Chapter: Clinical Anesthesiology: Clinical Pharmacology: Intravenous Anesthetics
Intravenous Anesthetics: Propofol
PROPOFOL
Mechanisms of Action
Propofol induction of general anesthesia
may involve facilitation of inhibitory neurotransmission mediated by GABA A receptor binding. Propofol allo-sterically
increases binding affinity of GABA for the GABAA
receptor. This receptor, as previously noted, is coupled to a chloride channel,
and activation of the receptor leads to hyperpolarization of the nerve
membrane. Propofol (like most general anesthetics) binds multiple ion channels
and receptors. Propofol actions are not reversed by the specific
benzodiaz-epine antagonist flumazenil.
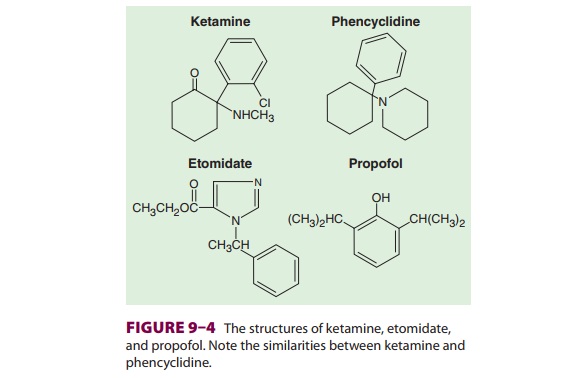
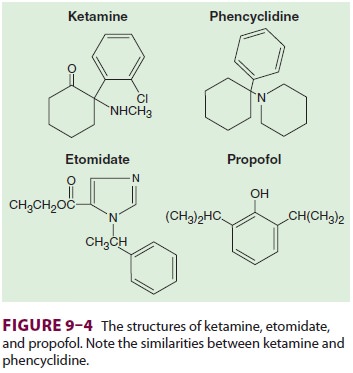
Structure–Activity Relationships
Propofol consists of a phenol ring
substituted with two isopropyl groups (see Figure 9–4). Propofol is not water
soluble, but a 1% aqueous solution (10 mg/mL) is available for intravenous
administration as an oil-in-water emulsion containing soybean oil, glycerol,
and egg lecithin. A history of egg allergy does not necessarily contraindicate
the use of pro-pofol because most egg allergies involve a reaction to egg white
(egg albumin), whereas egg lecithin is extracted from egg yolk. This
formulation will often cause pain during injection that can be decreased by
prior injection of lidocaine or less effectively by mixing lidocaine with
propofol prior to injection (2 mL of 1% lidocaine in 18 mL propofol). Propofol
formulations can support the growth of bacteria, so sterile technique must be
observed in preparation and handling. Propofol should be administered within 6
h of opening theampule. Sepsis and death have been linked to con-taminated
propofol preparations. Current formula-tions of propofol contain 0.005%
disodium edetate or 0.025% sodium metabisulfite to help retard the rate of
growth of microorganisms; however, these additives do not render the product
“antimicrobi-ally preserved” under United States Pharmacopeia standards.
Pharmacokinetics
A. Absorption
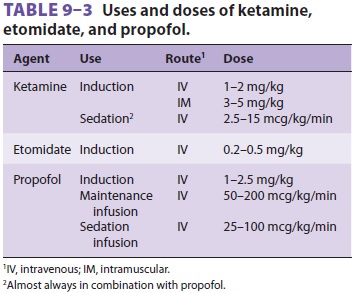
Propofol is available only for
intravenous adminis-tration for the induction of general anesthesia and for
moderate to deep sedation (see Table 9–3).
B. Distribution
Propofol has a rapid onset of action.
Awakening from a single bolus dose is also rapid due to a very short initial
distribution half-life (2–8 min). Most investigators believe that recovery from
propofol is more rapid and is accompanied by less “hangover” than recovery from
methohexital, thiopental, ket-amine, or etomidate. This makes it a good agent
for outpatient anesthesia. A smaller induction dose is recommended in elderly
patients because of their smaller Vd. Age is also a key factor determining required
propofol infusion rates for TIVA. In coun-tries other than the United States, a
device called the Diprifusor is often used to provide target (con-centration)
controlled infusion of propofol. The user must enter the patient’s age and
weight and the desired target concentration. The device uses these data, a
microcomputer, and standard phar-macokinetic parameters to continuously adjust
the infusion rate.
C. Biotransformation
The clearance of propofol exceeds hepatic
blood flow, implying the existence of extrahepatic metabo-lism. This
exceptionally high clearance rate probably contributes to relatively rapid
recovery after con-tinuous infusions. Conjugation in the liver results in
inactive metabolites that are eliminated by renal clearance. The
pharmacokinetics of propofol do not appear to be affected by obesity,
cirrhosis, or kidney failure. Use of propofol infusion for long-term seda-tion
of children who are critically ill or young adultneurosurgical patients has
been associated with spo-radic cases of lipemia, metabolic acidosis, and death,
the so-termed propofol infusion syndrome.
D. Excretion
Although metabolites of propofol are
primarily excreted in the urine, chronic kidney failure does not affect
clearance of the parent drug.
Effects on Organ Systems
A. Cardiovascular
The major cardiovascular effect of
propofol is a decrease in arterial blood pressure due to a drop in systemic
vascular resistance (inhibition of sympathetic vasoconstrictor activity),
preload, and cardiac con-tractility. Hypotension following induction is usually
reversed by the stimulation accompanying laryngos-copy and intubation. Factors
associated with propo-fol-induced hypotension include large doses, rapid
injection, and old age. Propofol markedly impairs the normal arterial
baroreflex response to hypotension. Rarely, a marked drop in preload may lead
to a vagally mediated reflex bradycardia. Changes in heart rate and cardiac
output are usually transient and insignificant in healthy patients but may be
severe in patients at the extremes of age, those receiving β-adrenergic
blockers, or those with impaired ventricular function. Although myocardial
oxygen consumption and coronary blood flow usually decrease comparably,
coronary sinus lac-tate production increases in some patients, indicating some
mismatch between myocardial oxygen supply and demand.
B. Respiratory
Propofol is a profound respiratory
depressant that usually causes apnea following an induction dose. Even when
used for conscious sedation in sub-anesthetic doses, propofol inhibits hypoxic
venti-latory drive and depresses the normal response to hypercarbia. As a
result, only properly educated and qualified personnel should administer
propofol for sedation. Propofol-induced depression of upper airway reflexes
exceeds that of thiopental, allowing intubation, endoscopy, or laryngeal mask
placement in the absence of neuromuscular blockade. Although propofol can cause
histamine release, induction with propofol is accompanied by a lower incidence
of wheezing in asthmatic and nonasthmatic patients compared with barbiturates
or etomidate.
C. Cerebral
Propofol decreases cerebral blood flow
and intracra-nial pressure. In patients with elevated intracranial pressure,
propofol can cause a critical reduction in CPP (<50 mm Hg) unless steps are taken to support mean
arterial blood pressure. Propofol and thiopen-tal probably provide a similar
degree of cerebral pro-tection during experimental focal ischemia. Unique to
propofol are its antipruritic properties. Its anti-emetic effects (requiring a
blood propofol concen-tration of 200 ng/mL) provide yet another reason for it
to be a preferred drug for outpatient anesthesia. Induction is occasionally
accompanied by excitatory phenomena such as muscle twitching, spontaneous
movement, opisthotonus, or hiccupping. Although these reactions may
occasionally mimic tonic–clonic seizures, propofol has anticonvulsant
properties and has been used successfully to terminate status epi-lepticus.
Propofol may be safely administered to epileptic patients. Propofol decreases
intraocular pressure. Tolerance does not develop after long-term propofol
infusions. Propofol is an uncommon agent of physical dependence or addiction;
however, both anesthesia personnel and medically untrained indi-viduals have
died while using propofol inappropri-ately to induce sleep in nonsurgical
settings.
Drug Interactions
Fentanyl and alfentanil concentrations
may be increased with concomitant administration of pro-pofol. Many clinicians
administer a small amount of midazolam (eg, 30 mcg/kg) prior to induction with
propofol; midazolam can reduce the required pro-pofol dose by more than 10%.
Related Topics