointestinal tract can be con-fused with those of N. gonorrhoeae.
Wet mount examination of centrifuged deposit of urine sample: In men, the urine sample, preferably 10–15 mL ofearly morning (the first) voided urine, is collected and centri-fuged and examined under high power. The demonstration of 10 or more PMN in the centrifuged urine under high power is suggestive of urethritis.
◗ Culture
Isolation of N. gonorrhoeae from clinical specimens by culture confirms the diagnosis of gonorrhea. Genital, rectal, and pha-ryngeal specimens are inoculated on a nonselective medium (e.g., blood agar or chocolate agar) and on a selective medium (e.g., Modified Thayer Martin medium).
The colonies of gonococci on chocolate agar after 48 hours of incubation at 35–36°C in the presence of 5–10% CO2 are small, round, translucent, and convex with finely granular surface. On Thayer Martin medium, the colonies show similar mor-phology as that on chocolate agar. The mixed microbial flora present in the clinical specimens is suppressed by the selective media. However, the vancomycin present in the selective media inhibits some strains of gonococci.
◗ Identification of bacteria
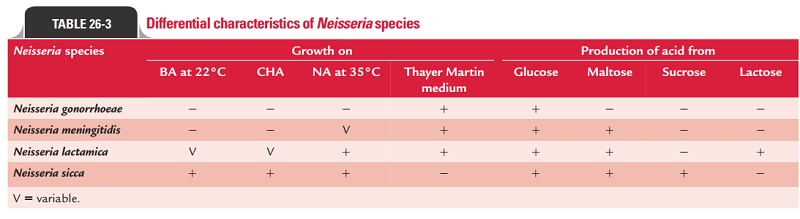
They are differentiated from N. meningitidis and otherNeisseria species by a variety of tests (Table 26-3).
◗ Detection of gonococcal antigen
The gonococcal antigens can be detected by both direct fluo-rescent antibody (DFA) test and direct enzyme-immunoassays (EIA) in urethral discharge and endocervical discharge as well as in other clinical specimens.
The DFA using fluorescein-conjugated monoclonal antibodies is a rapid and useful method for demonstration of gonococcal antigens in clinical specimens. The EIA using polyclonal antigonococcal antibodies are also used for the detection of gonococcal antigens in clinical specimens.
◗ Serodiagnosis
The serological tests are done to detect gonococcal antigens or specific anti-gonococcal antibodies in the serum for diagno-sis of gonorrhea. ELISA and RIA (radioimmunoassays) using whole cell lysates, pilus proteins, and LPS antigens of the gono-cocci demonstrate antibodies in the serum.
These serological tests are not recommended for routine use. These are used only in specific situations, such as chronic gonorrhea, gonococcal arthritis, etc.
Related Topics